Primary Angiitis of CNS (PACNS)
Primary Diagnosis
Primary angiitis of CNS (PACNS)
Differential Diagnoses
Leptomeningeal carcinomatosis
Meningitis
Neurosarcoidosis
Reversible cerebral vasoconstriction syndrome (RCVS)
Central nervous system manifestations of systemic vasculitis
Imaging Findings
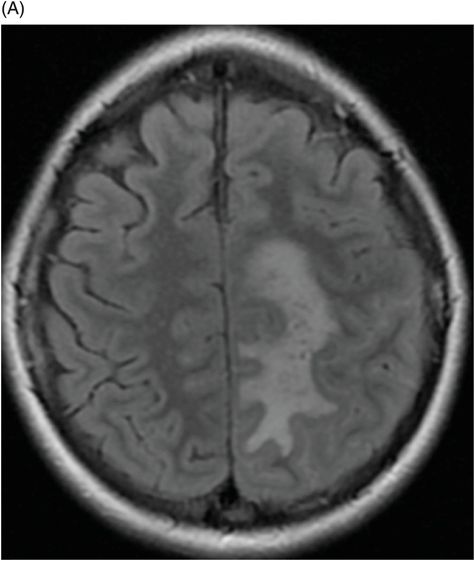
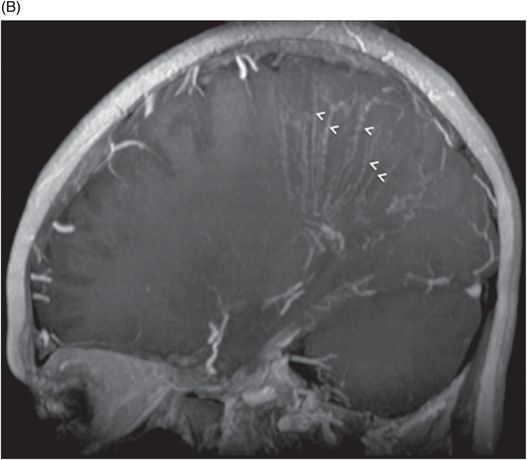
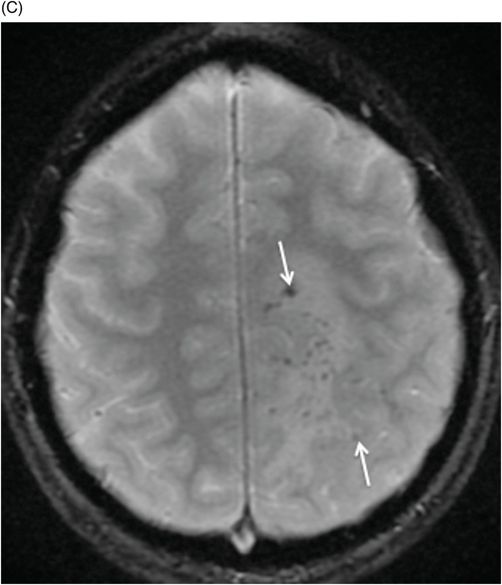
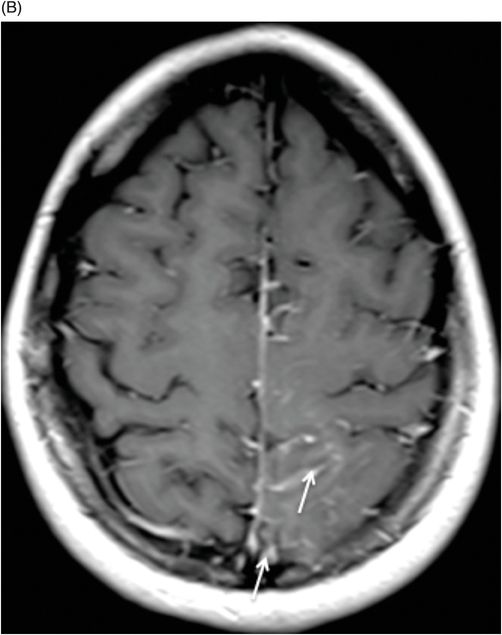
Fig. 51.1: (A) FLAIR image demonstrated abnormal signal in the left parietal subarachnoid space (arrows) with no obvious abnormality involving the cortex or subcortical white matter. (B) Postcontrast T1WI sequence demonstrated leptomeningeal enhancement on the left parietal region, as well as linear enhancement in the subcortical white matter. Fig. 51.2: (A) FLAIR image demonstrated prominent FLAIR abnormality involving cortical and subcortical white matter of the left posterior frontal and left parietal region. (B) Sagittal postcontrast image demonstrated prominent vascular/perivascular enhancement (arrowheads) in the left posterior frontal and parietal lobe. No significant leptomeningeal enhancement was noted. (C) GRE image demonstrated numerous microhemorrhages (arrows) in the subcortical white matter. A tiny focus of diffusion restriction was noted in the left superior frontal gyrus. Fig. 51.3: Composite MIP image of the 3D TOF MRI image demonstrated focal stenosis (arrows) involving multiple M2 branches of the left middle cerebral artery (MCA). There is paucity of the left M3 branches, as compared to the right side. Note that the right MCA and its branches are unremarkable.
Discussion
Although PACNS lacks characteristic imaging findings or a typical clinical presentation, a constellation including male gender, middle aged (50 years of age), subacute onset of headache, and stroke-like symptoms correlates with the profile of the PACNS patient. Although initial imaging appearance is non-specific, imaging findings from the second MRI and MRA are strongly suggestive of vasculitis. The presence of large areas of cortical and subcortical white matter FLAIR abnormality associated with a tiny focus of diffusion restriction is suggestive of critical ischemia of a large tissue with focal area of acute infarct. Presence of microhemorrhages and multifocal vascular narrowing on MRA are also suggestive of vasculitis. Extensive vascular/perivascular enhancement in the involved area suggests vessel wall disease. In the absence of systemic vasculitides, the clinical presentation and imaging findings are highly suggestive of PACNS.
Although leptomeningeal enhancement in a 50-year-old is highly suggestive of leptomeningeal carcinomatosis, it was ruled out because of the lack of any known primary malignancy. Mild CSF pleocytosis and the absence of fever or meningeal signs ruled out the possibility of meningitis. Absence of chest sarcoidosis, increased serum or CSF ACE levels, and punctate enhancement are not suggestive of neurosarcoidosis. Relatively subacute, rather than acute, presentation and male gender are not typical of RCVS.
Primary angiitis of CNS is a rare disease with annual incidence of 2–4 cases per million people per year. It is more common in males and the average age at presentation is 50 years. The diagnostic criteria of PACNS include: 1) new-onset neurologic deficit; 2) angiographic or histologic evidence of vasculitis; and 3) absence of systemic condition that can explain the findings. As the treatment of PACNS includes cytotoxic therapy, proper patient selection is very important. Diagnosis of PACNS may be definite if it is proven by biopsy, or probable if clinical, laboratory, and imaging findings are highly suggestive of diagnosis. The disease has various forms: 1) non-progressive, large- and medium-vessel disease, 2) progressive, large- and medium-vessel disease; or 3) angiographically occult small vessel disease. All PACNS variants are age-dependent.
Primary angiitis of CNS typically involves small to medium-sized arteries and veins, especially those located close to the meninges and subcortical white matter. T-cell and activated macrophage infiltration of the vessel wall, with granuloma formation, and adventitia involvement (usually associated with intimal proliferation), with luminal narrowing are characteristic microscopic findings.
Gradually worsening headache and cognitive impairment are the most common initial symptoms. Focal neurologic deficits appear later in the disease process. Small vessel disease, frequently occult on angiography, more commonly presents with acute or subacute encephalopathy in conjunction with headache, confusion, and cognitive impairment. In contrast, larger vessel disease more commonly presents with infarctions and focal neurologic deficits frequently demonstrated as angiographic abnormalities.
Magnetic resonance imaging is sensitive but not specific for this disease and is abnormal in 90–100% of patients. The most common imaging abnormality involves T2-FLAIR hyperintensity involving the subcortical white matter, followed by deep gray matter, deep white matter, and superficial cortex. Acute infarcts can only be seen in 50% of cases. Acute presentation may have mass effect and cortical or subcortical swelling that can be confused with a superficial tumor. Diffuse, unexplained small vessel ischemic disease involving deep cerebral and periventricular white matter may be seen. These lesions may be focal and can be confused with multiple sclerosis. Chronic superficial lesions can present as laminar necrosis. Enhancement with contrast can be seen in only one-third of all cases. No specific enhancement pattern is known. Leptomeningeal enhancement can be seen in 10–15% of cases. Subarachnoid hemorrhage is a not common finding, but can be seen as was noted in this patient.
Conventional angiogram is more specific but less sensitive for the diagnosis of PACNS than MRI. The reported sensitivity of angiographic abnormalities is 20–90% and specificity is 20–60%. Sensitivity increases if medium- or larger-sized blood vessels are involved. Typical angiographic appearances include beading of blood vessels, or segmental narrowing of the small or medium-sized blood vessels. Biopsy may be required in equivocal cases and should target the enhancing meninges, if present, for maximum yield of biopsy.
There is no specific management recommendation for PACNS. Usually treatment is started with glucocorticoids, with or without cyclophosphamide, or other immunosuppressive therapy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree