
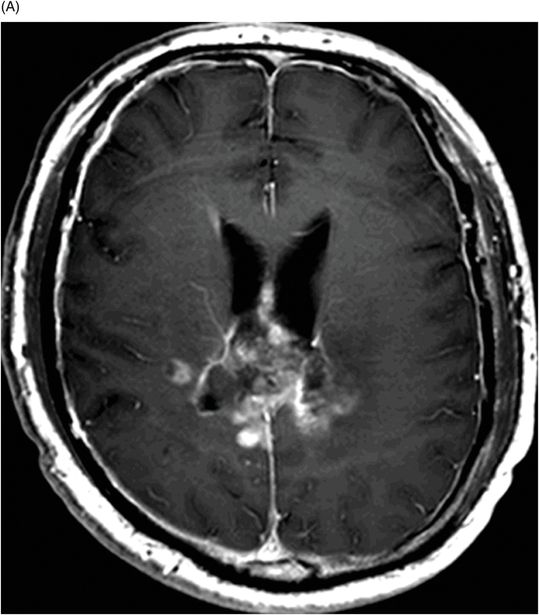
(A) Axial postcontrast T1WI and (B) Axial FLAIR image through the splenium of the corpus callosum (40 days after completion of concurrent TMZ and radiotherapy).

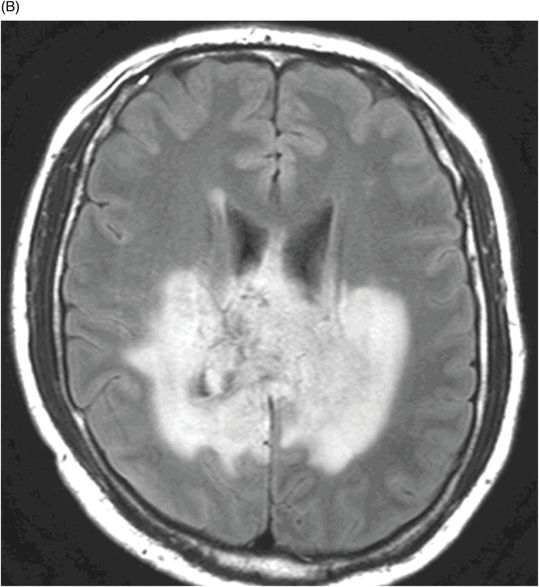
(A) Axial postcontrast T1WI sequence and (B) Axial FLAIR image through the splenium of the corpus callosum (90 days after completion of concurrent TMZ and radiotherapy).

Pseudoprogression due to Chemoradiation
Primary Diagnosis
Pseudoprogression due to chemoradiation
Differential Diagnosis
True tumor progression
Imaging Findings
Fig. 93.1: (A) Axial postcontrast T1WI through the splenium of the corpus callosum demonstrated a large surgical cavity involving the right of the posterior parietal lobe and the corpus callosum. There is significant residual tumor in the splenium of the corpus callosum. (B) Axial FLAIR image through the same level demonstrated minimal abnormal FLAIR signal beyond the margin of the enhancing component of the tumor. Fig. 93.2: (A) Axial postcontrast T1WI sequence obtained little more than one month after completion of the concurrent chemoradiation demonstrated significant enlargement of the enhancing component of the tumor. (B) Axial FLAIR demonstrated enlargement of the abnormal, peri-enhancing, hyperintense FLAIR areas as well. Fig. 93.3: (A) Three-month follow-up scan demonstrates significant improvement of both the enhancing component as well as (B) the FLAIR peritumoral abnormal hyperintense areas.
Discussion
Significant worsening of the enhancing component and the peri-enhancing FLAIR abnormality of a tumor within three months of completing concurrent chemoradiation in a GBM patient with GBM with hypermethylated MGMT gene promoter region is highly suggestive of pseudoprogression (PP). Follow-up scans demonstrating significant improvement of the enhancing component as well as improvement of the peri-enhancing FLAIR hyperintense areas, without therapy changes, confirms the diagnosis of PP, and rules out the possibility of true tumor progression.
Pseudoprogression can be defined by worsening of the enhancing portion of the previously treated tumor and peritumoral FLAIR abnormality in the absence of increased tumor activity. It can be seen in up to one-third of the GBM patients treated with concurrent TMZ and radiotherapy (Stupp protocol). As the name suggests, the worsening of apparent imaging abnormalities improves over time, as the underlying mechanism originates from extensive brain injury due to chemoradiation, rather than tumor proliferation. Although PP can be seen in patients treated exclusively with radiotherapy, it is more commonly seen in patients treated with combined TMZ and radiotherapy, typically within three months of completing chemoradiation. Pseudoprogression can occur even six months after chemoradiation is completed. In the literature, the incidence of PP is variably reported as low as 9% to as high as 65%. This variation stems from the use of differing criteria to define PP in terms of either the increased degree of abnormal enhancement or the degree of decreased enhancement on follow-up MRI. In a recently published large prospective study, the incidence of PP demonstrated was approximately 10%.
Epigenetic silencing of the gene encoding one of the DNA-repair proteins, O6-methyl-guanine methyl transferase (MGMT), has been linked to PP. MGMT is responsible for repairing the DNA once it is damaged by radiation and chemotherapy. If the MGMT promoter region is hypermethylated, the gene is silenced and tumor cells are less efficient at repairing DNA damage, particularly if a concurrent chemoradiation regimen is used. In approximately one-third of patients with GBM, the MGMT promoter is not hypermethylated. However, the MGMT promoter is hypermethylated in up to 66% of patients with PP. MGMT promoter methylation status can predict PP in up to 91% if the MGMT promoter is hypermethylated versus only 59% in wild type. MGMT methylation status has prognostic implications as well. In patients whose tumor has a MGMT promoter that is hypermethylated, the time to progression is 21.9 months versus 9.2 months in patients with an unmethylated, wild type MGMT promoter.
Up to 60% of PP patients do not have any worsening of clinical symptoms. However, the remaining 40% of patients may develop new seizures, signs of increased intracranial pressure, or rarely, focal neurologic deficit. On imaging, there is enlargement or worsening of the enhancing component as well as the peritumoral abnormal T2 hyperintense areas of the tumor, as compared to the immediate, baseline postoperative MRI. According to RANO criteria, any abnormal enlargement of the enhancing component of the tumor within three months of completing chemoradiation is considered PP; therefore, no change in management is implemented, in the absence of any new enhancement or enhancement outside the radiation field. However, this three-month criterion has been questioned recently.
Diffusion and perfusion imaging may be complementary as PP typically demonstrates increased ADC value on DWI and low rCBV on perfusion imaging in most cases; however, exception to this rule has been reported. A neuroradiologist can comfortably diagnose predominant tumor recurrence verses predominant PP; however, diagnosis is challenging if there is an equal mixture of these two conditions. In a recent study, it was shown that perfusion MRI with ferumoxytol is more sensitive for differentiating between these two.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








