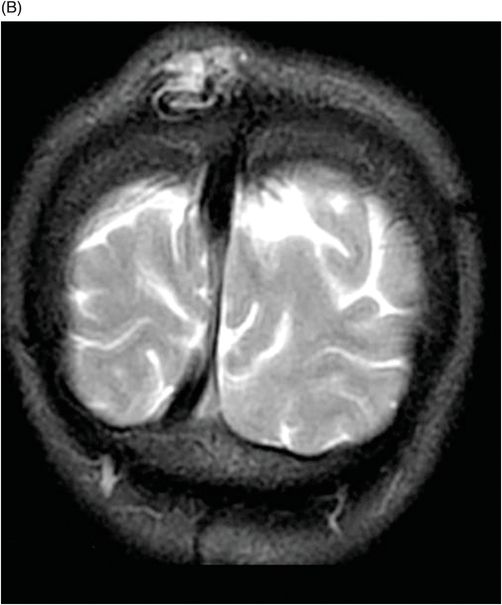
(A–B) Axial postcontrast T1WI SPGR MRI images through the parietal lobes.
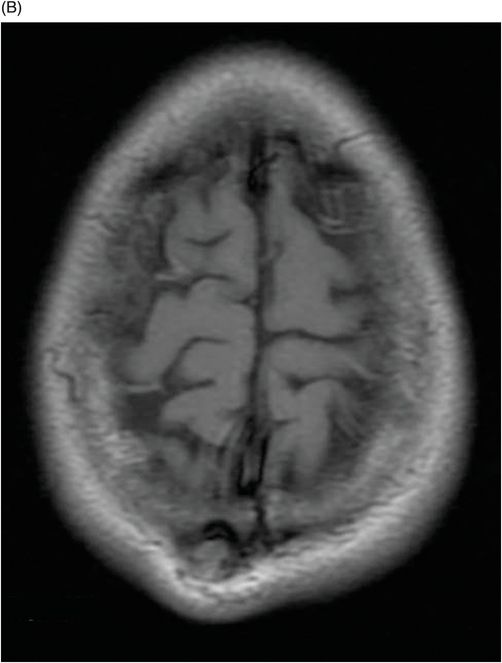
The MPR reconstruction on (A) Coronal and (B) Sagittal planes of the T1WI SPGR postcontrast images through the parietal region.

Sinus Pericranii
Primary Diagnosis
Sinus pericranii
Differential Diagnoses
Cephalocele/meningocele
Eosinophilic granuloma
Hemangioma
Imaging Findings
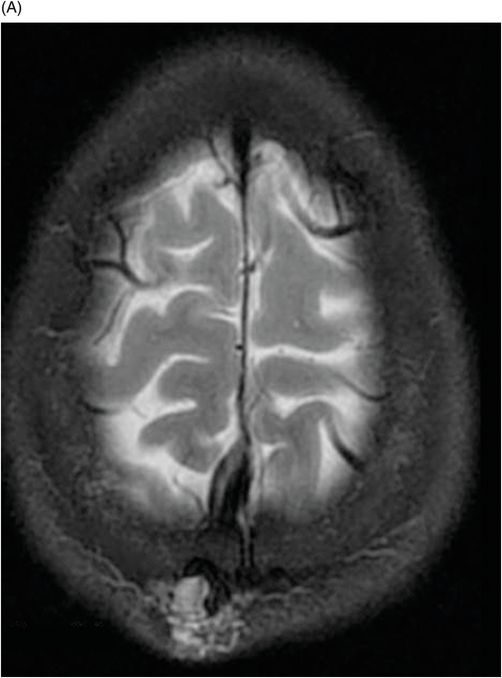
Fig. 35.1: (A) Axial and (B) Sagittal T1WI showed a soft tissue mass with foci of flow void adjacent on the right parietal region. Fig. 35.2 (A) Axial and (B) Coronal T2WI confirm a hyperintensity lesion on the right parietal region with a serpiginous vessel inside. Fig. 35.3: (A–B) Axial postcontrast T1WI SPGR MRI images demonstrated a soft tissue mass in the parietal region, with homogeneous gadolinium enhancement. Fig. 35.4: The MPR reconstruction on (A) Coronal and (B) Sagittal planes of the T1WI SPGR postcontrast images clearly demonstrated the trans-osseous connections between the soft tissue mass and the adjacent superior sagittal sinus.
Discussion
Sinus pericranii is an anomalous communication between the intracranial venous system (mainly the superior sagittal sinus) and epicranial venous structures via an adjacent, small bone defect. It is a slow-growing, developmental abnormality, usually occurring in infancy or secondary to trauma. They may vary in size in response to changes in intracranial pressure from Valsalva maneuver, crying, coughing, or from jugular vein compression.
Symptoms are infrequent, but include headache, vertigo, feelings of fullness, or local pain. Rarely, spontaneous thrombosis may occur, presenting with marked focal tenderness, and loss of compressibility. The most commonly involved bones are the frontal and parietal, followed by the occipital, and temporal.
Cephalocele is a fault involving the dura and the cranial vault associated with herniation of intracranial components. There are four main types: 1) meningoencephalocele, when there is herniation of CSF, nerves, and meninges; 2) meningocele, which is the herniation of the meninges, without brain parenchyma or nerves; 3) atresic cephalocele, which contains dura mater, degenerated fibrous and nervous tissue; and 4) gliocele, a cyst that is lined by glial cells and filled with CSF.
Osseous hemangiomas of the skull are benign, vascular lesions with capillaries, venous and cavernous vascular channels; they are histopathologically identical to soft tissue hemangiomas. They are more common in middle-aged females, with the peak incidence between the fourth and sixth decade of life. The outer table is commonly affected, while the inner table is spared. Either radiographic studies or CT scans show a typical lytic lesion, with trabecular matrix, periosteal reaction (sunbeam), and sclerotic margins. Magnetic resonance imaging is the best method to show lesion extension and its relationship to the adjacent neurovascular structures. Hemangiomas are typically hyperintense on T1WI and heterogeneously hyperintense on T2WI.
The most common imaging finding of calvarial eosinophilic granuloma is a well-defined mass involving the diploe. On CT, a sharply circumscribed skull lesion is identified with differential involvement of the inner and outer table. Magnetic resonance imaging shows these bone lesions as sharply defined soft tissue masses, with signal intensity equivalent to that of skeletal muscle and markedly enhanced after intravenous paramagnetic contrast medium.
Most cases appear to be congenital in nature and are frequently associated with other venous anomalies and syndromes. The primary concern is often cosmetic. The varicosities tend to increase in size slowly, although there has been a report of spontaneous regression.
Radiographic studies will show a bone defect with regular or irregular margins. A CT scan or MRI may demonstrate dilated vascular structures, which are enhanced on both sides of the cranial vault, close to a dural venous sinus or a cortical vein. Catheter angiogram may be required to confirm the diagnosis in difficult cases. Sinus pericranii may be associated with intracranial vascular anomalies, most commonly developmental venous anomalies.
Treatment is usually not required. Endovascular embolization may be performed to prevent hemorrhage, if the aberrant communication is large, or to address cosmetic concerns. Surgical resection is required in patients with complex anatomy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree