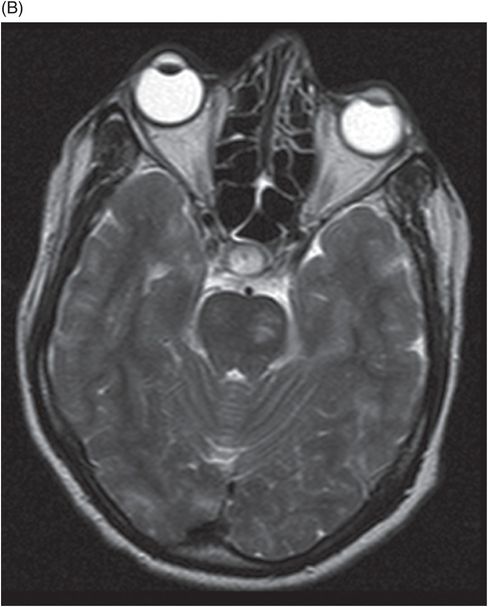
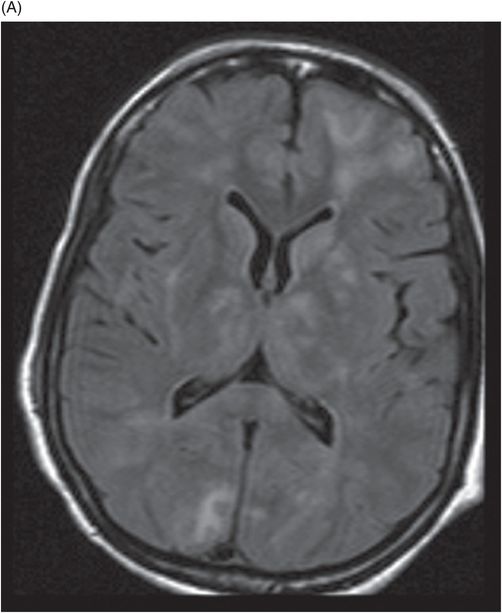
(A) Axial FLAIR image at the level of lateral ventricles and deep gray nuclei. (B) Axial FLAIR image at the level of midbrain and anterior temporal horns.
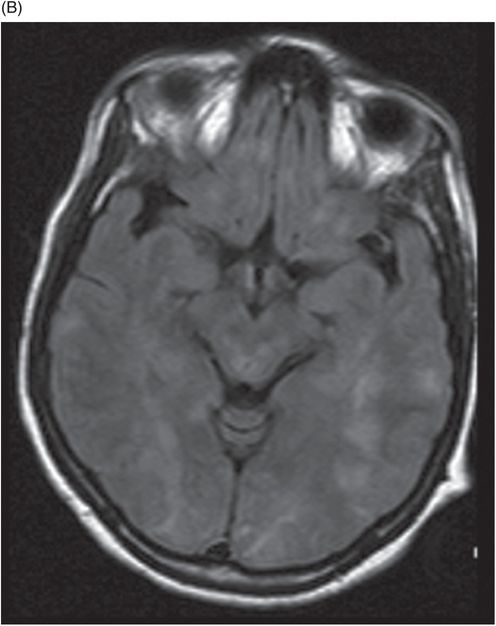
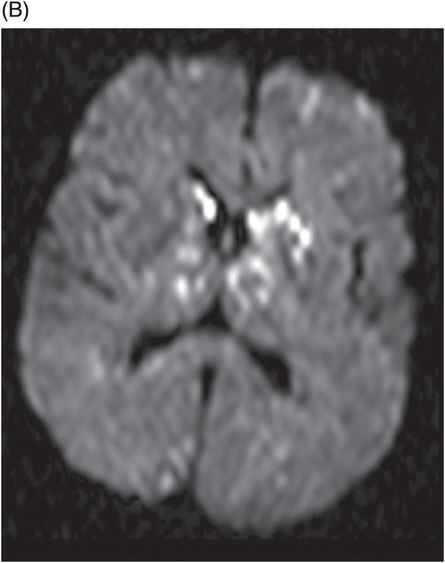
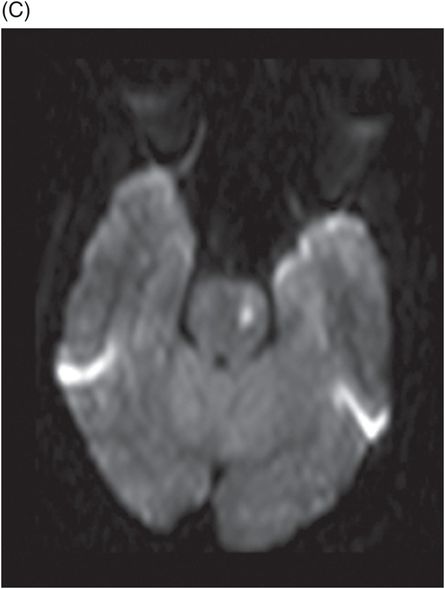
(A) and (B) Axial DWI at the level of corona radiata and deep gray nuclei and (C) Axial DWI at the level of midbrain.
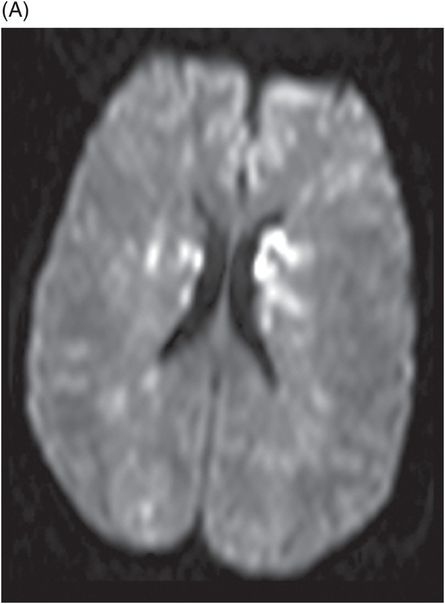
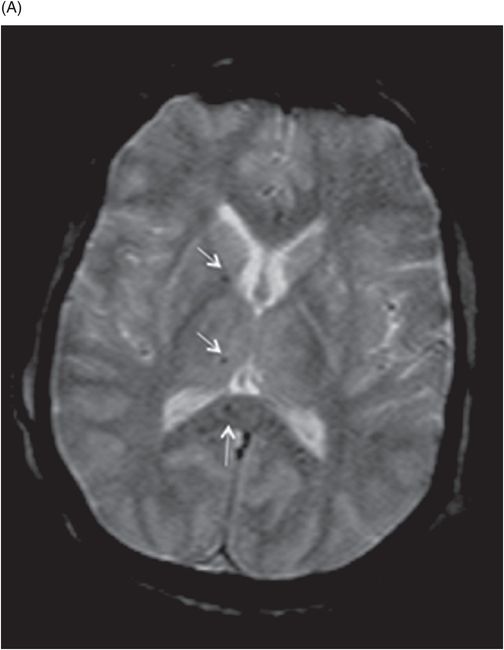
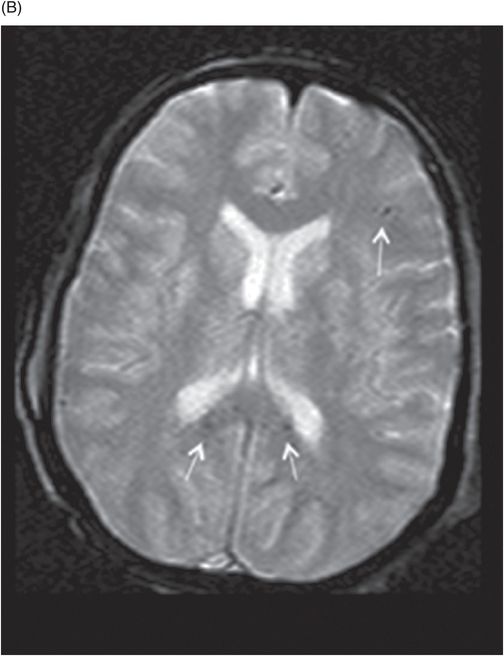
(A–B) Axial GRE images at the level of lateral ventricles, corona radiata, and deep gray nuclei.
Cerebral Fat Embolism
Primary Diagnosis
Cerebral fat embolism
Differential Diagnoses
Diffuse axonal injury
Cardioembolic stroke
Infective endocarditis
Venous thromboembolism with patent foramen ovale
Imaging Findings
Fig. 30.1:(A–B) T2WI of the brain showed discrete and confluent areas of high signal. Fig. 30.2: FLAIR sequence showed similar discrete and confluent areas of high signal in the subcortical regions, deep gray nuclei, midbrain, and corpus callosum. Fig. 30.3: (A–C) Axial DWI of the brain showed confluent heterogeneous foci of diffusion restriction in the bilateral corona radiata, deep gray nuclei, and left side of midbrain. Fig. 30.4: (A–B) Axial GRE images of the brain demonstrated multiple punctate foci of microhemorrhages (arrows) in the bilateral deep gray nuclei, corpus callosum, corona radiata, and few foci in the subcortical white matter.
Discussion
In approximately half of the patients with severe head trauma, diffuse axonal injury (DAI) is the suggested primary diagnosis, accompanied by an altered level of consciousness at the onset of injury. Contrary to that, like our patient, individuals with cerebral fat embolism experience a period of normal mentation followed by development of confusion and other neurologic symptoms, commonly after manipulation of long bone fractures. Lesions from DAI typically involve the gray-white matter interface with coarse hemorrhages. In contrast, lesions from cerebral fat embolisms mainly involve the white and deep gray matter with evidence of extensive vasogenic edema. Small punctate hemorrhages suggest fat embolism. However, corpus callosum involvement in DAI and fat embolism is similar. Cardioembolic shower and venous thromboembolism with patent foramen ovale may have a very similar pattern with deep watershed infarcts and hemorrhages. However, echocardiogram, CT pulmonary angiogram, and venous Doppler are helpful in differentiating these conditions from presence of fat embolism.
Fat embolism is a clinical entity consisting of respiratory, CNS, and cutaneous manifestations following long bone fractures. It is likely related to the release of fat emboli into mainstream circulation. It is an uncommon but potentially life-threatening condition. Though technically fat emboli can occur in every patient following long bone fractures, a clinical syndrome of fat embolism is seen in only 0.5–3% of patients with long bone fracture. Hypoxia, deteriorating mental status and petechial skin rash are the main diagnostic criteria. The pathogenesis by which fat emboli can cross from pulmonary to systemic circulation remains controversial. Small-sized fat droplets may pass through the lungs and reach the systemic circulation directly. The most common organs affected are the brain and kidneys. On a clinical spectrum, manifestation of cerebral fat emboli is highly variable and includes non-specific headache and lethargy on one end and convulsions, delirium, and coma on the other end. Fat embolism should be suspected in all cases of traumatic long bone injuries with development of altered mental status after a period of normal neurologic function.
The physiologic response cascade to fat emboli is likely due to the toxic effect of locally released free fatty acids from the fat emboli. Mechanical occlusion of cerebral blood vessels may cause ischemic lesions. The combination of infarction and diffuse cerebral blood-brain barrier breakdown due to toxicity is implicated in the pathophysiology of brain injury. Autopsy studies show that hemorrhage is common in severe cases. However, hemorrhages are less common in patients who recover. Almost complete reversal of MRI changes seen in the acute phases is expected, most patients have complete recovery and a good long-term prognosis.
The brain CT results are usually normal; however, they may show diffuse edema and hemorrhage in more severe cases. Magnetic resonance imaging is more sensitive in diagnosing and assessing lesion load. However, MRI remains non-specific and although T2 lesion load correlates with initial severity, this is not predictive of final neurologic outcome. The high-signal T2 lesions are typically multiple, small, non-confluent lesions situated within the cerebral white matter and deep gray matter. This pattern has been described as a star field pattern. Lesions are uncommon in the gray-white matter interface. T2-weighted high-signal lesions may take several days to develop and DWI may be more sensitive in the hyperacute phase. Lesions demonstrated on DWI are mostly non-restricted and suggest reversible vasogenic edema. However, DWI lesions with restricted diffusion suggest infarction and are more likely to result in permanent MR imaging and pathologic changes, such as cyst formation and gliosis. Restricted DWI lesions are associated with poor prognosis and long-term disabilities. Enhancement following gadolinium injection has been described in a few cases. Petechial hemorrhages can be seen early and may continue to be present in acute, subacute, and late stages. These hemorrhagic spots may be in a separate area from the T2-weighted abnormality. The lesions are mostly seen in the white matter and not at the gray-white matter interface or corpus callosum, as seen in DAI. This pattern of punctate microhemorrhages within the deep white matter could be a pathognomonic feature of cerebral fat embolism. However, most patients will recover completely with complete reversal of MRI changes; more severe cases will result in cerebral atrophy, demyelinating changes, and sequelae of infarction, hemorrhage, or necrosis.
The mainstay of treatment for fat embolism remains supportive care and possibly corticosteroid administration. Early fixation of long bone fractures has been advocated and in one study, there was significant increased risk of fat embolism with fracture fixation more than 10 hours after injury. Currently, mortality associated with fat embolism is reported at 7–10%.
Cerebral fat embolism should be suspected in trauma patients with otherwise unexplained neurologic deterioration: MRI with DWI and SWI should be performed for diagnosis and prognostication.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








