(A) Sagittal FLAIR and (B) Axial T2WI through the midbrain.
Listeria Rhombencephalitis
Primary Diagnosis
Listeria rhombencephalitis
Differential Diagnoses
Infiltrating glioma
Vertebrobasilar infarct
Demyelinating pathologies: tumefactive lesions, clinically isolated syndrome, and multiple sclerosis
Meta osmotic demyelination syndrome
Imaging Findings
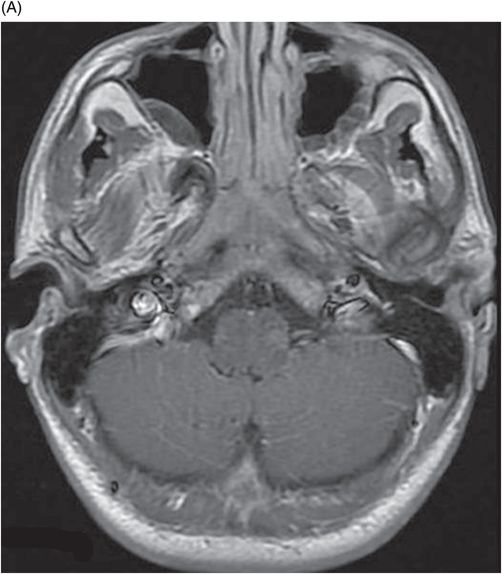
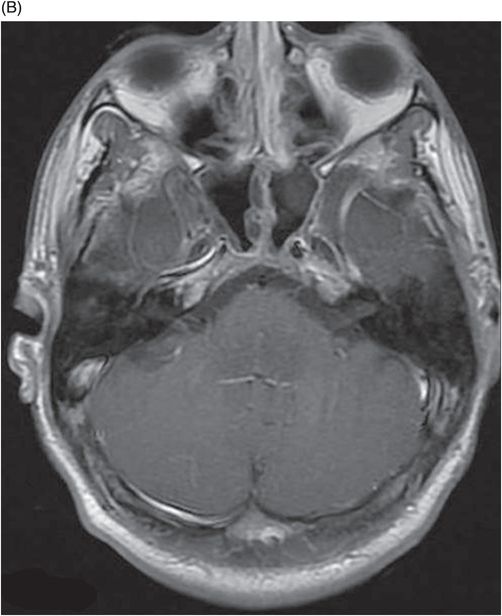
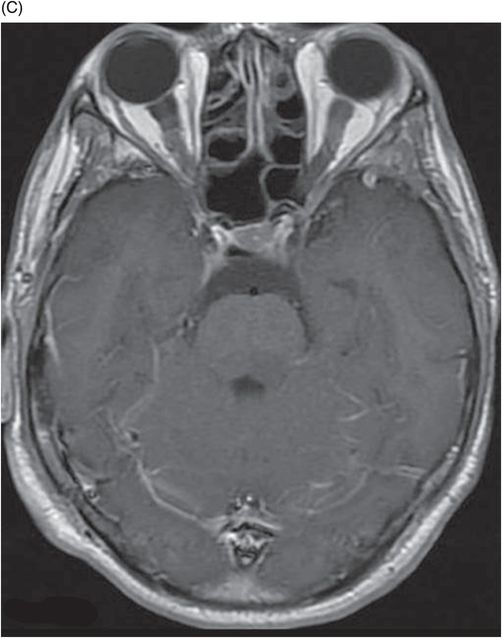
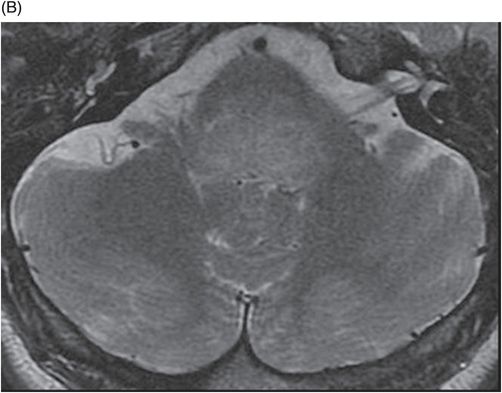
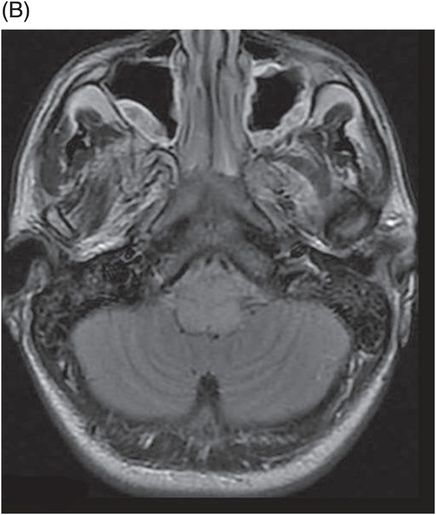
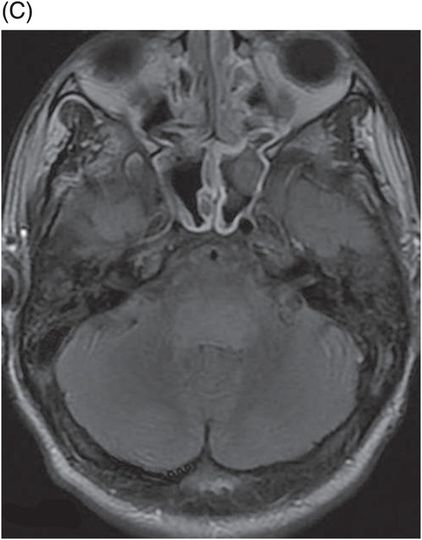
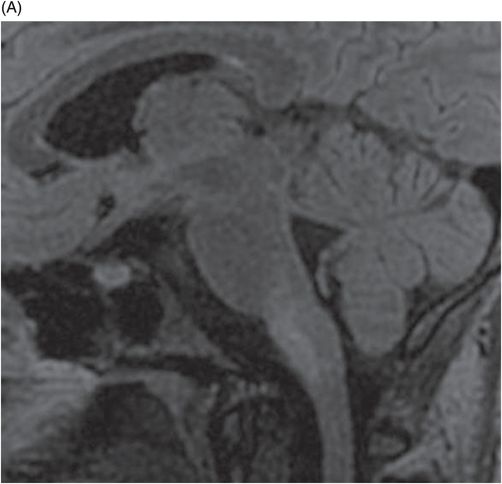
Fig. 38.1: (A) Sagittal FLAIR and (B–C) Axial FLAIR images demonstrated increased signal intensity in the dorsal pons, medulla, and upper cervical spinal cord. Fig. 38.2: (A–C) Postintravenous gadolinium injection axial T1WI demonstrated focal enhancement in the lateral medulla. Fig. 38.3: (A) Sagittal FLAIR and (B) Axial T2WI images (pre-antibiotic therapy).
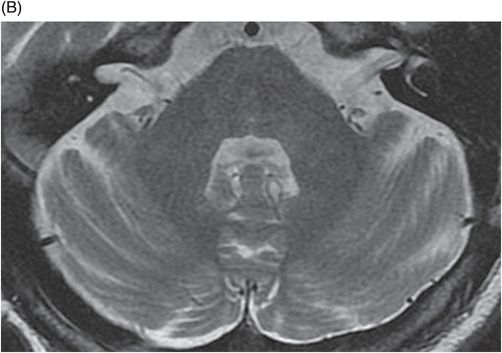
Fig. 38.4: (A) Sagittal FLAIR and (B) Axial T2WI (post-antibiotic therapy with ampicillin) demonstrated positive treatment response (improvement of the lesions).
Discussion
Confirmation of rhombencephalitis (RE) is based on the presence of brainstem and/or cerebellar dysfunction. In this patient, the clinical findings including corticospinal tract abnormality, a lowered level of consciousness, and CSF positive for pleocytosis are consistent features suggestive of RE. Several presenting features confirm the presence of an underlying infectious agent, rather than a tumefactive lesion or demyelinating syndrome. For example, the CSF polymorphonuclear predominance, the positive therapeutic response to ampicillin, lack of a clear association of the lesion with a particular vascular territory, acute verses gradual symptomatic onset, and enhancement focus on the brainstem, are suggestive of bacterial infection, most likely by Listeria monocytogenes.
Rhombencephalitis is a syndromic diagnosis referring to inflammatory diseases affecting the hindbrain (brainstem and cerebellum). Technically, the midbrain or mesencephalon is not part of the rhombencephalon, thus, the term brainstem encephalitis is often used interchangeably with RE. The first RE case, reported in 1957, was caused by Listeria monocytogenes. Since then, a variety of etiologies for RE have been described.
The etiologies of RE can be divided into three categories: infectious, autoimmune, and paraneoplastic syndromes. Listeria is the most common cause of infectious RE, followed by enterovirus 71 (EV 71), and the herpes viruses. Behçet disease (BD) is the most common autoimmune cause, but systemic lupus erythematosus (SLE) and relapsing polychondritis have caused RE, in isolated cases. In addition, paraneoplastic syndromes (PNS) have been associated with anti-Yo, anti-Tr, anti-Hu, and other antibodies.
Infectious agents can cause fever, meningeal signs, and low level of consciousness. Epstein-Barr virus (EBV) encephalitis predominantly affects the cerebellum, not the meninges. Patients with EBV typically present with ataxia, fever, without meningeal signs. Cranial nerve deficits are common in herpes virus infection, usually presenting with neuro-ophthalmologic abnormalities (abnormal ocular movements, nystagmus, anisocoria, ptosis, spasmodic movements, and oscillopsia). Cerebellar ataxia is common in PNS and infectious cases, and in only 10% of patients with BD. Long tract signs (corticospinal, spinothalamic, posterior column) occur in the majority of BD, but are uncommon in PNS and infectious causes, except listeria.
Cerebrospinal fluid analysis findings include pleocytosis and elevated protein. Listeria infection is associated with intense pleocytosis (range 20–3,300 cells/mm3, average 237 white blood cells). Intense pleocytosis was also described in patients with BD, viral and tuberculosis infection (> 100 cells/mm3), whereas in PNS, the mean cell count is up to 50 cells/mm3. Neutrophil predominance has been reported in both listeria infection and BD. A low CSF glucose level indicates that the infectious agent is bacterial.
Magnetic resonance imaging is extremely important for the etiologic diagnosis of RE. The usual MR findings are increased signal intensity in the pons, medulla, upper cervical cord, and cerebellum, more frequently than in the midbrain on T2WI or FLAIR MR scans. Listeria infection, unlike other causes, can cause ring-enhancing abscesses in these locations. In the series reported by Moragas et al., in 2011, MRI was normal in 100% of PNS cases and abnormal imaging was seen in all patients with multiple sclerosis (MS), BD, and listeriosis. Lesions caused by listeria were found in an exclusively intratentorial location. In MS, associated supratentorial and infratentorial lesions were more common.
In all patients with RE, blood culture and lumbar puncture should be performed to investigate the presence of HSV and tuberculosis by PCR, Gram stain and Ziehl-Neelsen stain in CSF, and to perform conventional and mycobacterium cultures. Empirical treatment with ampicillin and acyclovir should be initiated in all patients, with the possible exception of those who are afebrile and demonstrate normal MRI findings at presentation. Antibiotics can be changed based upon MRI, culture results, PCR results, and antibody studies.
The outcome of RE in all etiologic groups is similar, with the exception of individuals with PNS, who have the poorest prognosis, due to the unfavorable prognosis of the underlying disease. Exclusion of non-survivors does not improve the prognosis of Ramsay Hunt patients with PNS over those with the remaining etiologies.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree