Herpes Simplex Cerebellitis
Primary Diagnosis
Herpes simplex cerebellitis
Differential Diagnoses
Rhombencephalitis
Acute disseminated encephalomyelitis (ADEM)
Cerebellar gliomatosis
Bilateral dysplastic cerebellar gangliocytoma (Lhermitte-Duclos disease)
Imaging Findings
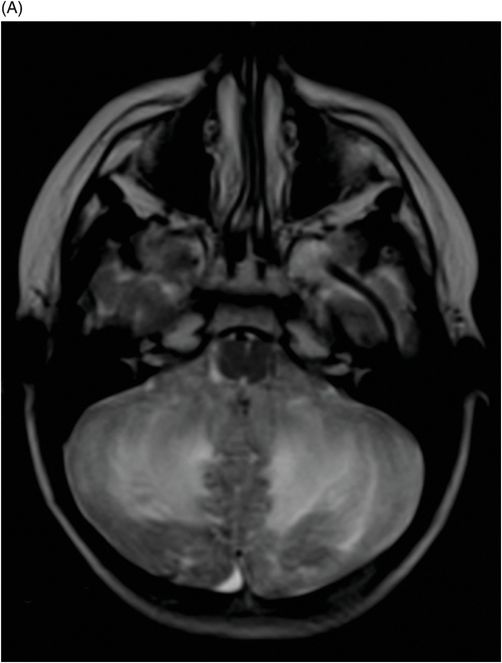
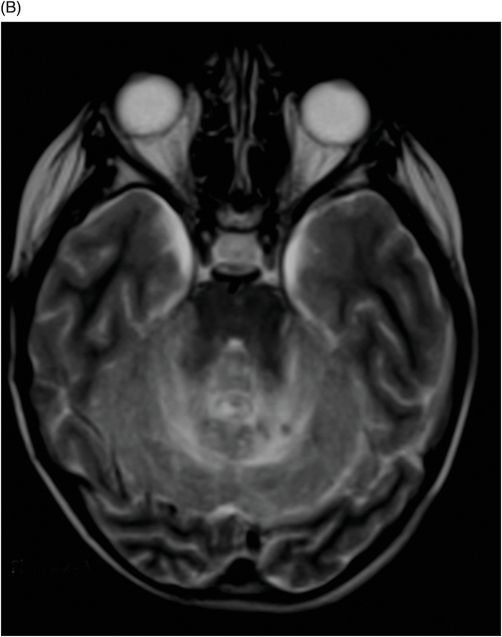
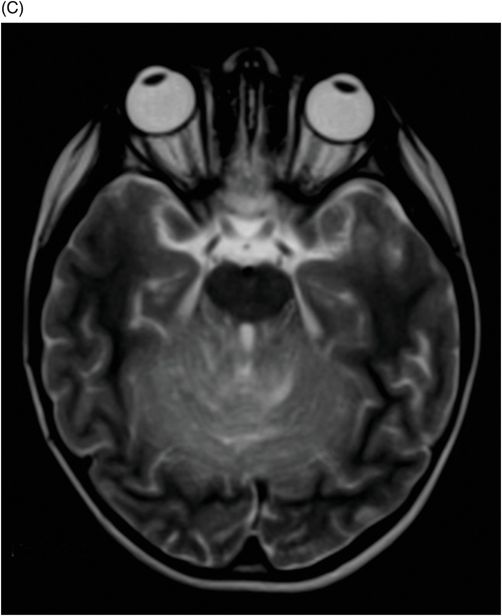
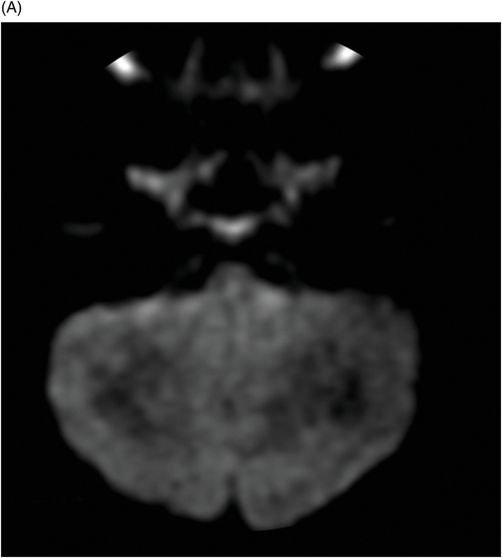
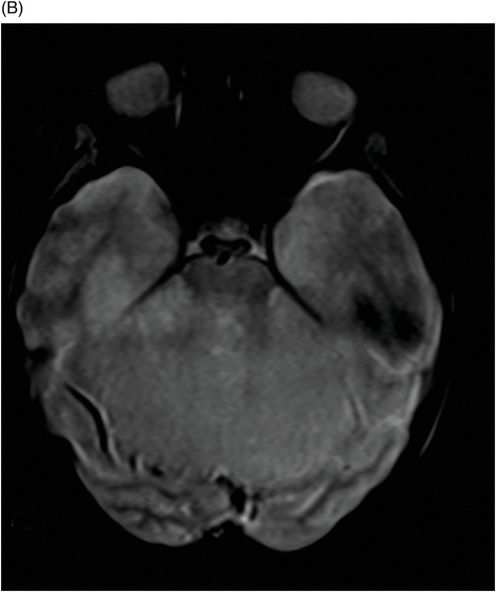
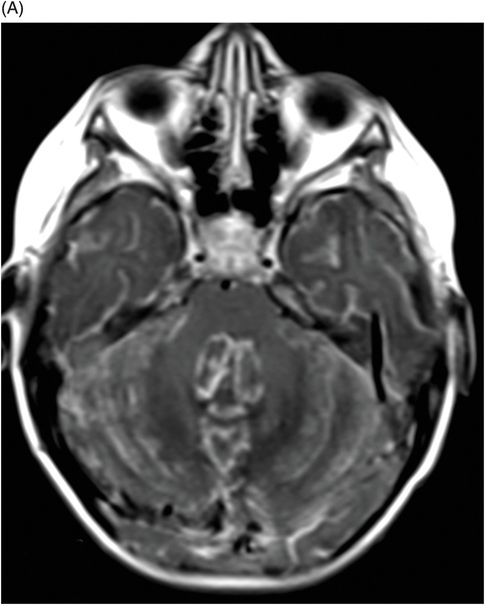
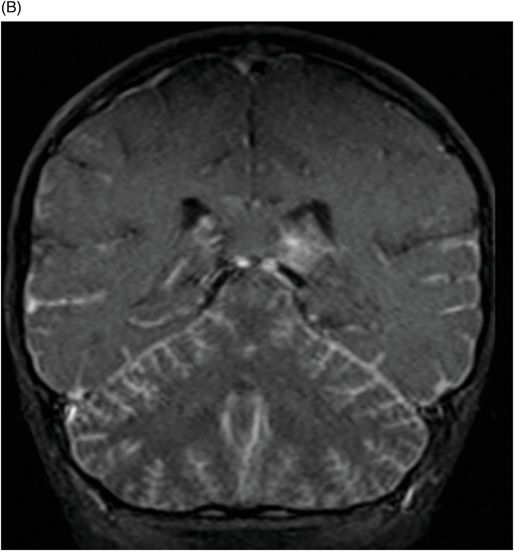
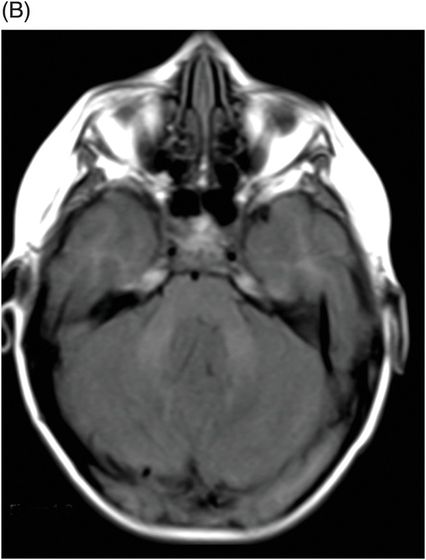
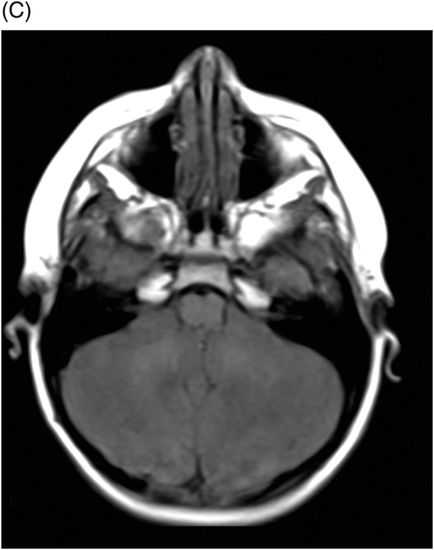
Fig. 37.1: (A) Sagittal and (B–C) Axial T1WI demonstrated increasing size of the cerebellum associated with some hypointense areas in the cerebellar parenchyma. The expansive effect exerts compression on the brainstem, promoting tonsillar herniation. Fig. 37.2: (A–C): Axial T2 images showed hyperintense signal of the cerebellar parenchyma, with edema and obliteration of the sulci between the folia cerebelli. Fig. 37.3: (A–B) Axial diffusion images did not demonstrate any areas of diffusion restriction. Fig. 37.4: (A) Axial and (B) Coronal postgadolinium T1WI showed diffuse leptomeningeal enhancement between the cerebellar leaves as well as in the temporal lobes.
Discussion
In patients presenting with altered level of consciousness, the clinical differential diagnosis of acute disseminated encephalomyelitis (ADEM) should be considered, initially. In patients with ADEM, the distribution of imaging lesions occurs more diffusely through the parenchyma and usually presents with asymmetrically located multifocal lesions. However, when a history of recent viral illness or vaccination is present, acute cerebellitis may be clinically and radiologically indistinguishable from ADEM that is confined to the cerebellum. Neurologic findings in a febrile child suggest that an infectious agent is responsible for the presenting clinical findings. Acute cerebellitis is a neurologic condition defined by fever, headache, dysarthria, nystagmus, tremor, truncal ataxia, and altered mental status. It should not be confused with acute cerebellar ataxia, which is not associated with fever or altered mental status. Acute cerebellitis is further characterized by CSF pleocytosis. Positive laboratory findings from PCR analysis of CSF fluid confirm diagnosis of human herpes virus-1.
Acute disseminated encephalomyelitis usually presents with asymmetrically located multifocal lesions and associated multifocal neurologic deficits. Multiple edematous white matter T2 hyperintense lesions occurring simultaneously are the classical imaging findings of ADEM. Asymmetrically distributed lesions affect the central white matter and cortical gray-white junction of both cerebral hemispheres and infratentorial areas: typically they are not pial postcontrast enhanced. In cases of rhombencephalitis, the lesions involve the cerebellum and brainstem diffusely. Acute disseminated encephalomyelitis is a focal disease and occurs after vaccination or viral infection, especially in children and adolescents. Cerebellar gliomatosis and Lhermitte-Duclos disease are generally excluded from the differential diagnosis because they are slow-growing lesions, without significant mass effect, and mainly because the patient is in good general condition and has no history of infection.
Acute cerebellitis is a major cause of cerebellar dysfunction in children and young adults. The main causal factors include infectious agents, reactive inflammatory processes, and postvaccine reactions. Numerous pathogens are directly associated with cerebellitis, with an emphasis on viral etiology. Varicella-zoster virus (VZV) has a tropism for posterior fossa structures, as it is transmitted transsynaptically through multiple different cranial nerves. Other Herpesviridae members, including Epstein-Barr virus (EBV or HHV-4), cytomegalovirus (CMV or HHV-5), and herpes virus variants (HHV-7 and HHV-8), have reportedly caused cerebritis. If cerebellitis onset stems from VZV reactivation, the typical vesicular skin-rash lesions may accompany CNS findings. Many other viral and bacterial causes of acute cerebellitis have been reported in the literature.
Although neuroimaging is diagnostically sensitive enough to confirm the presence of a herpes infection, it does not provide etiologic insight. Thus, MR is the imaging modality of choice for clinical assessment of suspected cerebellitis and can demonstrate hyperintense cerebellar parenchyma lesions in T2 and FLAIR sequences. Postcontrast-enhanced images will show leptomeningeal enhancement associated with diffuse edema, which may promote compression of brainstem, tonsillar herniation, and hydrocephalus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree