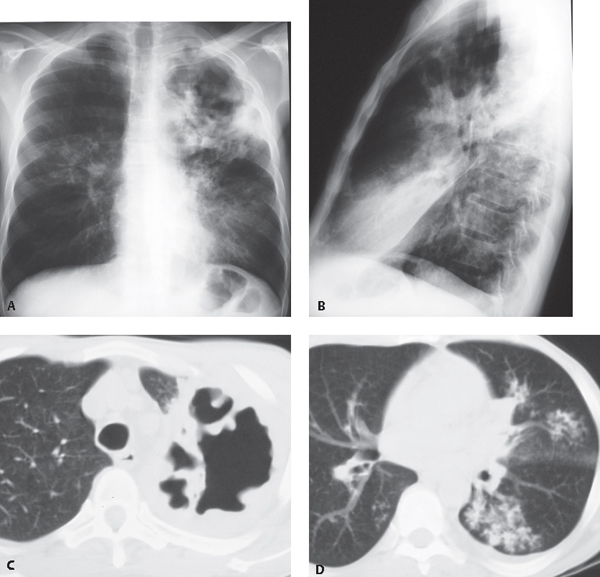
CASE 59 55-year-old man with history of alcohol and drug abuse presents with chronic cough, low-grade fever, and weight loss Posteroanterior (PA) (Fig. 59.1A) and lateral (Fig. 59.1B) chest radiographs demonstrate a large left upper lobe cavity with irregular nodular borders and adjacent pleural thickening. Note right lower lobe, lingular, and left lower lobe consolidations. Coned-down unenhanced chest CT (lung window) (Figs. 59.1C, 59.1D) demonstrates the irregular left upper lobe cavity (Fig. 59.1C) and tree-in-bud and centrilobular nodules in the lingula, left lower, and right lower lobes (Fig. 59.1D) consistent with endobronchial spread of pulmonary infection. Fig. 59.1 Mycobacterium tuberculosis • Non-Tuberculous Mycobacterial Infection • Other Necrotizing Pulmonary Infections (fungi, atypical organisms) • Lung Abscess with Multifocal Bronchiolitis Tuberculosis is the leading cause of death from infectious disease worldwide. More than two billion people (one-third of the world population) are infected, with approximately nine million new cases and nearly two million deaths reported annually and most of these occurring in developing countries. Tuberculosis is a worldwide pandemic, but over half of all new cases are reported in Asia and Africa. Approximately 1.4 million affected patients were infected with HIV in 2007, most of these in the African region. In the United States, approximately 13,000 new cases were reported in 2008, with a case rate per 100,000 population of approximately 4.2. Individuals at risk in the United States include those in ethnically diverse populations, immigrants, minorities, the homeless, the immunocompromised (particularly HIV-infected patients), and the elderly. Tuberculosis is caused by M. tuberculosis, an aerobic rod transmitted from person to person through inhalation of droplets containing tubercle bacilli. The organisms are initially deposited in the mid and lower lung zone alveoli, multiply within macrophages, and disseminate via lymphatic and hematogenous routes. Cell-mediated immunity develops up to 10 weeks after initial infection. Most patients contain their disease, but approximately 5% develop active tuberculosis within the first or second year after initial infection and approximately 10% develop active disease in their lifetime. Progression to active infection is more common in HIV-infected individuals, with a risk of up to 10% per year. Infection may also occur through re-activation of organisms that survive in areas of high oxygen tension or via exogenous exposure. Patients with latent tuberculosis infection are asymptomatic and have a positive tuberculin skin test, but do not have active tuberculosis infection and are not infectious. These patients may be diagnosed via whole blood interferon-γ assay, which provides higher diagnostic accuracy than the traditional skin tests. Patients with tuberculosis disease have clinical, radiologic, and/or laboratory evidence of infection. The old concepts of primary and post-primary tuberculosis have been challenged, as tuberculosis infection worldwide is not likely to represent a single infectious event and re-infection is likely frequent. However, the nomenclature remains useful in categorizing the imaging manifestations of the disease. The radiologic features associated with primary and post-primary (or reactivation) tuberculosis correlate better with the host immune status than with the time elapsed since initial infection. Thus, severely immunocompromised patients typically exhibit the “primary pattern” of tuberculosis whereas immunocompetent individuals often exhibit the “post-primary pattern” of infection. The majority of patients with tuberculosis have pulmonary involvement. Extrapulmonary tuberculosis is more common in children and immunosuppressed patients. Affected patients may remain asymptomatic or present with a severe symptomatic pneumonia after initial infection. Patients with pulmonary tuberculosis may have an indolent clinical course and often present with cough, chest pain, and hemoptysis. Systemic complaints may include fever, chills, night sweats, anorexia, weight loss, weakness, and malaise. The diagnosis of tuberculosis is based on the identification of M. tuberculosis in body fluids or tissue.
 Clinical Presentation
Clinical Presentation
 Radiologic Findings
Radiologic Findings
 Diagnosis
Diagnosis
 Differential Diagnosis
Differential Diagnosis
 Discussion
Discussion
Background
Etiology
Clinical Findings
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree