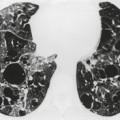
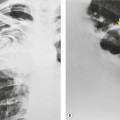
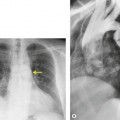
This chapter describes the normal anatomy of the airways, lungs, mediastinum, and diaphragm, as demonstrated on chest radiography (Fig. 2.1, Fig. 2.2 and Fig. 2.3), computed tomography (CT), and magnetic resonance imaging (MRI).
AIRWAYS AND LUNGS
Central airways
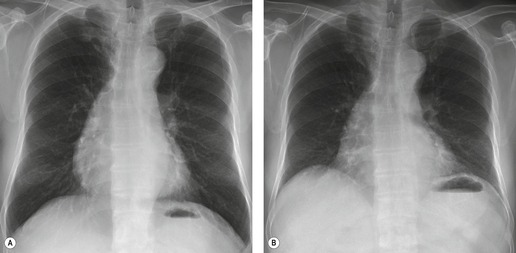
The trachea1. and 2. is a tube which, in children and young adults, passes downward and backward close to the midline (Fig. 2.4) and has sufficient flexibility to adapt to body position. In adults, the aorta may cause a recognizable impression and, in infants and young children, the brachiocephalic artery may indent the trachea. In older individuals, the intrathoracic trachea deviates slightly to the right to accommodate the left-sided arch. With unfolding and ectasia of the aorta, the trachea deviates more to the right as it descends into the chest and may also bow forward. In a CT study of 50 normal individuals, the midpoint of the trachea in the thorax lay between 1.6 cm to the right and 0.7 cm to the left of the midline. 3
The trachea has 16–20 incomplete C, U, or horseshoe-shaped cartilage rings which can give the trachea a corrugated outline. Calcification of the cartilage rings is a common normal finding after the age of 40 years, increasing in frequency with the age of the individual; 4 in one study, it was seen on CT in 50% of subjects in their seventh and eighth decades. 5 The incidence of visible tracheal calcification on chest radiography is very small; it was less than 1% in a series of 5000 inpatients, most of whom were women over 70 years. 6
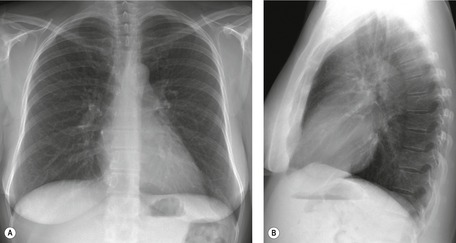
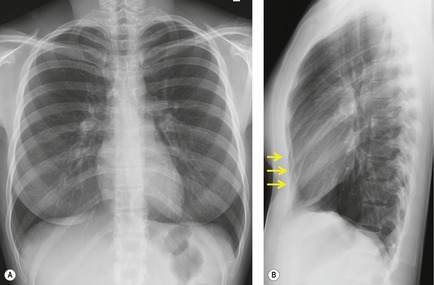
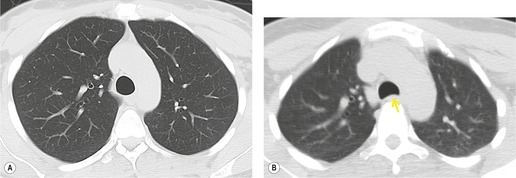
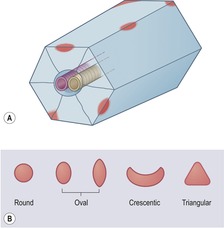
In cross-section, the trachea is usually round, oval, or oval with a flattened posterior margin, the posterior margin being formed by the fibromuscular membrane. It may occasionally show other configurations such as a square or inverted pear shape.4.7. and 8. The trachea enters the thorax 1–3 cm above the level of the suprasternal notch and the intrathoracic portion is 6–9 cm in length. 8 The range of tracheal diameters in adults on chest radiography in men is 13–25 mm in coronal plane, and 13–27 mm in sagittal plane; in women the diameters are 10–21 mm in coronal plane, and 10–23 mm in sagittal plane. 9 On CT, which allows precise assessment of diameters and cross-sectional areas without magnification, the mean transverse diameter is 15.2 mm (SD 1.4) for women and 18.2 mm (SD 1.2) for men, the lower limit of normal being 12.3 mm for women and 15.9 mm for men. 10 The diameters in the growing child and young adult have been documented by Griscom and Wohl. 11 In addition to sex and age differences, it is probable there are interracial differences in the diameter and configuration of the trachea. 12 Cross-sectional areas can also be measured: the mean is 194 mm2 (SD 35) in women and 272 mm2 (SD 33) in men. The normal cross-sectional area on forced expiration is considerably less than on full inspiration: in 10 normal male volunteers the cross-sectional area dropped from a mean of 280 mm2 (SD 50.5) at full inspiration to 178 mm2 (SD 40.2) at end-expiration. 13 The major change is forward movement or invagination of the posterior wall of the trachea, leading to a marked reduction in the anteroposterior diameter14.15.16.17. and 18. (Fig. 2.5).
The trachea divides into the two mainstem bronchi at the carina at approximately the level of T5. The left main bronchus extends up to twice as far as the right main bronchus before giving off its upper lobe division, the left main bronchus is approximately 50 mm long and the right main bronchus is approximately 25 mm long. In children the angles are symmetric, but in adults the right mainstem bronchus has a steeper angle than the left. The range of subcarinal angles is wide; 19 in one survey they varied between 35° and 90.5° (mean 60.8°, SD 11.8°). 20 Abnormalities of angle can, therefore, only be diagnosed by right–left comparisons, not by absolute measurement.
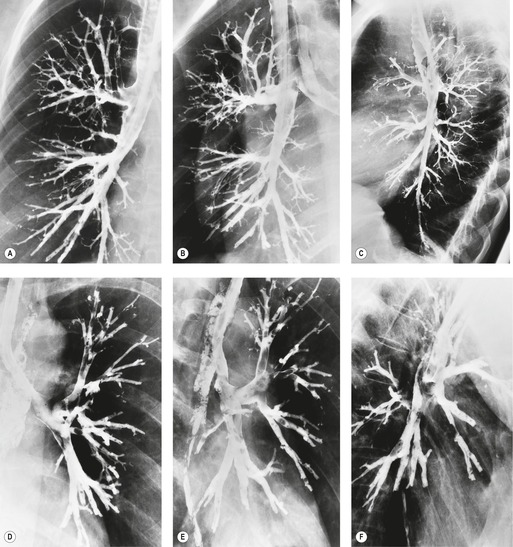
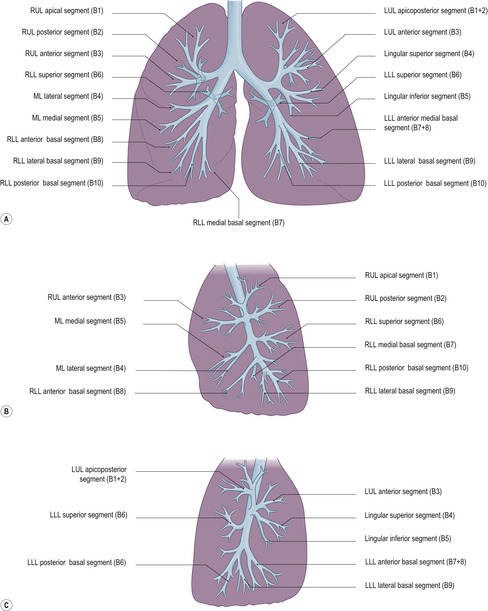
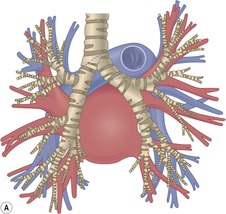
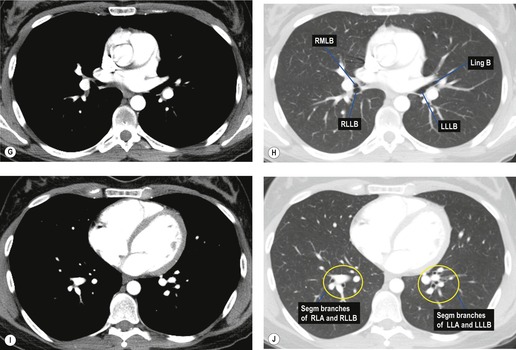
The lobar and segmental branching pattern is shown in Fig. 2.6 and the branching pattern of the airways beyond the segmental bronchi is shown diagrammatically in Fig. 2.7. The walls of the segmental bronchi are invisible on chest radiography except when seen end-on as ring shadows. They are, however, clearly seen on CT, particularly on thin contiguous sections. 21 The CT anatomy of central airways has been described in the literature.8.22.23. and 24. The reader is also referred to a number of detailed articles concerning the CT appearance of the segmental and subsegmental airways: upper lobes,25.26.27. and 28. lower lobes,29. and 30. and lingular segments. 25
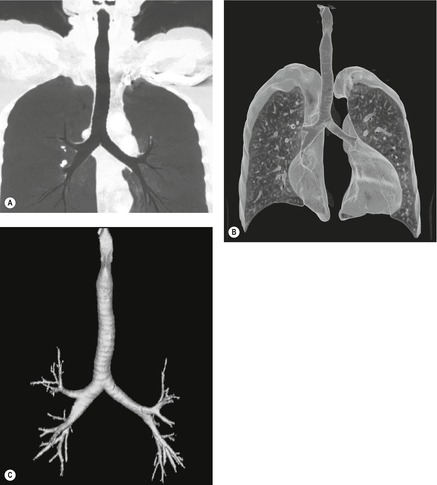
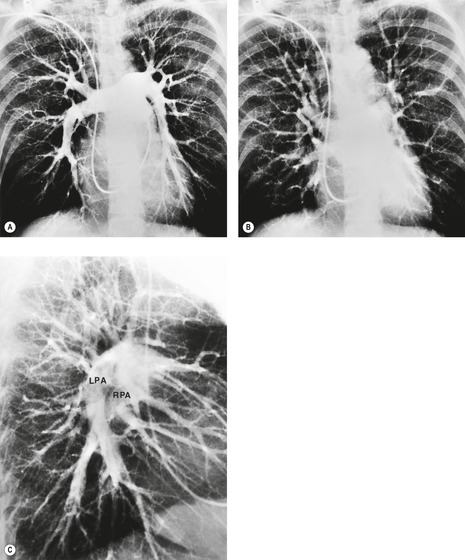
Variations in bronchial anatomy,31.32.33. and 34. particularly those affecting segmental and subsegmental airways, are fairly common, but are rarely clinically relevant (Fig. 2.8). However, they can be confusing to bronchoscopists searching for landmarks. There are two kinds of anomalous airways: (i) displaced, in which a standard airway arises from an unusual site; and (ii) supernumerary. Displaced airways are much commoner than supernumerary ones. Ghaye et al. 35 have written a detailed, illustrated review including an analysis of their experience of both types of variants on CT examination. Anomalous bronchi can be well shown by thin-section multidetector CT (MDCT) with three-dimensional reconstructions, or by MRI.33. and 36. The reported variations are:
• Tracheal bronchus, also known as bronchus suis, is an anomaly in which either a segment of the right upper lobe or the entire right upper lobe bronchus originates from the trachea rather than the main bronchus (Fig. 2.8). Tracheal bronchus is found in 0.5–3% of bronchoscopies.37. and 38. A tracheal bronchus arises from the lateral wall of the trachea,35.39. and 40. usually within a few centimeters of the mainstem take-off. It is much more common on the right side and is usually a displaced apical segmental bronchus, but it may be supernumerary supplying the apical segment, a displaced upper lobe airway, or even a supernumerary upper lobe airway. 41 When a tracheal bronchus is a displaced upper lobe airway, the more distal trachea is narrowed. 42 The anomaly is usually clinically inapparent, but occasionally the orifice is narrow41.43. and 44. or the airway is bronchiectatic,41. and 43. which may lead to recurrent distal pneumonia and abscess formation. Apical cyst formation in the lung supplied by a tracheal bronchus is also described. 45
• There may be a common origin of the right upper and middle lobe bronchi. 46
• An accessory cardiac bronchus is a supernumerary bronchus arising from the medial aspect of the right main bronchus or the bronchus intermedius proximal to the origin of the right superior (apical) segmental airway of the lower lobe. It usually passes downward and medially toward the heart, paralleling the bronchus intermedius. It is either blind-ending, in which case it may have a nodule of nonaerated lung tissue at its tip, or supplies a small ventilated ‘lobule’.47. and 48. Most patients are asymptomatic; however, an accessory cardiac bronchus may be associated with local infection49 or hemoptysis. Ghaye et al. 35 found a frequency of accessory cardiac bronchus of 0.08% in 17 500 consecutive patients. The diameter of the accessory bronchus ranged from 4 to 14 mm, and the length ranged from 4 to 23 mm. The simultaneous occurrence of an accessory cardiac and tracheal bronchus has been reported.48.50. and 51.
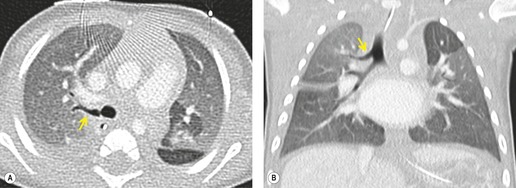
• Isolated cases of the so-called bridging bronchus have been described. 54 In this condition, the right lower lobe bronchus arises from the left main bronchus and crosses or ‘bridges’ the mediastinum to reach the right lung (Fig. 2.9). This anomaly is exceedingly rare.
 |
| Fig. 2.9 (Case courtesy of N L Müller, Vancouver, BC, Canada.) |
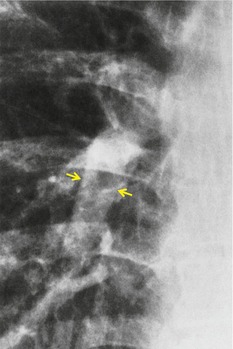
Pulmonary hila
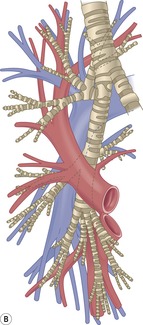
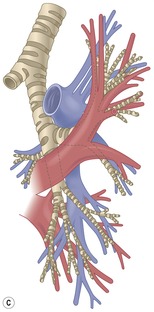
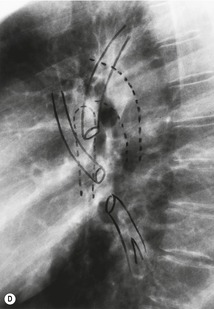
Understanding the appearances of the normal hila requires an appreciation of the anatomy of the major bronchi, hilar blood vessels (Figs 2.10 and 2.11),24.55.56. and 57. and hilar lymph nodes,58. and 59. and their relationship to one another on cross-sectional imaging (Fig. 2.12). Connective tissue does not contribute significantly to the bulk of the hila, and the small amount of fat between the vessels is, for practical purposes, visible only on CT and MRI. The following points of anatomy should be remembered:
• The right main bronchus has a more vertical course than the left main bronchus and the right upper lobe bronchus arises more proximally than the left upper lobe bronchus.
• The right mainstem bronchus and its divisions into the right upper lobe bronchus and bronchus intermedius are outlined posteriorly by lung so that the posterior wall of these portions of the bronchial tree is seen as a thin stripe on lateral chest radiographs (Fig. 2.13), except for a focal nodule, representing a small draining pulmonary vein in some 5% of normal subjects. 60 This region is, therefore, an important area in which to look for masses, such as lymphadenopathy. On the left side the lower lobe artery intervenes between the lung and the bronchial tree, and only a small tongue of lung can invaginate between the left lower lobe artery and the descending aorta to contact the posterior wall of the left mainstem bronchus (Fig. 2.12). 61
• The right pulmonary artery passes anterior to the major bronchi to reach the lateral aspect of the bronchus intermedius and right lower lobe bronchus, whereas the left pulmonary artery arches over the left main bronchus and left upper lobe bronchus to descend posterolateral to the left lower lobe bronchus.
• The pulmonary veins are similar on the two sides. The superior pulmonary veins are the anterior structures in the upper and mid-hilum on both sides, and the inferior pulmonary veins run obliquely forward beneath the divisions of each lower lobe artery to enter the left atrium. Because the central portions of the pulmonary arteries are so differently organized on the two sides, the relationship between the major veins and arteries differs. On the right, the superior pulmonary vein is separated from the central bronchi by the lower division of the right pulmonary artery, whereas on the left, the superior pulmonary vein is separated from the lower division of the left pulmonary artery by the bronchial tree.
• On chest radiographs, the transverse diameter of the lower lobe arteries prior to their segmental divisions can be measured with reasonable accuracy. These arteries should normally be 9–16 mm in diameter (Fig. 2.14). The large round shadow seen on lateral and oblique views of the right hilum is a combination of the right pulmonary artery and the superior pulmonary vein. The combined shadows of these two vessels may be sufficiently large to be confused with a mass.
• Normally there are no large vessels traversing the angle between the middle and the lower lobe bronchi on the right, or the angle between the upper and lower lobe bronchi on the left, on lateral or oblique plain chest radiographs. Therefore, a rounded shadow larger than 1 cm in either of these angles is likely to be a mass rather than a normal vessel. 62
• Normal hilar lymph nodes are not recognizable on chest radiography, but are identifiable on contrast-enhanced CT as triangular or linear soft tissue densities. 58 The normal range of size of hilar lymph nodes has not yet been fully established, but Remy-Jardin et al. 58 suggested a short-axis figure of up to 3 mm, except around the left lower lobe artery where the diameter may be somewhat larger in healthy individuals. The shape of the hila on CT is important when trying to assess the normality of lymph nodes. In normal subjects, the interfaces with the lungs are concave except at the sites of blood vessels. 59
• A collection of fat between the bifurcation of the right pulmonary artery as it exits the mediastinum, lying anterolateral to the bronchus intermedius, may be confused with lymphadenopathy if this anatomic variant is not recognized. 63 The major difficulty is that the fat in question may be combined in the same CT section as horizontal portions of the adjacent right pulmonary artery and appear to be of soft tissue rather than fat density, due to partial volume artifact.
Lung parenchyma
The segmental bronchi divide into progressively smaller airways until, after 6–20 divisions, they become bronchioles. The bronchioles divide, and the last of the purely conducting airways are known as the terminal bronchioles. Beyond the terminal bronchioles lie the acini, the gas-exchange units of the lung. The entire airway down to the terminal bronchiole can be demonstrated on a well-filled bronchogram.
The bronchopulmonary segments are based on the divisions of the bronchi and can be identified with reasonable accuracy by CT.23. and 27. The boundaries between segments are complex in shape; the segments have been likened to the pieces of a three-dimensional jigsaw puzzle. With the rare exception of accessory fissures, the segments are not delimited by septa. Although processes such as atelectasis, pneumonia, or edema may predominate in one segment or another, these processes never conform precisely to the whole of just one segment, since collateral air drift occurs from adjacent segments. In other words, it is unusual to see visible evidence of precise segmental boundaries.
The pulmonary blood vessels (Fig. 2.10) are responsible for the branching linear markings within the lungs. It is not possible to distinguish arteries from veins in the outer two-thirds of the lungs on chest radiography. More centrally, the orientation of the arteries and veins differs: the inferior pulmonary veins draining the lower lobes run more horizontally, and the lower lobe arteries more vertically. In the upper lobes, the arteries and veins show a similar gently curving vertical orientation, but the upper lobe veins (when not superimposed on the arteries) lie lateral to the arteries and can sometimes be traced to the main venous trunk, the superior pulmonary vein, even on chest radiographs.
The diameter of the blood vessels beyond the hilum varies according to the patient’s position. On films taken with the patient in the upright position, the diameter of both the arteries and veins increases gradually from apex to base; for comparisons of diameter to be valid, the measurements must be made equidistant from the hilum. These changes in vessel size correlate with physiologic studies of perfusion, which show that in an erect subject there is a gradation of blood flow increasing from apex to base, a difference that is less marked when supine. Although general statements regarding differences in regional blood vessel size can be made, meaningful measurements of individual peripheral pulmonary vessels are difficult to make on plain chest radiographs, since it is not possible to know whether the vessel being measured is an artery or a vein or what degree of magnification has been used. The following measurements are suggested for upright chest films:
• The artery and bronchus of the anterior segment of either or both upper lobes are frequently seen end-on. The diameter of the artery is usually slightly less than the diameter of the bronchus (4–5 mm). 60
• Woodring64 measured the visible bronchi and immediately adjacent arteries in the upper and lower half of the chest in upright patients and found that the artery/bronchus ratio was 0.85 (SD 0.15) for the upper zone and 1.34 (SD 0.25) for the lower zone.
• Vessels in the first anterior interspace should not exceed 3 mm in diameter. 65
The acinus, which is 5–6 mm in diameter, comprises respiratory bronchioles, alveolar ducts, and alveoli. Up to 24 acini are grouped together in secondary pulmonary lobules, each 1–3 cm in diameter, which in the lung periphery are separated by interlobular septa. When thickened by disease, these septa form so-called septal lines (Kerley B lines). The anatomy of the pulmonary lobule and the appearance of the normal pulmonary parenchyma on high-resolution CT (HRCT) is discussed in Chapter 4.
A rich network of lymphatics drains the lung and pleura. The subpleural lymphatic vessels are found just beneath the pleura, at the junction of the interlobular septa and pleura, where they interconnect with one another as well as with the lymphatic vessels in the interlobular septa. The lymph then flows to the hilum by way of lymphatic channels that run peribronchially and in the deep septa. The lymphatic network is radiographically invisible, but in certain conditions, such as when the lung is edematous or when the lymphatic channels are occluded by tumor, the thickened septa containing the dilated lymphatics may become visible.
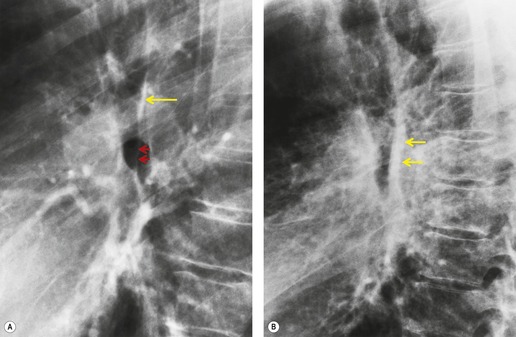
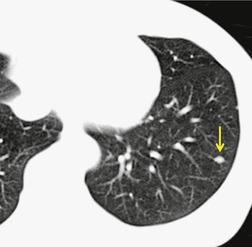
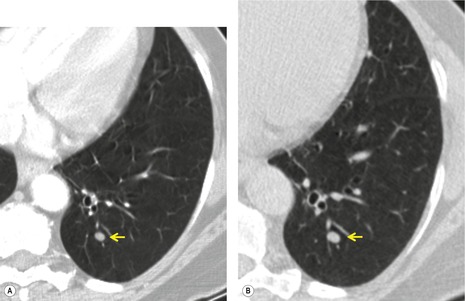
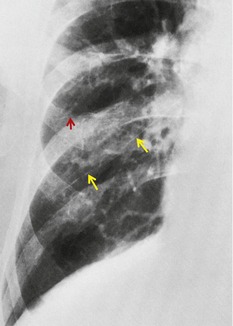
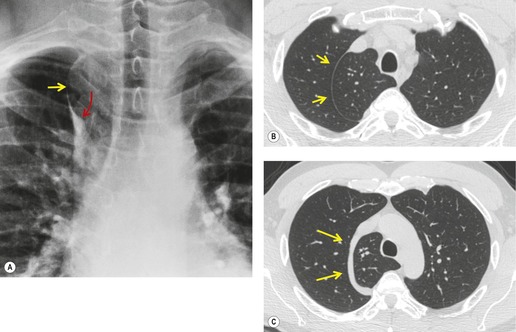
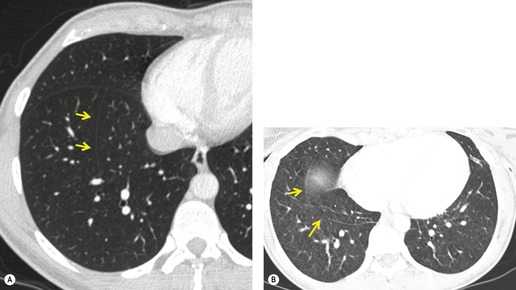
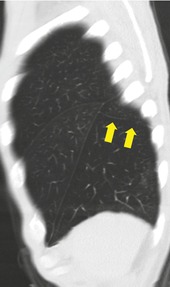
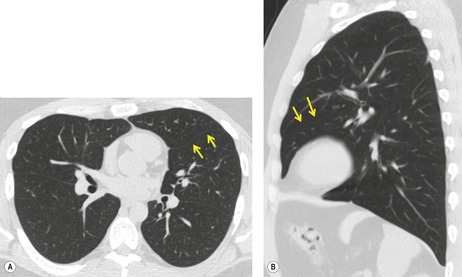
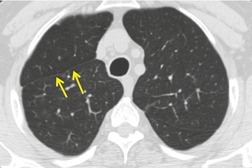
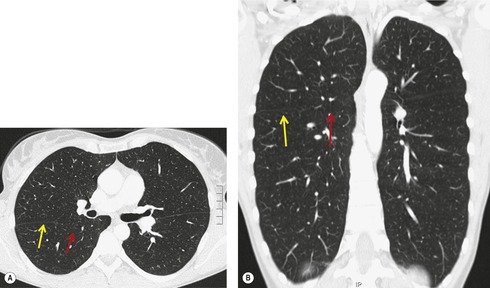
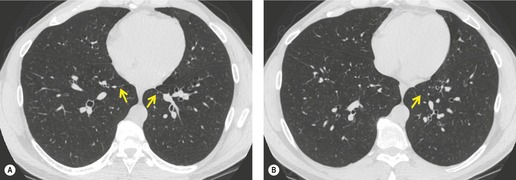
There are a few intrapulmonary lymph nodes, which are small and are not identifiable on plain chest radiographs. CT shows them as small, peripherally located, often coffeebean-shaped nodules (Fig. 2.15, Fig. 2.16, Fig. 2.17 and Fig. 2.18).66. and 67. In one series of 19 cases shown by CT, the intrapulmonary lymph nodes were either abutting the pleura or within 8 mm of the pleura, were round or oval in shape with homogeneous density and had well-defined borders, with the exception of one node which showed an irregular border resembling a small carcinoma. None of the nodes was larger than 12 mm. All were in the lower lobes or middle lobe/lingula. 68 The subpleural, lower lobe predominance of intrapulmonary lymph nodes, and the fact that one or two have an irregular outline indistinguishable from lung cancer on CT, has also been reported by others.69. and 70. Pathologically, intrapulmonary lymph nodes are believed to result from the presence of inorganic dust within the lungs and lymphatic obstruction. 71
The pleura
The pleural space is lined by a smooth membrane consisting of a single layer of flat, in part cuboidal, mesothelial cells, lubricated by a small amount of fluid. Inferiorly the parietal pleura is tucked into the costophrenic sulcus. The disposition of the sulcus is important in upper abdominal interventional procedures. On the surface of the body the inferior edge of the sulcus crosses the xiphoid and eighth costochondral junction to reach the midaxillary line at the level of the tenth rib.72. and 73. It then passes horizontally across the eleventh and twelfth ribs to reach the first lumbar vertebral body. The cephalad part of the sulcus is occupied to a variable extent by lung, whereas caudally the sulcus is empty and the diaphragm and chest wall are separated only by the two layers of parietal pleura. The distance between the lowest part of the sulcus and the lung edge depends on the phase of respiration and the segment of sulcus being considered. The right midaxillary intercostal approach is often used for percutaneous introduction of needles into the upper abdomen, and because the pleural reflection reaches the tenth rib in this region, it is common for the pleura to be punctured, for example, during percutaneous transhepatic biliary or subphrenic abscess drainage when bile or pus may flow into the pleural space.
The parietal mesothelial cells lie on loose, fat-containing, areolar connective tissue bounded externally by the endothoracic fascia. Five layers can be defined in the visceral pleura:74. and 75. (1) a mesothelial layer; (2) a thin layer of connective tissue; (3) a strong layer of connective tissue – the chief layer; (4) a vascular layer; and (5) the limiting lung membrane, connected by collagen and elastic fibers to the chief layer. 74
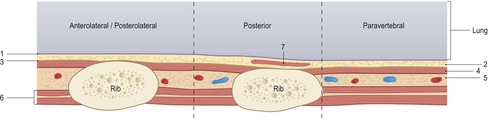
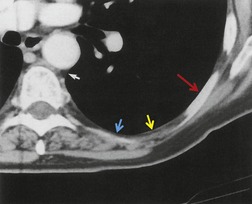
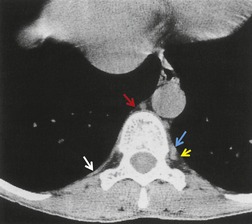
The normal pleura cannot be imaged as such by CT, even by HRCT, because it cannot be separated from immediately adjacent structures (Fig. 2.19). The CT appearances of the normal interface between chest wall and pulmonary parenchyma have been reported in detail by Im and co-workers. 76 In normal subjects, there is a linear opacity of soft tissue density, 1–2 mm thick, overlying an intercostal space, connecting the inner aspects of the ribs (Figs 2.20 and 2.21). This opacity, the intercostal stripe, is produced by two layers of pleura, extrapleural fat, the endothoracic fascia, and the innermost intercostal muscle. It is marginated centrally by air in the lung and peripherally by fat lying between the innermost and internal intercostal muscles. The intercostal stripe disappears on the inner aspect of ribs, since at this point it generally consists only of pleura, extrapleural fat, and endothoracic fascia, which are too thin to resolve. In some circumstances, however, it can be seen:
• Posteriorly, where the ribs are parallel to the scan plane and the CT section is through the lower tapering edge, the intercostal stripe is then seen on the inner aspect of the rib (Fig. 2.20).
• When there is significant fat between the parietal pleura and endothoracic fascia; this characteristically occurs laterally at the level of the fourth to eighth ribs, and in obese individuals may be conspicuous on the plain chest radiograph.
• Low in the parasternal and paravertebral region, poorly developed muscle slips (anteriorly the sternocostal muscle and posteriorly the subcostal muscle) lie on the inside of the ribs, producing linear, soft tissue opacities 1–2 mm thick (Fig. 2.19). The sternocostal muscle is commonly identified, but the subcostal muscle is seen less often (Fig. 2.21). These muscles are distinguished from pleural thickening by being smooth, uniform, and bilateral.
• Paravertebrally, intercostal muscles are absent and the lung–soft tissue interface is formed by a very thin line produced by two layers of pleura and the endothoracic fascia (Figs 2.19 and 2.20). Linear soft tissue opacities 2–3 mm thick lying immediately underneath this interface are produced by intercostal veins, which can be positively identified when they join the azygos or hemiazygos vein.
Fissures
The lobes of the lungs are separated by fissures, 77 which in the majority of people are incomplete. In other words, lung parenchyma, together with its bronchovascular bundles and draining veins, passes from one lobe to another through holes in the fissures.26.78. and 79. The frequency of incomplete fissures in different series ranges from 12.5% to 73% for the major fissures80 and from 60% to 90% for the minor fissures.81.82. and 83. These defects are important because they allow collateral air drift between lobes, permit disease to ‘cross’ fissures, and also limit the accumulation of pleural fluid in the interlobar portions of the pleural cavity.84.85. and 86.
The major fissures on each side are similar. The left major (oblique) fissure divides the left lung into an upper and lower lobe. The right lung has an additional fissure, the minor (horizontal) fissure, which separates the middle from the right upper lobe. The major fissures run obliquely forward and downward, passing through the hilum, commencing at approximately the level of the fifth thoracic vertebra to contact the diaphragm up to 3 cm behind the anterior chest wall. Portions of one or both major fissures are frequently seen on the lateral chest radiograph (Figs 2.22 and 2.23). It is, however, unusual to be able to trace both fissures in their entirety on chest radiographs.
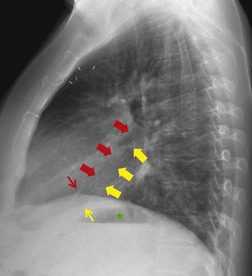
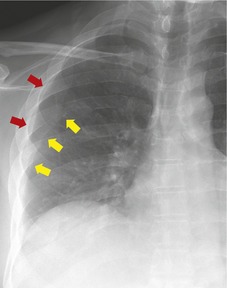
In Proto and Speckman’s study87 of lateral chest radiographs, part of a right fissure was seen in 22% of the images, part of a left fissure was seen in 14%, and part of a major fissure of indeterminate side was seen in 62%; in only 2% of radiographs was a complete major fissure identified. When the major fissure is incompletely seen, it is almost always the lower portion that is detected. Each major fissure follows a gently curving plane somewhat similar to that of a propeller blade, with the upper portion facing forward and laterally and the lower portion facing forward and medially. Below the hila the lateral portions of the major fissures lie further forward than do the medial portions, whereas above the hila this relationship reverses (Fig. 2.24). These undulations cannot be traced on the chest radiograph. Therefore, on a lateral view the radiologist cannot be certain what portion of the fissure is being profiled, and it is easy to misinterpret a fissure as displaced when it is in fact in normal position. The inferior few centimeters of either or both major fissures are often wide as a result of fat or pleural thickening between the leaves of the pleura. This thickening may lead to loss of silhouette where the fissure contacts the diaphragm.
The major fissure is not usually seen on a frontal radiograph, but it may be detected under three circumstances. First, the upper edge may become visible where it contacts the posterior chest wall when extrapleural fat enters the lips of the fissure. This generates the ‘superolateral major fissure’, a curved line or stripe that starts medially above the hilum and curves downward and laterally. 88 Second, the upper aspect of the major fissure can be tangential to the X-ray beam, particularly on lordotic projections, 89 generating a hairline opacity that runs obliquely across the mid-zone (Fig. 2.25). Medially, this fissure line often crosses the hilum to end against the spine, allowing it to be distinguished from the minor fissure, which never crosses hilar vessels. Third, reorientation of the lateral aspect of the lower part of the oblique fissure probably accounts for the vertical fissure,90.91. and 92. seen particularly on the right, low down close to the chest wall. It is most often described in babies with lower lobe volume loss and cardiomegaly. 90
The minor fissure fans out forward and laterally in a horizontal direction from the right hilum. On a standard upright frontal chest radiograph the minor fissure contacts the lateral chest wall at or near the axillary portion of the right sixth rib. The fissure curves gently, usually downward in the anterior and lateral portions. Because of the undulations of the major fissure the posterior portion of the minor fissure may be projected posterior to the right major fissure on a normal lateral view.
On frontal chest radiographs some or all of the minor fissure is seen in about 50–60% of patients. 93 The whole fissure is seen in only 7% of individuals. When just a portion is seen, it is much more commonly the lateral than the medial portion. Felson93 pointed out that on a frontal chest radiograph the fissure ends medially at the interlobar pulmonary artery within about 1 cm of the point at which the superior venous trunk crosses the lower lobe artery (Fig. 2.26). This observation can be helpful in finding and identifying the fissure. On a lateral view, the minor fissure is seen in about half of chest radiographs: in part in 44% and in total in 6%. 94
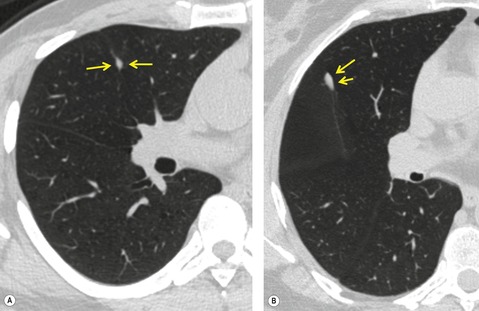
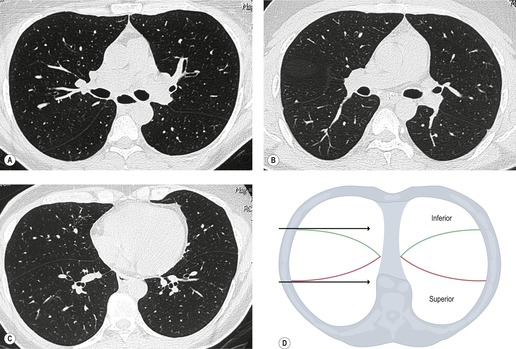
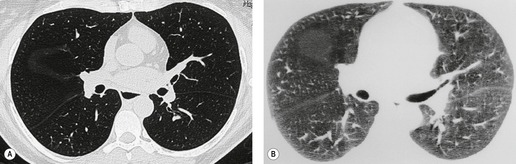
On 5–10 mm CT sections the position of the major fissures can usually be predicted by noting the relatively avascular zone that forms the outer cortex of the lobe.79.95. and 96. The region of the major fissures is seen as a band of avascularity, or a zone with much smaller vessels, traversing the lung. The major fissures may be seen as lines but, because they run obliquely through the sections, the fissure itself may be invisible or may be seen as a poorly defined band of density.79. and 97. With thin-section CT the left major fissure is seen as a line throughout its course in almost all subjects (see Fig. 2.24), but the line may not be visible in upper and middle portions of the right major fissure in up to a quarter of patients, presumably because the right major fissure is more obliquely oriented to the scanning plane. 79
The minor fissure is in the plane of section of the CT scanner, and therefore when in normal position it is not seen as a line in axial sections. Its position can usually be inferred from the large, triangular, or oval deficiency of vessels on one or more sections just above the level of the bronchus intermedius.96.98. and 99. With HRCT, a variety of normal patterns are encountered, depending on the precise shape of the minor fissure. 78 Because the fissure may assume the shape of an upward-arching dome, some portions may run sufficiently obliquely through the section to be seen as a line, an ill-defined band shadow or a rounded density (Fig. 2.27).78. and 99.
Accessory fissures
Accessory fissures are clefts of varying depth in the outer surface of the lung that delineate accessory lobes. In one CT study of 50 patients, 22% had some form of accessory fissure; 100 and in another study of 186 patients, 32% had an accessory fissure. 101 Four accessory fissures are either common or easily recognized:
• The best known accessory fissure, seen in up to 1% of the population, is the ‘azygos lobe fissure’ (Fig. 2.28), so-called because it contains the azygos vein within its lower margin. The fissure is almost invariably on the right side, although left-sided ‘azygos’ fissures have been described, in which case the vein at the base of the fissure is the superior intercostal vein. 102 The fissure results from failure of normal migration of the azygos vein from the chest wall through the upper lobe to its usual position in the tracheobronchial angle, so that the invaginated visceral and parietal pleurae persist to form a fissure in the lung. The altered course of the azygos vein together with the fissure is readily seen at CT. 103 Since there is no corresponding alteration in the segmental architecture of the lung, the term ‘lobe’ is a misnomer: the portion of the lung is supplied by branches of the apical segment bronchus with or without a contribution from the posterior segmental airway. 104 The ‘azygos lobe’ is not unduly susceptible to disease. A potential diagnostic pitfall is that the ‘azygos lobe’ may occupy less volume than the equivalent normal lung and may therefore appear relatively opaque, 105 even when no disease is present (Fig. 2.29). The right brachiocephalic vein may on rare occasion course through the anterior portion of the azygos fissure. 106
• The ‘inferior accessory fissure’ usually incompletely separates the medial basal segment from the rest of the lower lobe. Because this segment lies anteromedially in the lower lobe, the accessory fissure has components that are oriented both sagittally and coronally (Fig. 2.30) and are tangential to frontal and lateral X-ray beams, respectively; even so the fissure is rarely seen on lateral radiographs. The frequency of occurrence is difficult to ascertain because the fissure varies greatly in depth and prominence from one examination to the next. 100 The reported prevalence also depends on the method of detection. The fissure is present in 30–50% of anatomic specimens, 90 in 16–21% of CT scans,100. and 101. and in 5–10% of chest radiographs.90.100. and 107. On the frontal radiograph, the fissure is a hairline that arises from the medial aspect of the hemidiaphragm and ascends obliquely toward the hilum (Fig. 2.31). Sometimes there is a small triangular peak at its diaphragmatic end, and this, with a very short fissure line, may be all that is seen. At the other extreme the fissure may be long, reaching all the way to the hilum. 93 Although the left lower lobe lacks a separate medial basal segment, the anteromedial basal bronchus divides early into two components analogous to the medial and anterior segmental bronchi on the right, 100 and an inferior accessory fissure is about as common on the left as the right. However, it is not detected with equal frequency on radiographic examination; in one series of 500 radiographs 80% of inferior accessory fissures were right sided, 12% were left sided, and 7% were bilateral. 107 On the lateral radiograph the inferior accessory fissure is occasionally seen as a vertical line, often associated with a diaphragmatic peak in the region of the esophagus. 100 The inferior pulmonary ligament is close to the medial portion of the inferior accessory fissure, and some diaphragmatic peaks on the lateral radiograph in this region are really due to the inferior pulmonary ligament and its septum. On CT the fissure appears on sections near the diaphragm as an arc, concave to the mediastinum, extending from the major fissure back to the mediastinum near the esophagus.100. and 101. Should the inferior accessory fissure marginate a pneumonia in the medial basal segment, the triangular opacity has a sharp outer border, 108 which may mimic a collapsed lower lobe. Other lesions such as pleural effusion, mediastinal mass, hernia, or fat pad may be simulated. 100
• The ‘superior accessory fissure’ separates the superior (apical) segment of a lower lobe from the basal segments (Fig. 2.32) and superficially resembles a minor fissure on a frontal radiograph. It was identified on 6% of lateral radiographs in one series, 94 a figure that seems high when judged by general experience and CT series. 101 The minor fissure lies above the middle lobe bronchus, and the superior accessory fissure lies below the superior segmental bronchus. Because both of these airways arise at approximately the same level, the superior accessory fissure is projected below the minor fissure on frontal radiographs. On the lateral view it differs from the minor fissure in that it extends backward across the vertebral bodies. 94 The original descriptions of the superior accessory fissure suggested it was horizontal in orientation, but a recent evaluation of CT images suggests that it is often oriented obliquely, 109 travelling upward as it sweeps laterally and posteriorly from the hilum. On CT, like the minor fissure, it may appear as an avascular area, which should be distinguished from downward angulation of the upper end of the major fissure, a distinction that depends on identification of the superior segmental bronchus. 100 It may also be seen as a line or a boundary to atelectasis or pleural fluid, similar to the major fissures. 109
• The ‘left minor fissure’ is present in 8–18% of people but is only rarely detected on posteroanterior (PA) and lateral radiographs, with a reported frequency of 1.6%. 110 It separates the lingula from the rest of the left upper lobe and is analogous to the minor fissure. It is usually arched and located more cephalad than the minor fissure, and slopes medially and downward (Fig. 2.33).
Other rare accessory fissures include intersegmental fissures between the medial and lateral segments of the right middle lobe (Fig. 2.31), the superior and inferior segments of the lingula, the segments of the upper lobes (Fig. 2.34), and the anterobasal and laterobasal segments of both right and left lower lobes. 101
Incomplete fissures
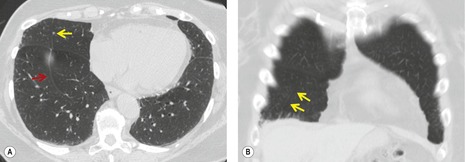
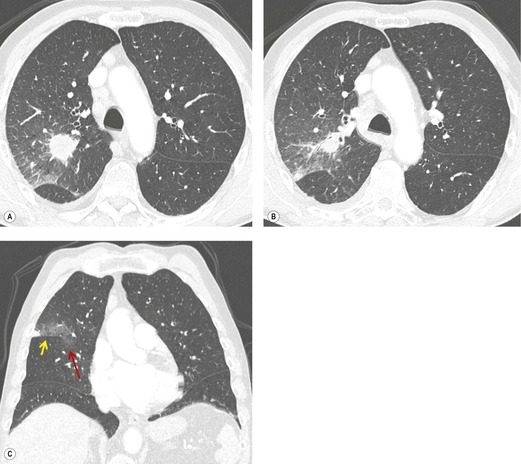
Not all pleural fissures are completely separated, and it is estimated that up to 73% of all fissures are in fact incomplete, i.e. that the pleural layers are not complete, such that the lung parenchyma of two neighboring lobes are in direct contact.111. and 112. These incomplete fissures, which are best seen on CT examinations (Fig. 2.35),111.112.113. and 114. are of clinical relevance in three circumstances:
• Unexpected distribution of effusion on chest radiographs: pleural fluid cannot freely distribute in the intrafissural space.
• Unexpected ventilation of a given lobe, despite a central airways obstruction: there is no anatomic barrier and collateral ventilation, therefore, allows unhindered exchange of gas between anatomically different lobes (also relevant in endobronchial valve placement for the treatment of severe emphysema).
• Unexpected spread of disease: absence of parts of a given fissure allows unhindered spread of disease, most commonly tumor or infection, from one lobe to another (Fig. 2.36).
(Inferior) pulmonary ligaments
The (inferior) pulmonary ligaments consist of a double sheet of pleura that hangs down from each hilum like a curtain and joins the lungs to the mediastinum and to the medial part of the hemidiaphragms. 115
The two layers of pleura contact each other below the inferior pulmonary vein and end in a free border that usually lies over the inner third of the hemidiaphragm but is sometimes displaced toward the hilum. The right inferior pulmonary ligament is short and wide based and is related on its mediastinal aspect to the azygos vein. On the left the ligament is longer and attaches to the mediastinum close to the esophagus and anterior to the aorta (Fig. 2.37). 115 The ligament overlies a septum within the lung that separates posterior and medial basal segments. 116 The bare area of the ligament contains connective tissue, small systemic vessels, lymphatics, and lymph nodes. 117
The ligament is not visible on chest radiographs. On CT it is visible in about 50–75% of patients (Fig. 2.37).116.118. and 119. It is best detected just above the diaphragm as a thin curvilinear line passing outward and slightly backward from the mediastinum at the level of the esophagus. There is strong evidence that this line represents an intrapulmonary septum associated with the ligament rather than the ligament itself.116.120. and 121. Often a small, triangular elevation is present at the mediastinal base of the ligament. The ligament and variations in its degree of development have been considered important for the following reasons:
• The ligament determines the shape of a collapsed lower lobe.
• The ligament determines the ultimate shape of the collapsed lung in a pneumothorax. 122
• Pleural effusion collecting posterior to the ligament tends to produce a triangular opacity, not unlike a lower lobe collapse. 122
• The juxtaphrenic peak sign described with volume loss of an upper lobe may be due to diaphragmatic traction by way of the ligament and septum.
• The ligament provides a pathway from lung to mediastinum and allows pathologic processes to travel in either direction.
MEDIASTINUM
The mediastinum is divided by anatomists into superior, anterior, middle, and posterior divisions. The exact anatomic boundaries between these divisions are unimportant to the radiologist because these boundaries neither provide a clear-cut guide to disease nor form barriers to the spread of disease. Moreover, almost every writer on the subject seems to have a different definition.81.117.123. and 124.
The mediastinal structures and spaces as seen on CT and MRI are described before the appearances on plain film because the complex interfaces between the mediastinum and the lungs are best understood by careful correlation with cross-sectional images.
Normal mediastinum
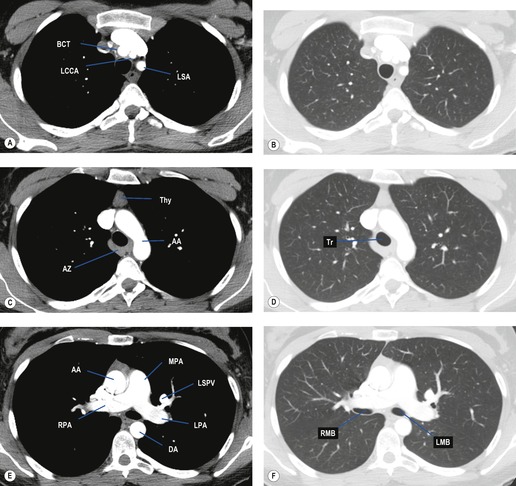
The normal mediastinal structures always identified at CT (Fig. 2.12) and MRI are the heart and blood vessels, which make up the bulk of the mediastinum; the major airways; and the esophagus. These structures are surrounded by a variable amount of connective tissue, largely fat, within which lie lymph nodes, the thymus, the thoracic duct, and the phrenic and laryngeal nerves.
Mediastinal blood vessels
On transverse CT images the vertically oriented ascending and descending portions of the aorta appear round, whereas the arch is seen as a tapering oval that becomes narrower as it gives rise to the arteries to the neck, head, and arms. The average diameter of the ascending aorta is 3.5 cm, and that of the descending aorta is 2.5 cm. 125 Sections above the aortic arch show the three major aortic branches arranged in a curve lying anterior and to the left of the trachea. Their order from right to left is the brachiocephalic (innominate), left common carotid, and left subclavian arteries. The brachiocephalic artery is appreciably larger than the other two vessels. It varies slightly in position: in about half the population it is directly anterior to the trachea, and in the remainder, although still anterior to the trachea, it is either slightly to the right or left of the midline. 126 The left common carotid artery lies to the left of the trachea; the left subclavian artery also lies either to the left of the trachea or posterior to it. It is the most lateral vessel of the three and often contacts the left lung.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree