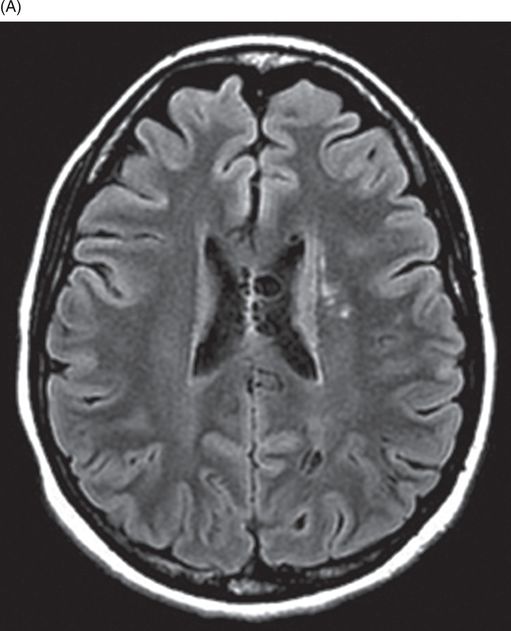
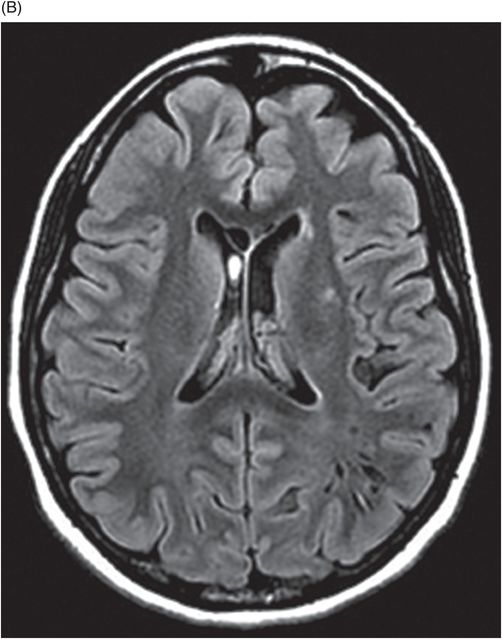
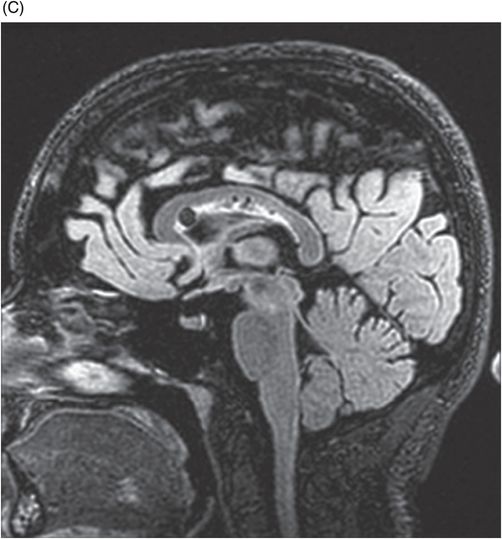
(A–B) Axial FLAIR images at the level of lateral ventricles and corona radiata. (C) Midsagittal FLAIR image through the corpus callosum.
Hypomelanosis of Ito
Primary Diagnosis
Hypomelanosis of Ito
Differential Diagnoses
Incontentia pigmenti
Tuberous sclerosis
Periventricular leukomalacia
TORCH group of infections
Imaging Findings
Fig. 70.1: Axial T2W image at the level of corona radiata and lateral ventricles showed multiple dilated perivascular spaces in the genu of corpus callosum, left periventricular, and left parietal subcortical white matter. Fig. 70.2: (A–B) Axial and (C) Midsagittal FLAIR images showed dilated perivascular spaces in the corpus callosum, periventricular, and left parietal subcortical white matter. Fig. 70.3: Axial postgadolinium image did not show enhancement. Fig. 70.4: (A–B) Diffuse hypopigmented skin lesions were noted along the lines of Blaschko on the abdominal wall, trunk, right thigh, and leg.
Discussion
Hypopigmented skin patches along the lines of Blaschko, and dilated perivascular spaces in a patient with mental retardation and seizures clinch the diagnosis of hypomelanosis of Ito.
Incontentia pigmenti is a closely mimicking diagnosis that also presents with dermal manifestations; however, the hyperpigmented skin lesions help in differentiating it from hypomelanosis of Ito. Lack of cortical tubers and other migration anomalies on neuroimaging make tuberous sclerosis a less likely diagnosis. The typical cutaneous manifestations in tuberous sclerosis include adenoma sebaceum and not hypopigmented lesions. Absent history of birth, asphyxia, and negative TORCH group of infections in a patient with hypopigmented skin lesions helps in excluding these options as the primary diagnosis.
Hypomelanosis of Ito is a multisystem neurocutaneous syndrome involving the scalp, hair, nervous system, eyes, dentition, and skeletal system. It results from sporadic chromosomal mosaicism and affects neural migration. The cellular migration defect usually takes place in the second trimester and involves melanoblasts and neuroblasts, resulting in various cutaneous and nervous system abnormalities. Microscopic examination of the involved skin shows decreased number of melanocytes and pigmented melanosomes. The clinical presentation is varied, presenting in the form of unilateral or bilateral hypopigmented linear white streaks, patches, or whorls with irregular borders along the line of Blaschko. Focal alopecia, trichorrhexis nodosa, dysmorphic facies with flattened face, frontal bossing, macrocephaly/microcephaly, and hypertelorism, cup-shaped ears with external auditory canal stenosis are the craniofacial features. Skeletal deformities include short stature, scoliosis, syndactyly, polydactyly, and brachydactyly. Association with a wide range of cardiac, genitourinary, and ophthalmologic abnormalities are also noted.
According to neuroradiologic literature, the frequency of neurologic involvement is variable and ranges from 10% to 100%. Mental retardation is often seen in more than 60% of cases with a varying degree of severity. Magnetic resonance imaging findings include hemimegalencephaly, cerebellar atrophy or hypoplasia, pachygyria, heterotopia, cortical dysplasia, dilated perivascular spaces, bilateral periventricular cysts, and indistinct cortical gray-white matter differentiation. The wide range of migrational anomalies account for the seizures and mental retardation. Other infrequent findings include agenesis of corpus callosum, focal cerebral atrophy, and in rare instances, medulloblastoma, choroid plexus papilloma, and arachnoid cyst are some of the associated pathologies. Seizure control with antiepileptic medications is the mainstay of treatment for hypomelanosis of Ito.
Ruiz-Maldonado et al. have proposed diagnostic criteria for hypomelanosis of Ito:
A) Sine qua non-criterion: congenital or early-acquired non-hereditary, cutaneous hypopigmentation in linear streaks or patches involving more than two body segments.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree