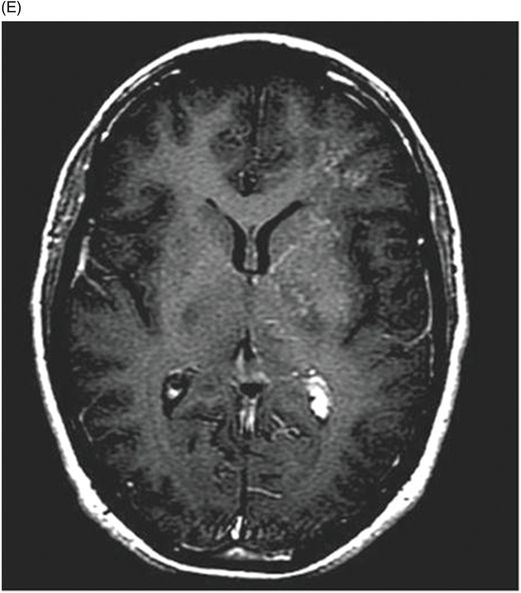
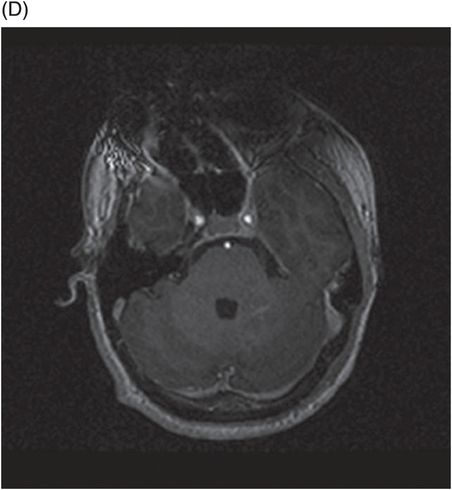
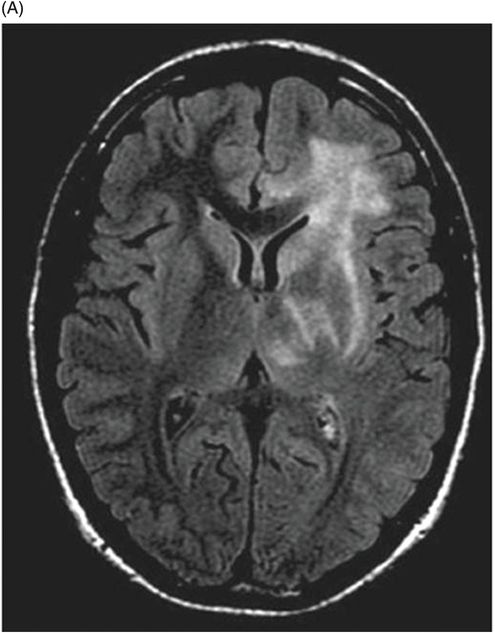
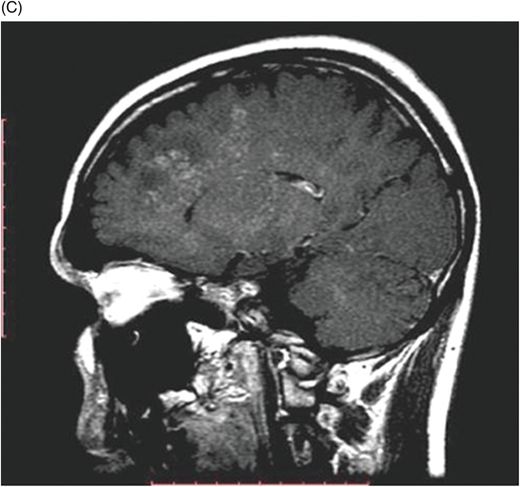
(A) Axial FLAIR, (B) Coronal T2WI, (C) Sagittal T1WI postgadolinium, (D) Coronal T1WI postgadolinium, and (E) Axial T1WI postgadolinium images (two months after initial admission imaging studies) through the level of the frontal lobes.


Cerebral Schistosomiasis
Primary Diagnosis
Cerebral schistosomiasis
Differential Diagnoses
Central nervous system neoplasm
Neurosarcoid
Tuberculosis
Neurocysticercosis
Imaging Findings
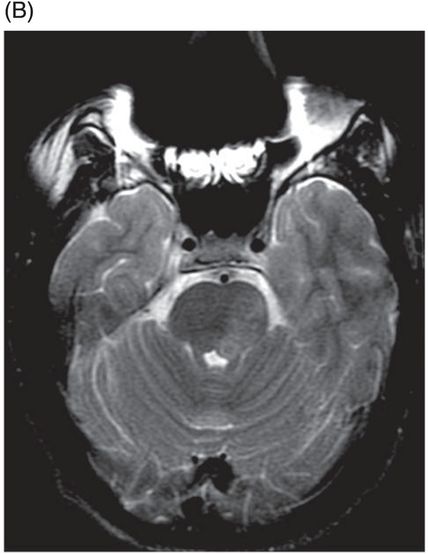
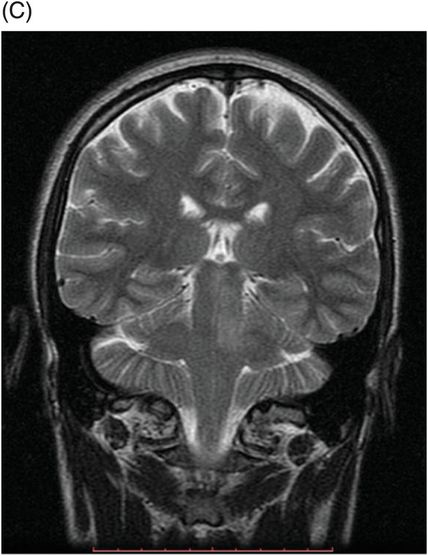
Fig. 44.1: (A) Axial FLAIR, (B) Axial T2WI, (C) Coronal T1WI, and (D) Axial T1WI postgadolinium images (MR studies from initial admission) demonstrated a hyperintense lesion on the left pons with a small, enhanced nodule in the left middle cerebellar peduncle. Fig. 44.2: (A) Axial FLAIR, (B) Coronal T2WI, (C) Sagittal T1WI postgadolinium, (D) Coronal T1WI postgadolinium, and (E) Axial T1WI postgadolinium images (two months after MR studies from initial admission) demonstrated multiple punctate, spotty, nodular, enhancing lesions, with surrounding vasogenic edema, in the left periventricular white matter and corona radiata of the left frontal lobe, and ipsilateral basal ganglia.
Discussion
Symptoms of cerebral schistosomiasis are non-specific, and patients usually present with headache, seizures, and focal neurologic deficits. The association of non-specific symptoms in conjunction with imaging findings may lead inexperienced radiologists to incorrectly diagnose schistosomiasis as a CNS neoplasm. Therefore, it is important that radiologists are able to recognize the typical MRI features associated with schistosomias in order to establish the correct diagnosis and avoid unnecessary surgery.
On MR imaging studies, cerebral schistosomiasis characteristically demonstrates the presence of lesions with long T1 and T2 signals that are associated with prominent, surrounding vasogenic edema and mass effect. Following intravenous contrast administration, nodular enhancement is noted and eventually demonstrates central, linear enhancement – the characteristic arborized pattern typically seen in patients with cerebral schistosomiasis. The cerebral hemisphere is more frequently affected, followed by the cerebellar hemispheres, basal ganglia, and brainstem. The enhancing lesions seen in this patient, from an endemic region in South America, are suggestive of cerebral schistosomiasis.
Schistosomiasis is a chronic parasitic infection caused by trematode blood flukes of the genus Schistosoma. The three main species that affect humans are S. mansoni, S. haematobium, and S. japonicum. They are responsible for infecting more than 200 million people in 77 countries, with an annual mortality rate of 200,000. Schistosoma mansoni is endemic in tropical Africa, the Near East, northeastern South America, and the eastern Caribbean islands. Schistosoma haematobium is found in Africa and the Middle East, and S. japonicum is found exclusively in Asia.
The Schistosoma life cycle begins when worm eggs in human feces or urine hatch in fresh water, infecting snails (intermediate host). The snails release their larvae (cercariae) into the water, infecting humans through contact with skin or mucosa, migrating to the liver or lungs, where they mature. The mature schistosome then migrates to the intestines and bladder venous plexus, where it releases eggs that are then excreted in urine and feces, finishing the life cycle.
Schistosoma usually affects the liver and intestines, causing hepatic fibrosis, portal hypertension, and intestinal and bladder complications, such as carcinogenesis. There have been a few cases reported of S. mansoni and S. haematobium ectopic worm migration to the CNS – causing spinal cord lesions and rarely, affecting the brain. Conversely, S. japonicum typically affects the brain. The most likely explanation for this exception is because its eggs are smaller and lack spines, allowing them to reach the brain via the plexus of Batson. The presentation of the unique arborized pattern on MR images characteristic of Schistosoma infestation, if seen, in a patient from a schistosomiasistic endemic zone, can be used to distinguish between a CNS neoplasm, neurosarcoid, tuberculosis, and neurocysticercosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree