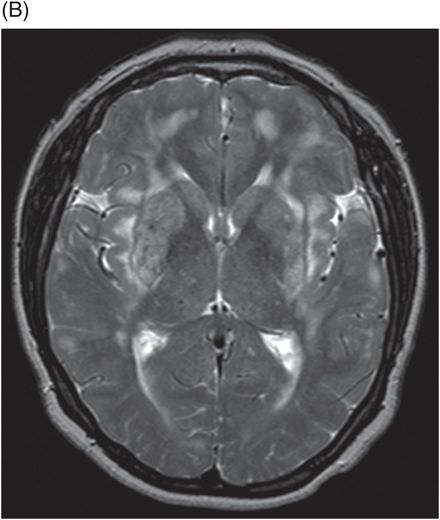
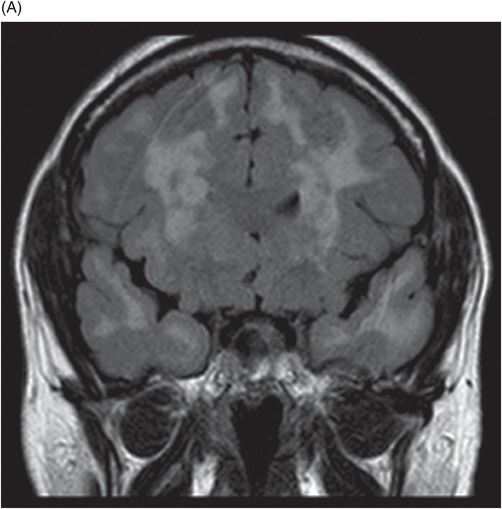
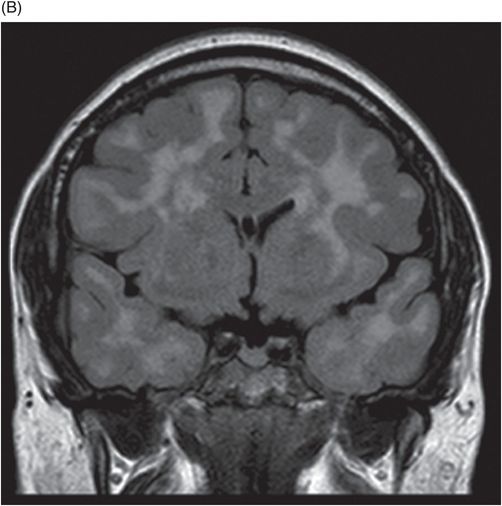
(A) Coronal FLAIR images at the level of frontal horns, anterior temporal lobes, and (B) body of lateral ventricles.
Cerebral Autosomal Dominant Arteriopathy with Subcortical Infarcts and Leukoencephalopathy (CADASIL)
Primary Diagnosis
Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL)
Differential Diagnoses
Multiple early age infarcts from a hypercoagulable state
Mitochondrial encephalopathy with lactic acidosis and stroke-like episodes (MELAS)
Primary angiitis of the CNS
Sporadic subcortical arteriosclerotic encephalopathy (SSAE)
Imaging Findings
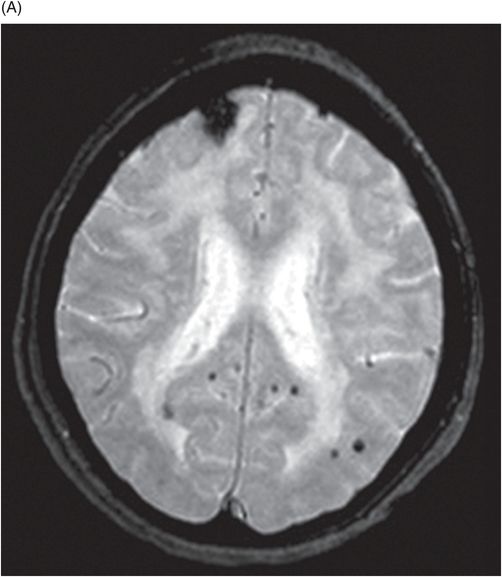
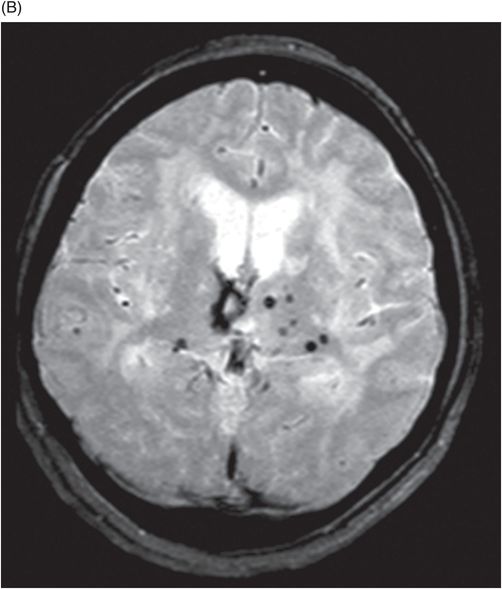
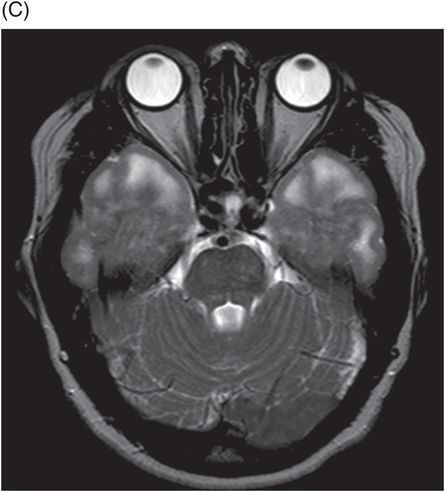
Fig. 27.1: (A) Axial T2WI showed confluent hyperintense signal changes in both cerebral hemispheres involving the frontoparietal white matter and central deep white matter. (B) Similar changes were also noted in the bilateral periventricular white matter and external capsules, and (C) anterior temporal white matter. Fig. 27.2: Coronal FLAIR images (A) at the level of frontal horns and (B) body of lateral ventricles depicted similar hyperintense signal changes in the periventricular, deep white matter, and anterior temporal regions. Fig. 27.3: (A) Axial GRE image at the level of lateral ventricles and (B) corona radiata demonstrated multiple discrete foci of T2 shortening/blooming representing microhemorrhages in the deep white mater, biparietal and right frontal subcortical white matter, and thalami.
Discussion
In a young, non-diabetic, non-hypertensive patient without any risk factors for atherosclerotic disease, the typical clinical presentation of migraine with aura combined with a history of multiple TIAs in different arterial distributions is highly concerning for CADASIL. Characteristic multi-arterial distribution of infarcts, extensive white matter small vessel ischemic changes, including the anterior temporal pole and subcortical lacunar cyst in the temporal lobe, are consistent with CADASIL. This diagnosis was confirmed with genetic testing for mutation in the NOTCH3 gene.
CADASIL can be differentiated from multiple early infarcts secondary to a hypercoagulable state, first by laboratory evaluation, which shows a deficiency in antiphospholipid antibodies and protein S in the latter. They also often present in young and middle-aged adults with stroke, but often have a history of recurrent arterial and venous thrombosis, spontaneous abortions, and thrombocytopenia. The lesions are often cortically based, as opposed to subcortical with CADASIL, and angiography shows findings similar to vasculitis and stenosis at the great vessel origins. Differential considerations also include MELAS, which often show bilateral, multifocal cortical and subcortical hyperintense lesions on FLAIR that resolve with clinical improvement.
Primary angiitis of the CNS shows lumen irregularities in the distal cerebral arteries on digital subtraction angiogram, which is normal in CADASIL. Sporadic subcortical arteriosclerotic encephalopathy is clinically associated with hypertension. Imaging in SSAE reveals lacunar infarcts in lenticular nuclei, pons, thalamus, internal capsule, and caudate nuclei. There is often diffuse confluent periventricular white matter involvement and it is uncommon to have temporal white matter lesions, as is classically seen in CADASIL. Lesions do not extend into the arcuate fibers of the temporal or paramedian superior frontal lobes. Susac syndrome also presents with similar features to CADASIL; however, it most often manifests as multiple, small typically supratentorial lesions with a predilection for the corpus callosum. CADASIL can be differentiated by its hereditary nature and demonstration of juxtafoveal telangiectasis on fundus examination.
CADASIL is an autosomal dominant trait causing characteristic subcortical lacunar infarcts and leukoencephalopathy in young/middle-aged adults, typically in the absence of traditional risk factors. Its prevalence is unknown, with over 500 families described worldwide in the literature. Transient ischemic attacks or strokes are the most common presenting disease manifestation, occurring in 60–85% of patients. Patients also present with migraines with auras (20–40%), cognitive deficits mostly related to executive dysfunction in memory and attention (90%), behavioral problems (75%), and seizures (5–10%). The average age of onset of imaging findings is 30 years of age, which precedes stroke/TIA by approximately 10–15 years. The average age of stroke onset is slightly earlier for men than women (50.7 years versus 52.5 years).
CADASIL is a small vessel disease, resulting from a mutation in the NOTCH3 gene on chromosome 19q12. Histologically, an angiopathy of small and middle-sized arteries, predominantly the penetrating cerebral and leptomeningeal vessels, is characteristic, without amyloid deposition or atherosclerosis. Genetic identification of the mutated gene is required for diagnosis.
Computed tomography findings are non-specific, demonstrating multiple non-enhancing, subcortical and basal ganglia regions of low attenuation. Magnetic resonance imaging is the investigation of choice and on T1WI images, two types of lesions are encountered – large, coalescent, isointense white matter lesions, and small, well-delineated, hypointense lesions, which spare the cortex. The total T1 lesion volume correlates significantly with the degree of disability and neuropsychologic impairment. On T2-weighted MR images, diffuse white matter hyperintensities are found early in the disease. Other findings include focal subcortical lacunar infarcts and prominent perivascular spaces. FLAIR findings are akin to T2 findings. Diffusion-weighted imaging shows restricted diffusion in acute lacunar infarcts. Perfusion studies show reduced CBF and volume in areas of white matter signal abnormality without significant mean transit time changes.
Classically, although the subcortical white matter can be diffusely involved, the frontal lobe (93%), temporal lobe (86%), and subinsular white matter (93%) are most commonly involved. Younger patients typically show frontal lobe, parietal lobe, external capsule, and anterior temporal lobe involvement, while older patients show additional findings in the posterior temporal and occipital lobes. Anterior temporal pole and paramedian superior frontal lobe findings are highly sensitive and specific to CADASIL. The orbitofrontal subcortical white matter, U fibers, and cerebral cortex are typically spared. Cerebral microhemorrhages occur in 25–70% of cases without a characteristic distribution.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree