Axial CT scan of the head without contrast through the level of occipital lobes.
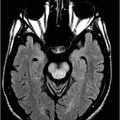
Axial T1WI MRI with contrast through the level of occipital lobes.

Microcystic Meningioma
Primary Diagnosis
Microcystic meningioma
Differential Diagnoses
Typical meningiomas/angiomatous meningioma
Astrocytoma
Metastatic clear cell carcinoma
Epidermoid
Chordoma/chondrosarcomas
Imaging Findings
Fig. 97.1: Axial CT scan of the head, without contrast, through the level of the occipital lobes demonstrated a large, oval, homogeneously hypodense mass in the right posterior temporal and occipital lobes with mass effect to the right lateral ventricle, without any leftward deviation of the posterior falx. The hypodensity is more like CSF than fat. Fig. 97.2: Axial T1WI image, without contrast, through the same level demonstrated a large hypointense mass in the right posterior temporal and occipital lobes, with numerous intratumoral cysts associated with mass effect. Fig. 97.3: Axial T2WI of the mass better demonstrated the cystic nature of the mass. The mass effect to the ventricle is well appreciated. It is to be noted that there is no peritumoral abnormal T2 signal. Fig. 97.4: Axial T1WI with contrast demonstrated heterogeneous, marked enhancement of the septi surrounding the hypointense cysts resulting in a honeycomb appearance of the dural-based mass. Fig. 97.5: Selective digital subtracted angiography image demonstrated tumoral blush from external carotid artery injection.
Discussion
Although the lesion is homogeneously hypodense on unenhanced CT scan images, the microcystic appearance on all the MRI sequences is diagnostic of microcystic meningioma (MM). The diffusion image demonstrated T2 shine-through effect (not shown), further suggesting the presence of microcysts in the tumor. On external carotid angiography, there was a prominent tumoral blush in the arterial phase, suggesting intense vascularity and further supporting the diagnosis of MM.
The persistent headache with visual abnormality is due to a posteriorly located mass close to the visual pathway. The mass is homogeneously hypodense on unenhanced CT scan. This appearance is non-specific and can be seen in any cystic lesion of the brain, such as astrocytomas, and benign intraparenchymal cysts, such as neuroepithelial or epidermoid cysts. Neuroepithelial cysts are usually incidental. No diffusion restriction (not shown) was present to indicate that the lesion was epidermoid. Although it is hard to delineate intra- versus extra-axial masses on T2-weighted sequence, dural-based enhancement is better appreciated on the postcontrast scan, suggesting that the tumor is extra-axial. Typical meningiomas are not cystic. High signal on T2-weighted sequence with heterogeneous enhancement can be seen in chordoma/chondrosarcomas; however, the location of the mass in this patient is not a known location for these types of tumors. Chondroma can have a similar appearance, but usually the chondroid matrix is appreciated on non-contrast head CT images. Furthermore, chondromas demonstrate minimal peripheral enhancement, rather than the honeycomb-type enhancement noted in this patient’s images. The absence of any known malignancy rules out the possibility of metastasis. The angiomatous variant of meningioma may demonstrate a similar extent of edema of the adjacent brain. However, it should not be confused with the MM, as the angiomatous variant typically demonstrates intense homogeneous tumor enhancement due to presence of an excessive amount of variably sized blood vessels, as compared to tumor cells.
Meningiomas account for about 24–30% of all primary intracranial tumors. Meningiomas typically occur in middle-aged and older adult patients with a peak in the sixth and seventh decades. However, meningiomas also occur in pediatric and elderly populations. Meningiomas typically affect females more than males. Most meningiomas involve the cerebral convexities, along the falx and venous sinuses. Other common sites include the olfactory groove, sphenoid ridges, sellar/parasellar regions, optic nerve sheath, petrous ridges, tentorium, and posterior fossa.
Most meningiomas are benign, WHO grade 1 lesions and grow slowly over time. The presenting symptoms are secondary to mass effect to the adjacent brain. Specific neurologic deficits depend upon the location of the tumor. Headache and seizures are other common presentations.
On imaging, most meningiomas are usually iso- to hyperdense on non-contrast CT scan images, and typically demonstrate intense enhancement with contrast on both CT and MRI. Frequently there is thickening and enhancement of the adjacent dura, the dural tail sign, which may not always represent extension of tumor. This can be reactive as well. This typical imaging appearance may not be present in some histologic subtypes of meningiomas.
Many histologic subtypes of meningiomas have been described. Microcystic meningioma is a rare variant of meningiomas with microcystic changes. This variant is typically benign, WHO grade 1. These tumors were originally described by Masson as humid meningiomas, based on their gross morphology. This variant is characterized by cells with thin, elongated processes that surround a pale eosinophilic mucinous fluid – the microcysts. Microcystic meningiomas are more commonly found in the convexity, along the falx cerebri. Although any age group can be affected by MM, they more commonly develop in adults, usually after the fourth decade of life, and are rare in children. Presenting symptoms are similar to other subtypes of meningiomas.
On CT, MM can show iso- to hypodensity and variable patterns of enhancement. Occasionally these tumors can be confused with brain edema because of its hypodense appearance. Hyperostosis of the adjacent bone is common and can be seen in approximately one-half of patients. Edema of the adjacent brain is commonly seen. The variable and heterogeneous patterns of enhancement, disproportionate edema of the adjacent brain, and lack of dural tail often lead physicians to confuse MM with aggressive lesions.
On MRI, typical MM demonstrates low signal on T1-weighted and high signal on T2-weighted images, with contrast enhancement in the majority of the cases. Owing to high mucinous fluid content, MM can follow CSF signal intensity on precontrast T1- and T2-weighted sequences. The presence of a broad-based cystic tumor in a typical location for a meningioma may be helpful in the diagnosis of a MM. Higher incidence of edema is another characteristic and common MRI finding of MM, compared to typical presenting meningiomas. Significant edema of adjacent brain is seen in up to 87.5% of patients with meningiomas and may be seen even in small lesions. Reasons for the disproportional edema are not fully understood and it has been suggested that high levels of vascular endothelial growth factor (VEGF) expression and cortical penetration with arachnoid disruption may play a role in edema formation. Variable enhancement pattern on MRI has been described in MM. Some lesions may present with only peripheral enhancement, which may have a honeycomb-like enhancement pattern, or may appear as a large, heterogeneously enhancing mass with both solid and cystic components.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree