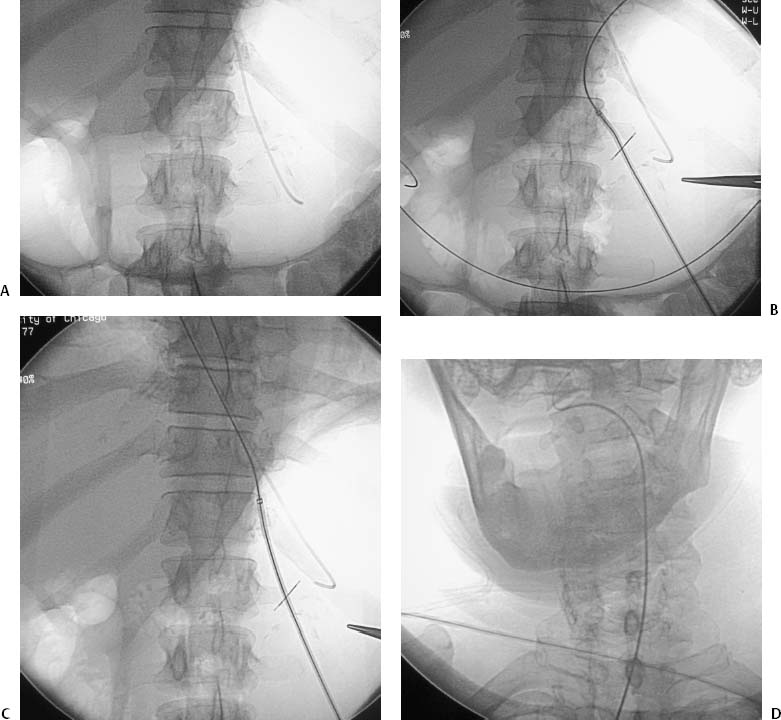
CASE 6 A 68-year-old male presented to our department with cerebrovascular accident and failure to thrive. Figure 6-1 Mushroom-retained gastrostomy. (A) Fluoroscopic image shows the stomach inflated via a 5F nasogastric catheter. (B) Fluoroscopic image shows that the stomach has been punctured and a 10F vascular sheath has been inserted into the stomach. (C) Fluoroscopic image shows retrograde catheterization of the esophagus using the sheath and guidewire. (D) Fluoroscopic image shows catheter and guidewire in the oropharynx. (E) Final fluoroscopic image shows 20F mushroom-retained catheter in the stomach. (F) Photograph of pull-type gastrostomy tube. Head CT revealing left middle cerebral artery (MCA) stroke (not shown). Stroke with inability to eat. After intravenous administration of 1 mg glucagon, the stomach is inflated using an indwelling nasogastric tube (Fig. 6-1A). An incision approximately 5 to 10 mm long is made along the intended puncture site. The midbody of the stomach is punctured, and a single retaining suture (T-tack) is deployed to hold the stomach against the anterior abdominal wall (Fig. 6-1B). The esophagus is catheterized using a 0.035-inch Rosen guidewire and 10-French (F) sheath (Fig. 6-1C). In some cases, a directional 5F catheter such as an RC-1 (Boston Scientific, Natick, Massachusetts) is used. Once the esophagus has been catheterized, the guidewire is advanced cephalad to the mouth. Occasionally, it is helpful to turn the patient’s head slightly to the left or right. Using direct fluoroscopic guidance, the wire is then directed out of the mouth and grasped with a hemostat (Fig. 6-1D).
Clinical Presentation
Radiologic Studies
Diagnosis
Treatment
Percutaneous Mushroom Gastrostomy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree