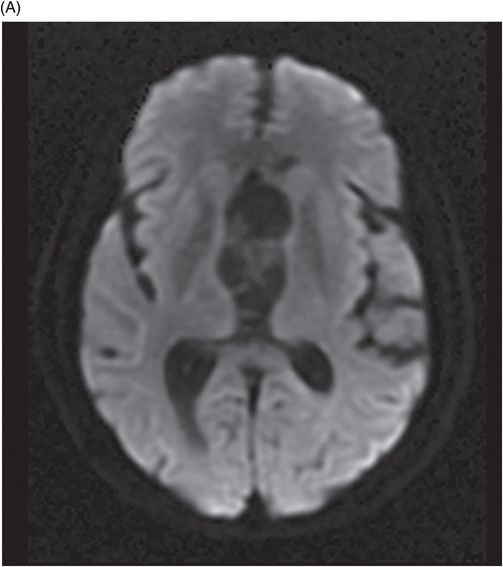
Axial T2WI of the head at the level of third and lateral ventricles.
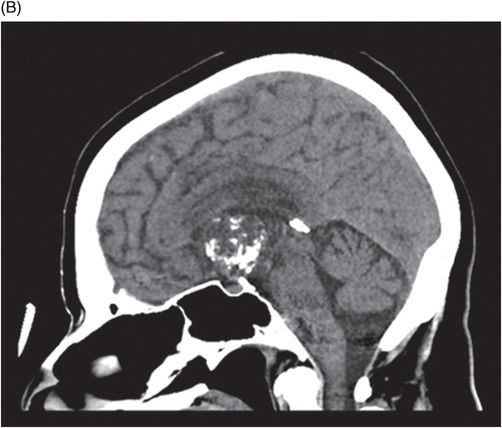
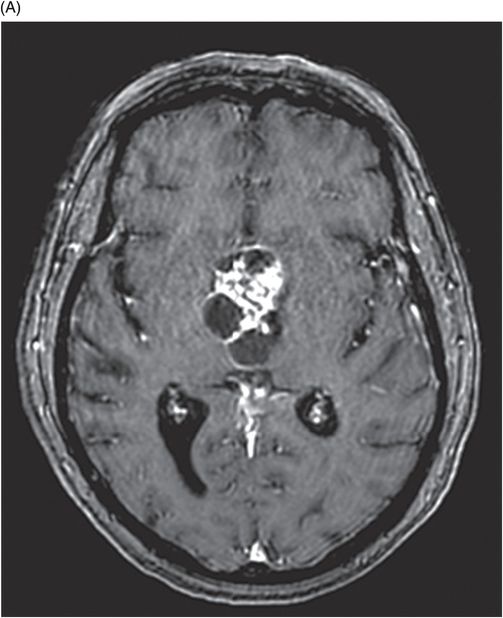
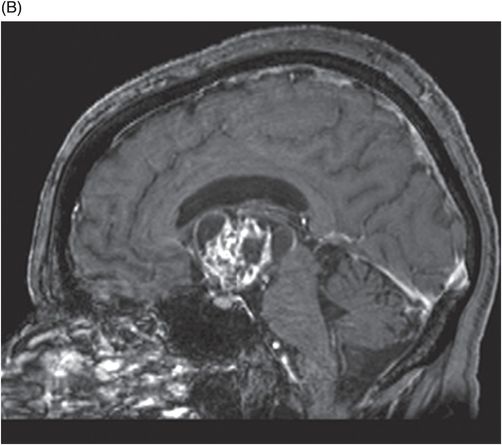
(A) Axial postcontrast image through the level of third and lateral ventricles. (B) Midsagittal postcontrast image.
Third Ventricular Craniopharyngioma
Primary Diagnosis
Third ventricular craniopharyngioma
Differential Diagnoses
Colloid cyst
Germ cell tumor
Glioma
Lymphoma
Chordoid glioma
Choroid plexus papilloma
Imaging Findings
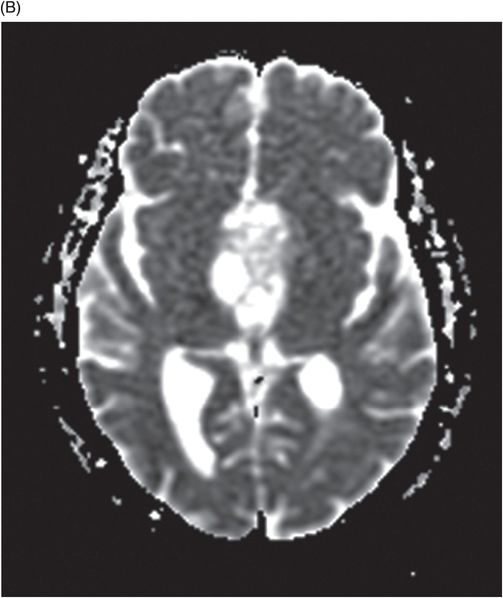
Fig. 99.1: (A) Axial non-contrast and (B) Sagittal reformatted CT images of the head showed a dense, heterogeneous, solid-cystic lesion with foci of calcification occupying the third ventricle. Fig. 99.2: Sagittal T1WI of the head. Fig. 99.3: Axial T2WI of the head showed a solid-cystic, mixed signal intensity lesion in the third ventricle. Fig. 99.4: (A) There is no evidence of diffusion restriction or corresponding changes on ADC map (B). Fig. 99.5: (A) Axial postcontrast and (B) Midsagittal postcontrast images showed heterogeneous enhancement. The pituitary gland is seen separate from the lesion. However, the optic chiasm is encased by the mass.
Discussion
Findings of a mixed signal intensity lesion with heterogeneous enhancement (solid portion of lesion), in conjunction with history of a slowly progressive, symptomatic headache and visual disturbances, are typical of a craniopharyngioma. Craniopharyngiomas are often mixed solid and cystic lesions. Cystic areas may be iso-, hyper-, or hypointense, relative to brain tissue, on T1-weighted sequences with thin enhancing wall. The solid components of the lesion enhance heterogeneously. Calcifications are characteristic in suprasellar craniopharyngiomas, but are rarely observed in intraventricular craniopharyngiomas. If present, calcifications usually demonstrate susceptibility effects on gradient echo sequence.
Common differential diagnoses for a third ventricular craniopharyngioma include colloid cyst, germ cell tumor, glioma, lymphoma, chordoid glioma, and choroid plexus papilloma. Colloid cysts are usually located in the roof of the third ventricle, are often hyperdense on non-contrast CT scan, hyperintense on T1, and iso- to hypointense on T2WI. However, the lack of calcification and enhancement in colloid cysts excludes this entity as the primary diagnosis. Hypothalamic germ cell tumors can arise from the infundibular stalk or from the floor of the third ventricle. They feature intense, homogeneous enhancement but lack cystic and calcified components, in contrast to the heterogeneous enhancement of the solid portion of craniopharyngiomas. Although hypothalamic glial tumors may have solid and cystic components, they feature marked homogeneous enhancement but lack calcification. Lymphomas are solid, avidly enhancing tumors and are hypointense on T2WI with diffusion restriction, uncharacteristic of craniopharyngiomas. In adults, chordoid glioma has a predominantly solid component, and enhances significantly. Although a few cases of choroid glioma report the presence of cystic components and necrosis, the presence of calcification is uncommon. The third ventricle is an unusual location for choroid plexus papilloma, whose lesions feature cauliflower morphology, may contain flow voids, and enhance avidly, not seen in craniopharyngiomas.
Craniopharyngiomas are benign, mixed epithelial tumors derived from the squamous epithelial remnants of Rathke’s pouch in the subpial space. They may arise at any point along the pituitary-hypothalamus axis, from the pituitary gland to the floor of the third ventricle. Rare ectopic locations include the third ventricle, nasopharynx, pineal gland, sphenoid sinus, and the clivus.
Craniopharyngiomas account for 2.5–4% of all intracranial tumors. They present a bimodal age distribution, with peak incidence between 5 and 14 years and 50 and 74 years of age. Intraventricular craniopharyngiomas occur primarily in the adult age group. No gender preponderance has been identified. Headache, nausea, and vomiting are common presenting complaints in intraventricular craniopharyngiomas, due to obstructive hydrocephalus. Other clinical symptoms include hypothalamic, amnesic, behavioral, and gait disturbances, seen more frequently than in their extraventricular counterparts.
Two main histologic types of craniopharyngiomas exist, adamantinomatous and squamous-papillary. Intraventricular craniopharyngiomas are predominantly of the squamous-papillary type, which tend to be smaller, round in shape, and primarily solid. When cysts are present, they are more often hypointense on T1WI. Overall, squamous-papillary craniopharyngiomas have a more heterogeneous appearance and enhancement pattern. In contrast, adamantinomatous craniopharyngiomas typically display multilobulated borders, with prominent cystic components that demonstrate hyperintense contents on T1WI.
Suprasellar craniopharyngiomas may involve the third ventricle, to various degrees, without truly being intrinsic third ventricle craniopharyngiomas (ectopic tissue in the third ventricle from which a craniopharyngioma arises). A suprasellar craniopharyngioma may be wholly extraventricular, expand in the chiasmatic cistern, and push the floor of the third ventricle superiorly, mimicking an intraventricular position. Identification of the intact floor of the third ventricle overlying the lesion permits differentiation from a true intraventricular craniopharyngioma. Craniopharyngiomas may initially develop in the suprasellar compartment, but subsequently invade the third ventricle through the floor. Craniopharyngiomas may also arise directly from the floor of the third ventricle and expand into the ventricle. An intrinsic third ventricle craniopharyngioma is located entirely in the ventricle, and an intact floor can be identified on imaging. The hypothalamus is usually below the level of the craniopharyngioma, which is another useful characteristic for identifying the intraventricular location of the tumor. Making this distinction is important for surgical planning.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree