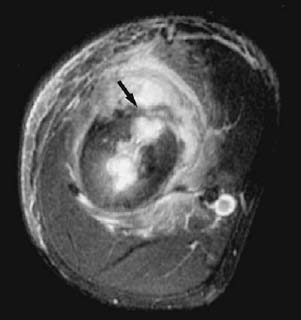
CASE 68 Sam Y. Chun, Ali Islam, Alison Spouge, Anthony G. Ryan, and Peter L. Munk A 15-year-old boy presented with a 6-month history of arm pain. Figure 68A Figure 68B Figure 68C The anteroposterior (AP) radiograph of the humerus (Fig. 68A) shows extensive solid periosteal new bone in the diaphyseal region, with expansion and remodeling of the bone. An AP tomogram (Fig. 68B) shows irregular, well-defined lucencies in the medullary cavity and lateral cortex of the bone (arrows). An axial fast inversion recovery sequence (Fig. 68C) reveals discrete high signal intensity in the medullary cavity with cortical breakthrough anteriorly (arrow), consistent with a draining sinus track, in addition to cortical thickening and periosseous soft-tissue edema. Chronic osteomyelitis. Chronic osteomyelitis is prolonged infection of the bone (generally defined as lasting more than 6 weeks), typically affecting adults. It is most often a sequela of an open fracture and may also be associated with vascular insufficiency, inadequate treatment, or immune deficiency. Chronic osteomyelitis may be classified as active or inactive, but differentiating the two is often difficult. Active infection implies that the pathogens are viable, which may be detected radiographically by the presence of sequestra, abscesses, and subperiosteal fluid collections. Brodie’s abscesses may be seen in both subacute and chronic infections; however, this entity is discussed separately in case 69. Chronic osteomyelitis is usually the sequela of an acute infection; therefore, the same organisms are involved, particularly Staphylococcus aureus. Patients with chronic osteomyelitis may present with localized bone pain, erythema, and draining sinus tracts. In chronic active osteomyelitis, the viable pathogens may remain isolated within the sequestrum and give rise to recurrent episodes of acute osteomyelitis. The patient may be asymptomatic between exacerbations. Complications can be severe and sometimes fatal. Serious complications include septic arthritis, epiphyseal plate damage with secondary growth disturbances in children, and epidermoid carcinoma of the fistula. Epidermoid carcinoma, usually squamous cell carcinoma, occurs in 0.5 to 1.6% of patients with chronic osteomyelitis, with a 20- to 40-year latent period. Radiographic signs of malignant transformation include a lytic lesion superimposed on changes of chronic osteomyelitis, soft-tissue mass, and pathologic fracture. Several factors may contribute to the progression of acute osteomyelitis into chronic osteomyelitis.
Chronic Pyogenic Osteomyelitis
Clinical Presentation


Radiologic Findings
Diagnosis
Differential Diagnosis
Discussion
Background
Etiology
Clinical Findings
Complications
Pathogenesis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


