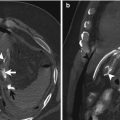
Fig. 8.1
Diverticular microperforation: little amount of free air associated with thickening of the sigmoid wall, diverticular pouch and perivisceral signs (mild, fuzzy hyperdensity and stranding of pericolic tissue, arrows)
8.3 Spectrum of MDCT Finding
The diagnosis of acute diverticular perforation requires the presence of the diverticula usually associated with circumferential thickening of a long segment of the colonic wall and with signs related to a cellulitic process into the perivisceral tissue: hyperdensity (sometimes very slight and fuzzy) and increase of perivisceral lymphatics and vessels presenting as hyperaemia and stranding of the pericolic fat are the first signs of inflammation eventually associated with thickening of the retroperitoneal or peritoneal folds [6].
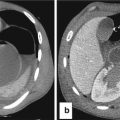
Phlegmon may appear, in proximity of the inflammation site, as a little mass, round or ovular, that is hyperdense (from +15 to +35 HU), enhanced after MDCT and surrounded by slightly dense tissue (Fig. 8.2).
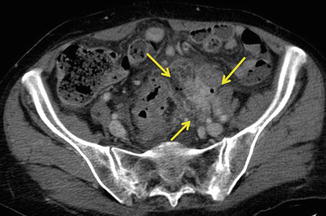
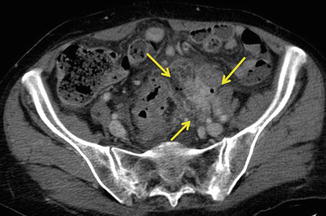
Fig. 8.2
Phlegmon, (arrows): hyperdense tissue (from +15 to +35 HU), enhanced after MDCT contiguous to a diverticulitis site and microbubbles of free air
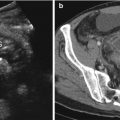
A fluid, hypodense, collection with surrounding thickened, hyperdense inflammatory wall due to an abscess may be more frequently found. Small air-bubble or air-fluid levels may be contained in the centre of the collection (Fig. 8.3).
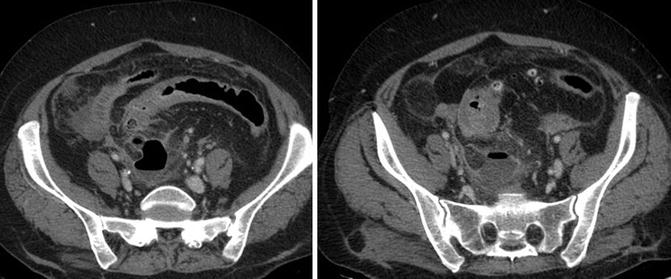
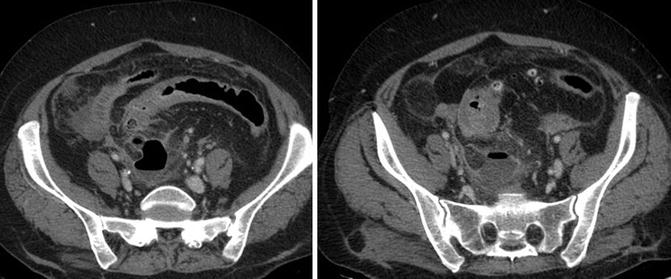
Fig. 8.3
Parasigmoid abscess: hypodense fluid collection, contained in the mesosigma, with an air-fluid level, and delineated by thickened, hyperdense inflammatory rim
The presence, the grade of thickness and of post-contrastographic density and the presence of septa and air-bubble levels are related to the grade of the abscess maturation.
The spectrum of MDCT findings of diverticulum perforation depends on the site of the lesion and on the involvement of the retroperitoneal or peritoneal spaces.
The most frequent perforation site is the sigmoid colon; the transverse colon accounts for approximately 18 % of perforations, whereas perforation of the cecum and the right colon is rare (only 5 % of perforations). The sigmoid mesocolon and thus the subperitoneal space are most frequently involved but, due to the continuity of the spaces beneath the posterior parietal peritoneum and abdominal pelvic walls with the root of the sigmoid mesentery and pelvic ligaments, a retroperitoneal or peritoneal extension of the process may happen.
When perforation is associated with an abscess formation, the abscess can be confined to the pelvis or can extend far into the abdomen.
When the peritoneal cavity is involved, the abscessual collection is always well delimited by thickened peritoneal folds presenting as a dense and uniform capsule.
In the sigmoid perforation MDCT has excellent contrast resolution to detect the presence of small amounts of free extraluminal air in close proximity to the intestinal wall thickening or centred within paracolic inflammatory tissue in the pericolic space. Extraluminal air can always be detected with adequate window setting even if there are only small bubbles [7].
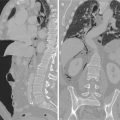
In sigmoid free perforation a greater amount of air can diffuse into the subperitoneal space, the retroperitoneal space of the pelvis, of the abdomen and also, through the diaphragmatic hiatus, of the thorax and of the neck resulting in pneumomediastinum and cervical emphysema [8] (Fig. 8.4).


Fig. 8.4
Retroperitoneum from diverticular perforation: free air in the mesosigma and perirenal space
In case of colonic perforation (left and right colon), air bubbles are preferentially located in the pericolic fat (contained perforation) (Fig. 8.5) [7].
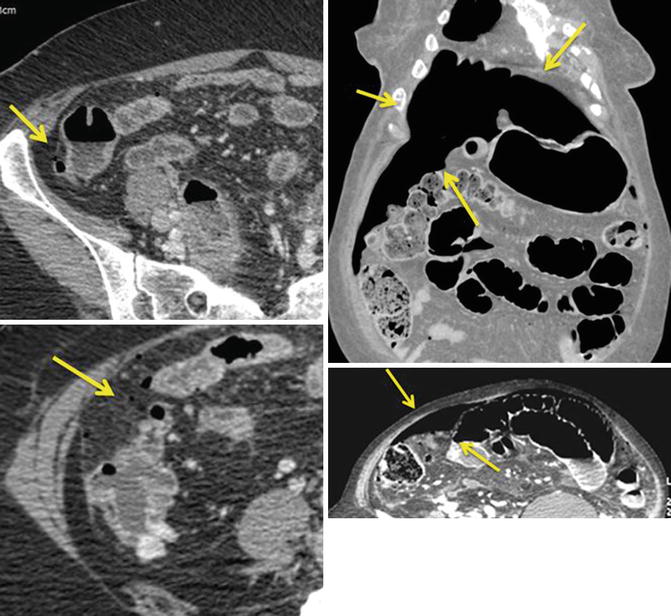
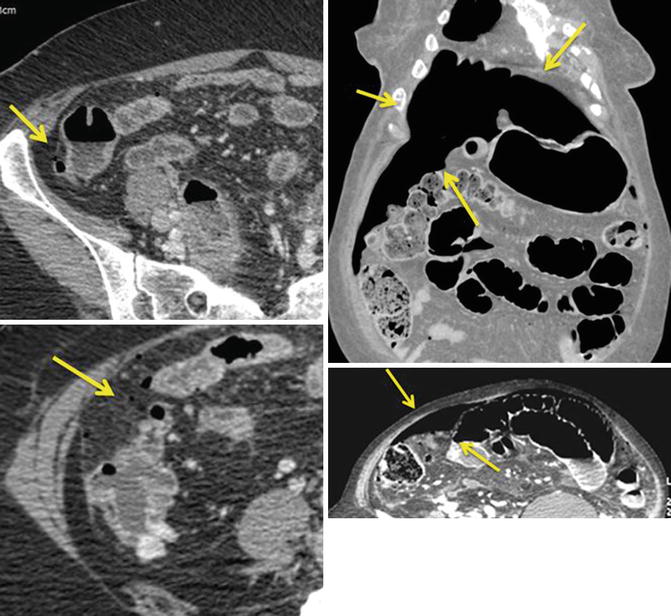
Fig. 8.5
Colonic perforation: evidence of pneumoperitoneum and air bubbles preferentially located in the pericolic fat (arrows)
In case of free perforation into the peritoneal cavity, the air rapidly reaches the most antideclive position usually in the anterosuperior part of the involved peritoneal recess (Fig. 8.4).
The risk of an adverse outcome is highest if the perforation of the diverticular or of the abscess wall allows faecal discharge in the peritoneum. The presence of spilled faeces or “dirty mass” in the lower abdomen is a specific indicator of colonic perforation [9].
A CT features an extravasated faeces that is a low-attenuation soft tissue mass containing small air bubbles (Fig. 8.6).
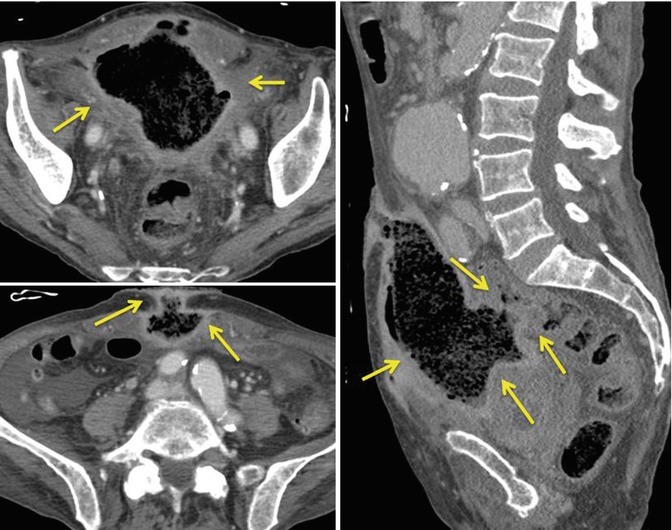
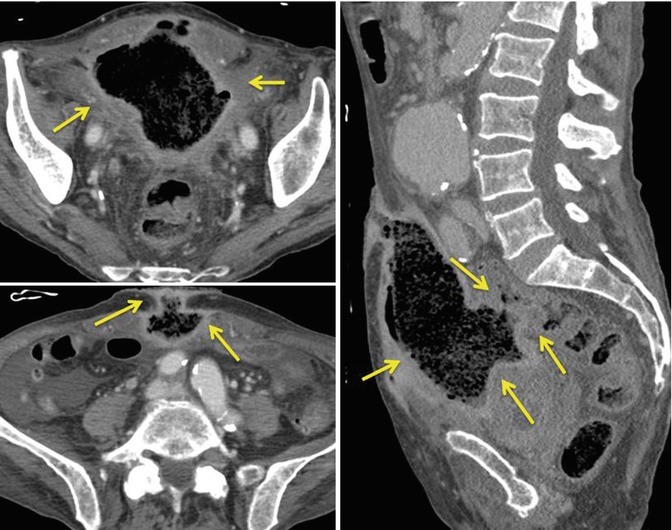
Fig. 8.6
Dirty mass (faecal abscess, arrows) fistulized to the abdominal wall
The spread of the inflammatory process into adjacent organs may have several clinical presentations such as hydronephrosis, psoas abscess, abdominal wall abscess [10] and spondylodiscitis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree