26 Fractures and Dislocations of the Fingers
Among fractures of the fingers, extra-articular and intra-articular forms are differentiated, as well as avulsion fractures. Tension from the attached tendons and ligaments results in a characteristic pattern of dislocation. Avulsion fractures are often not very impressive on radiographs, but are of functional importance. Further diagnostic examinations are often necessary for fractures and fracture-dislocations of the finger joints for precise determination of the fracture extent and the number and dislocation of the fragments. These examinations include oblique radiographic views, magnified radiographs, and high-resolution computed tomography (CT) with sagittal source images and multiplanar reconstructed (MPR) or three-dimensional (3D) images. Nonosseous injuries of the collateral ligaments and the palmar plate are shown best with magnetic resonance imaging (MRI).
Pathoanatomy and Clinical Symptoms
Fractures and dislocations of the finger are generally the result of external force, such as an occupational or sports injury or a fight. Less common endogenous causes of spontaneous fractures are bone tumors, such as enchondromas. Clinical symptoms are pain, loss of function, and, if there is a dislocation, deformity, and eventually even abnormal mobility of the finger.
Diagnostic Imaging
Radiography
The following principles apply in regard to fractures or dislocations of the fingers:
Even in emergency cases, both radiographic views should be absolutely orthogonal to each other. The lateral view of the finger is correctly aligned when the two condyles of the phalanged head of interest overlap and the joint space is not overlapped (see 1.7e,f).
Nondisplaced fractures are sometimes visible only in magnified radiographs using a fine-focus tube.
If an intra-articular fracture is suspected, the central beam must be directed on the affected joint.
Rotational deformity of a finger can only be diagnosed clinically, but not radiographically.
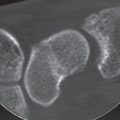
In individual cases, articular fragments and the extent of their dislocation can only be sufficiently identified in oblique radiographic views ( Fig. 26.1 ).
After reduction of a finger dislocation, a follow-up radiograph should always be taken to identify articular fragmentsthat were not seen originally.
Computed Tomography
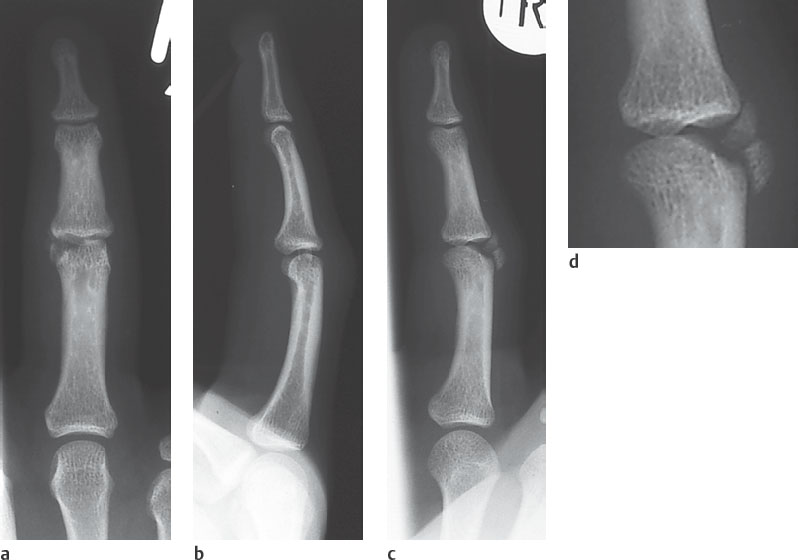
CT is indicated for intra-articular finger fractures when complex joint destruction is known or suspected. CT imaging is required for planning a surgical procedure on a comminuted fracture of a finger joint.
In spiral CT technique, the precise lateral orientation of the source images parallel to the longitudinal axis of the affected finger is mandatory. During the examination the patient is standing next to the CT gantry, and positioning is done with a light-beam localizer, for which the patient must perform maximal ulnar or radial inclination. A slice thickness of 0.5, 0.75, or 1.0mm is selected. After image computation with an overlapping increment, secondary reconstructions are performed with coronal multiplanar reconstruction (MPR) and three-dimensional (3D) surface-shaded display (SSD) or the volume-rendering technique (VRT). In the 3D image, electronic exarticulation of the joint is useful to obtain an unobstructed view of the fracture zone (Fig. 26.3c).
Magnetic Resonance Imaging
MRI is performed after a finger trauma when a fracture has been excluded but injuries to the collateral ligaments and palmar plate need clarification. For this purpose, MRI evaluation is performed in the subacute as well as in the chronic stage of the finger injury.
Slice of 2 mm thickness in the three standard spatial planes are acquired with a dedicated surface coil. If the signal-to-noise ratio is acceptable, 1.5 mm slices are preferable. Intravenous administration of a contrast agent is essential. Ruptures of the finger ligaments (see Fig. 29.18 ) and the palmar plate ( Fig. 26.8 ) can be sufficiently identified and their extent determined with contrast-enhanced MRI based on the enhancement of fibrovascular regeneration tissue.
Fracture Types
The trauma patterns listed in Table 26.1 are categorized according to treatment principles and prognoses.
Extra-articular Fractures
Fractures of the Tuberosity of the Distal Phalanx
Fractures of the tuberosity of the distal phalanx are caused by direct traumas (e.g., blows, crushes). Regardless of the fracture pattern, they are generally unimportant in regard to posttraumatic consequences. Therapy consists of pain control and release of subungual hematoma.
Fractures of the Finger Shafts
Fractures are categorized as transverse, oblique, spiral, longitudinal, and comminuted. In nondisplaced fractures, only a hair-thin interruption in the cortical and/or trabecular bone can be seen. Displaced fractures also exhibit a step deformity in the cortical contour, impaction of the trabecular bone, and different degrees of fragment dislocation. As a result of pull from the flexor and extensor tendons, palmar or dorsal malalignment predominates and can be easily recognized in lateral radiographic views.
Intra-articular Finger Fractures
These generally result from axial force. Longitudinal force vectors cause either a proximal burst fracture of the head of the phalanx near the median line or, more often, a distal impacted fracture of the base of the phalanx.
The following points must be considered in radiographic diagnosis:
A centrally impacted fracture leads to interruption of the subchondral bone plate in the dorsopalmar projection (Fig. 26.1a).
As a result of a displaced fracture of the head of a phalanx, the two finger condyles do not overlap as they normally do in a lateral view(Fig. 26.1b). In a correctly exposed radiograph, any deviation of a condyle is a direct sign of fracture. In such a situation, the next step is to take a complementary oblique view, which can often provide all the necessary information concerning the extent of the trauma (Fig. 26.1c,d and Fig. 26.2 ).
As already mentioned in this chapter, CT is indicated for planning reconstructive surgery on a complex articular fracture to determine the number of fragments, their dislocation, and the extent of the impaction in the joint surface without overlapping ( Fig. 26.3 ).
A further indication for high-resolution CT is a persisting posttraumatic deficit in flexion or extension when an intrarticular loose body is suspected and an injury of the tendons has been excluded ( Fig. 26.4 ).


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree