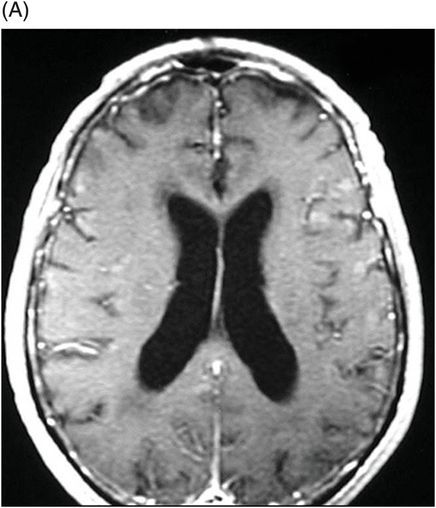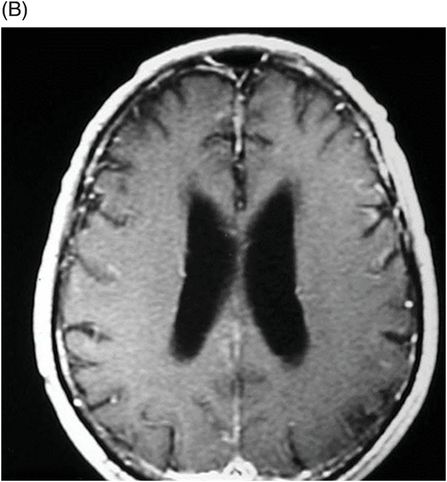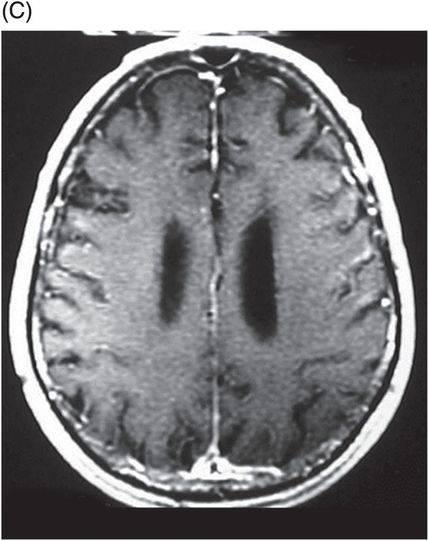
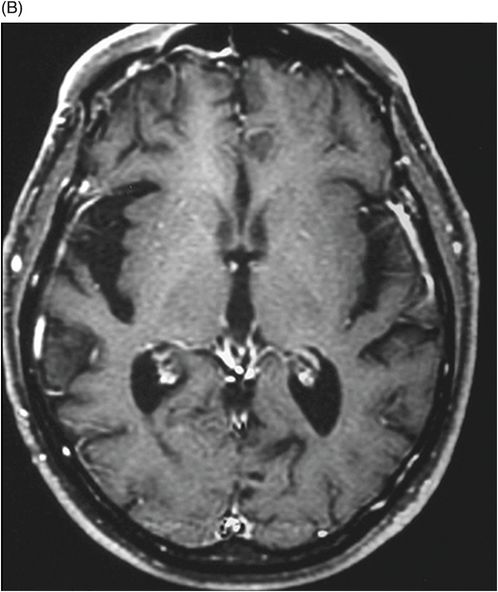
(A) Axial FLAIR and (B) Axial T1WI postgadolinium images through the third and lateral ventricles (two-year post-treatment follow-up).
Neurosyphilis Involving Temporal Lobe
Primary Diagnosis
Neurosyphilis involving temporal lobe
Differential Diagnoses
Meningeal syphilis
Syphilitic transverse myelitis
Herpes simplex infection
Polyradiculitis
Imaging Findings
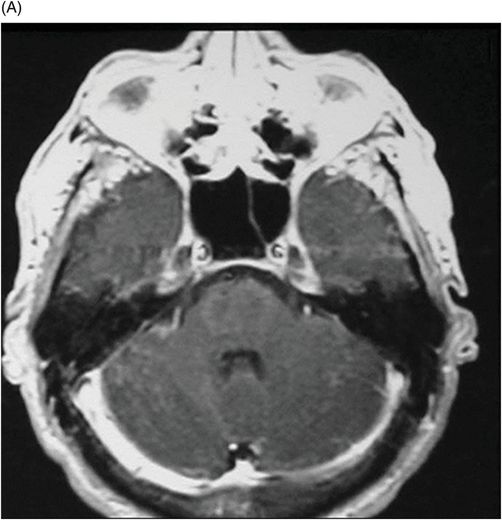
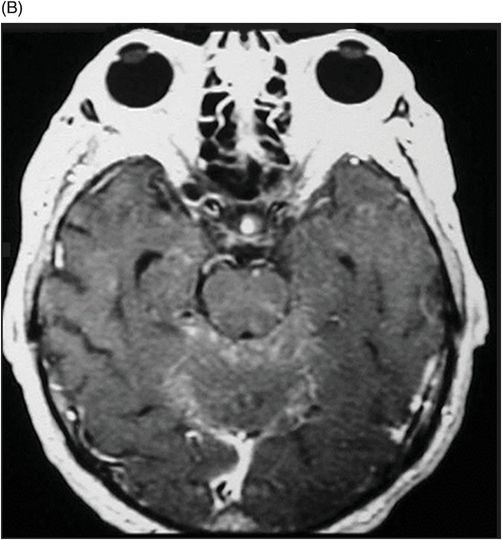
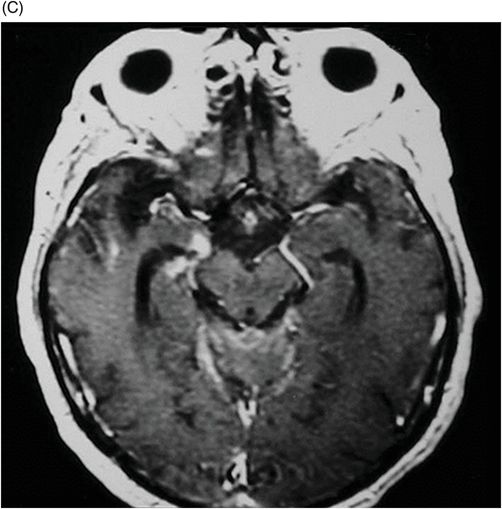
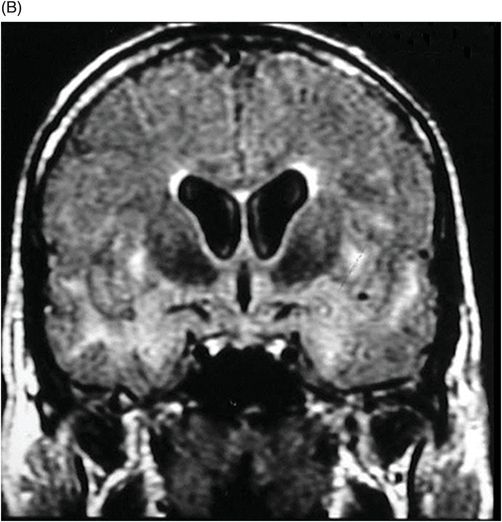
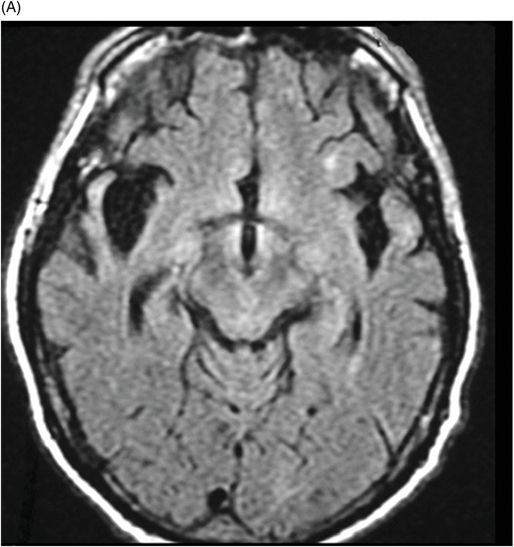
Fig. 40.1: (A–B) Coronal FLAIR demonstrated signal hyperintensity of the hippocampus and temporal lobe white matter. Fig. 40.2: (A–C) Postcontrast axial T1WI through the posterior fossa, and Fig. 40.3: (A–C) Contrast-enhanced, axial T1WI supratentorial images showed micronodular, abnormal enhancement on the right hippocampus, amygdala, temporal lobe, and leptomeningeal enhancement in the posterior fossa and supratentorial areas. Fig. 40.4: (A) Axial FLAIR and (B) T1WI postcontrast control images (two-year post-treatment follow-up) demonstrated improvement of the lesions and hippocampal and temporal lobe atrophy.
Discussion
The varied neuroradiologic findings in neurosyphilitic patients implicate numerous differential diagnoses, dependent on topographic location. For example, meningeal syphilis is difficult to differentiate from other inflammatory meningeal pathologies; syphilitic transverse myelitis, and polyradiculitis share some unspecific findings that also occur in myelitis; and the presence of high intensity signal in the temporal lobes can be difficult to differentiate from herpes simplex infections. Thus, patient clinical evaluation must encompass thorough appreciation of all presenting symptomatology in correlation with neuroradiologic findings.
Neurosyphilis is a parasitic infection of the brain and spinal cord caused by a sexually transmitted spirochete, Treponema pallidum. Central nervous system involvement typically indicates tertiary syphilitic infection. The increased prevalence of patients with AIDS coincides with a significant rise in the incidence of syphilis, and consequently, neurosyphilis. Approximately 1.5% of patients with AIDS develop neurosyphilis; however, it also occurs in 5–10% of untreated patients. Many patients with neurosyphilis are asymptomatic or have non-specific symptoms, confounding diagnostic efforts. However, its symptomatic nosology can be divided into four forms based on the predominant feature: meningeal, vascular (the most prevalent), general paresis, and tabes dorsalis (a rare manifestation in post-antibiotic era).
Syphilis follows a natural course of progression that has four stages: 1) early stage – chancre appears at the inoculation site with regional adenopathy; 2) secondary stage – two to four weeks later, the characteristic hematologic dissemination of syphilis manifests as a rash on the palms of the hands and soles of the feet, CNS involvement may occur, producing aseptic meningitis; 3) latent stage – begins when earlier symptoms disappear (serology remains positive for infection; and 4) tertiary syphilis – occurs 5 to 10 years after the primary infection and affects the CNS, cardiovascular system, bones, joints, skin, and mucous membranes.
Depending on the form, neurosyphilitic infection presents a wide variety of imaging findings. Meningeal neurosyphilis shows a focal or diffuse thickening and enhancement of the leptomeninges or pachymeninges, with or without hydrocephalus. The meningeal form can be also associated with cranial nerve involvement (commonly, CN II, and VIII), and formation of focal leptomeningeal granulomas or gummas of various sizes, which appear iso- to hypointense on T1WI, and hyperintense on T2WI. Vascular neurosyphilis shows evidence of multiple focal hyperintensities on T2WI, involving both gray and white matter associated with small foci of infarcts, secondary to vasculitis. In patients with the general paresis form, classical findings include frontal and temporal lobe cortical and subcortical atrophy, with subcortical gliosis. The tabes dorsalis form demonstrates an increase in signal intensity of the spinal cord on T2WI, a contrast enhancement of the pia and of the spinal cord nerve roots, and spinal cord atrophy.
Laboratory data can help approximate the diagnosis and may include positive serum fluorescent antibody findings, pleocytosis, elevated protein levels, or a positive VDRL test. The CSF should be analyzed; analysis should include VDRL, at least one treponemal reaction (FTA abs), PCR for Treponema pallidum, as well as standard CSF tests. Although VDRL of CSF is highly specific for neurosyphilis, it is negative in approximately one-half of neurosyphilis patients.
Owing to immunocompromise, the course of neurosyphilis in HIV-infected patients tends to be more aggressive than it is in the general population.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree