Chapter 1 A Multidisciplinary Approach to Cancer
A Radiologist’s View
Introduction
Imaging plays a central role in the care of patients with cancer. Subsequent chapters deal with some of the specifics regarding the use of imaging in the multidisciplinary environment, such as tumor staging, lesion respectability, and treatment-related complications. Many clinical decisions are influenced by the results of imaging studies, and the radiologist must, therefore, be a central member of the multidisciplinary care team. The significant role of imaging can be seen in the continued growth in the numbers of scans performed each year, particularly in the advanced imaging studies such as x-ray computed tomography (CT), magnetic resonance imaging (MRI), and positron-emission tomography with x-ray CT (PET/CT).1
Multidisciplinary Cancer Imaging: The Role of the Radiologist
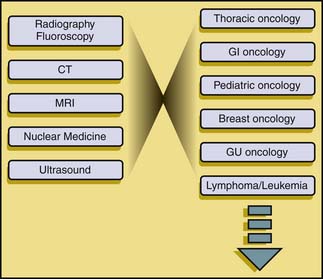
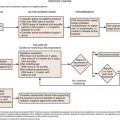
This increase in the breadth and complexity of radiology and nuclear medicine has necessitated a shift in practice patterns at many sites. In order to effectively function in the multidisciplinary environment of an academic cancer hospital, radiologists have needed to specialize. Radiology specialization has traditionally been either by modality (e.g., ultrasound, CT) or by system (e.g., body imaging, neuroradiology, thoracic radiology). The clinical specialties, conversely, have trended toward specialization according to disease. At M. D. Anderson Cancer Center, there are multidisciplinary care teams devoted to the care of patients with various malignancies. Each care team is composed of multiple members from various disciplines, including surgery, medical oncology, and radiation therapy. In order to adapt to the multidisciplinary paradigm, imaging has had to adapt from the traditional modality-based and system-based approaches to a disease-oriented framework (Figure 1-1).
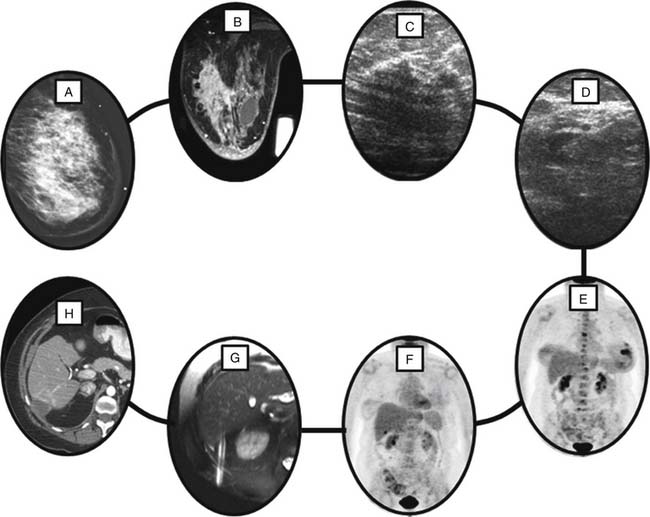
The challenge for the radiologist is that the diagnostic imaging within each of the multidisciplinary centers crosses the boundaries between traditional imaging specialties. To take an example, a woman with newly diagnosed, locally advanced breast cancer presents for workup (Figure 1-2). Breast imaging plays a central role in her evaluation, starting with mammography and moving to breast ultrasound and/or MRI as needed. Her pathologic diagnosis and tumor genetic markers will likely be established by a guided biopsy procedure. Further imaging workup of such a patient may include a contrast-enhanced CT of the chest and abdomen or a radionuclide bone scan for detection of osseous metastatic disease. The workup may stop there, but depending on many clinical factors such as signs and symptoms and serum tumor markers, additional imaging may be requested including PET/CT with fluoro-2-deoxy-D-glucose (FDG), or brain MRI.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree