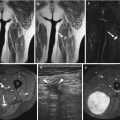
Fig. 12.1
(a–d) Subcutaneous lipoma in the left thigh overlying gracilis (*). (a) Ultrasound. (b) Axial SE T1-weighted MR image. (c) Axial fat-suppressed T2-weighted MR image. (d) Coronal SE T1-weighted MR image. There is a left thigh medial mass within the subcutaneous tissue (large arrows), isoechoic on ultrasound (a) and with SI similar to adjacent subcutaneous fat on all pulse sequences (b–d). There are multiple thin septa (small arrowheads) within the mass, echogenic on ultrasound (a) and low SI on T1-weighted images (b and d)
12.2 Benign Adipocytic Tumors
The benign adipocytic tumors represent a very common and varied group, and according to the most recent World Health Organization’s Committee for the Classification of Soft Tissue Tumors (2013), nine distinct entities are distinguished [26]: lipoma, lipomatosis, lipomatosis of nerve, lipoblastoma, angiolipoma, myolipoma of soft tissue, chondroid lipoma, spindle cell/pleomorphic lipoma, and hibernoma. However, this classification does not distinguish true neoplasms, hamartomatous processes, or simple overgrowth of fat, mainly because the differentiation is devoid of any clinical consequences. Myolipoma of soft tissue, extrarenal angiomyolipoma, and extra-adrenal myelolipoma are rare predominantly intra-abdominal lipoma variants, which are not discussed in this chapter, which focuses on truncal and extremity masses.
12.2.1 Lipoma
Microscopically a lipoma is usually a well-circumscribed and encapsulated mass composed of mature fat (adipocytes) differing very little from the surrounding fat. Although lipomas are well vascularized, this feature may not be readily apparent owing to vascular compression caused by the distended adipocytes.
Lipoma is the most common mesenchymal tumor, and in a review of 18,677 benign soft tissue tumors, lipoma and lipoma variants were the most common group, representing 16 % of all lesions [44]. Lipomas generally affect patients in the fifth to seventh decade of life, more frequently in obese people but with no definite sex predilection [21, 44].
Lipomas can be superficially or deeply located (subcutaneous or deep lipomas); they occur most commonly in the subcutaneous tissue and more rarely in the deep soft tissue. Subcutaneous lipomas are most frequently found in the upper back and neck, shoulder, abdomen, and proximal portions of the extremities, while the less common deep lipomas tend to be larger and less circumscribed than the superficial ones; please see Sect. 12.2.1.1 later [31, 48, 49].
Symptoms depend on the location and size of the tumors. A lipoma typically appears as a slowly growing, painless mass, but rapidly growing lipomas have been reported. Pain is rare but may occur as a consequence of neurovascular compression depending on the location and relationship to adjacent structures. Subsequent symptoms such as carpal or tarsal tunnel syndrome and chronic lower extremity deep vein thrombosis due to femoral vein compression have been reported.
Superficial lipoma manifests usually as a small mass, less than 5 cm, rarely exceeding 10 cm [49]. Subcutaneous lipomas are easily diagnosed at clinical examination, without the need for radiographic evaluation. The radiograph may occasionally demonstrate a radiolucent soft tissue mass and rarely osseous deformity by mass effect.
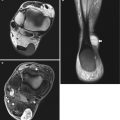
The most frequent sonographic appearance of lipoma is that of an elliptical, compressible, homogenous, and well-defined mass parallel to the skin surface. They are intrinsic multiple echogenic lines (Figs. 12.1 and 12.2) which relate to fibrovascular septi which can often show linear blood flow on Doppler interrogation [50]. The echogenicity can vary but is usually hyperechoic compared to adjacent fat; however, the homogenous nature is the most important reassuring feature [1, 50].
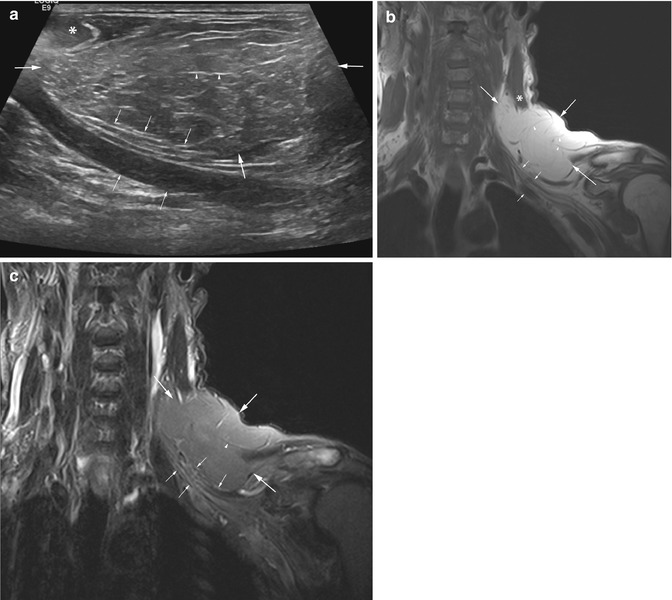
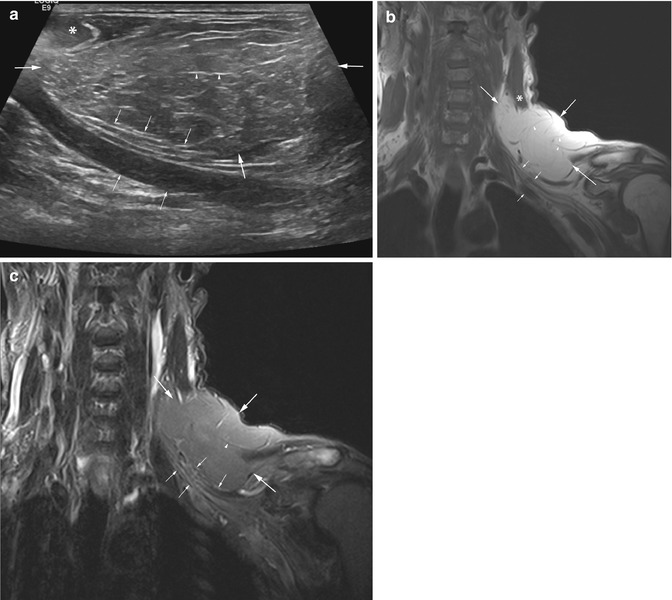
Fig. 12.2
(a–c) Lipoma of the left neck and supraclavicular region with left arm symptoms. (a) Ultrasound. (b) Coronal SE T1-weighted and (c) fat-suppressed T2-weighted MR images. The lipoma is intramuscular and subcutaneous. Ultrasound examination shows a homogenous, hyperechoic mass (large arrows) (a). On MRI the mass is homogeneous and SI is equal to that of subcutaneous fat on different pulse sequences (b–c). All images show sternocleidomastoid muscle (*), thin septi (arrowheads), and mass effect by the lipoma on the brachial plexus and subclavian vessels (small arrows)
On CT and MR images, lipomas also present as homogeneous, well-circumscribed, and encapsulated masses of fatty nature, without diffuse enhancement after intravenous contrast administration. The differentiation between the superficial lipoma and the surrounding fat may be difficult due to their similarity on density and SI (Fig. 12.1). Regular, thin septations can be seen both on CT and MR images [47, 75]. The septa appear as soft tissue density strands on CT scans and as low-intensity strands on T1-weighted MR images, which may become hyperintense on T2-weighted MR images (due to the blood vessels within). The width of these septa can be unmeasurable, with a slight enhancement after intravenous contrast administration, which is more clearly demonstrated on fat-suppressed T1-weighted MR images [38].
Lipomas composed of tissue other than adipose tissue may differ from the classic sonographic, CT, or MR imaging appearance (see Variants of Lipoma). Non-tumor changes such as calcification, mechanical edema in superficial lipomas, or intrinsic fat necrosis should be considered rather than always assuming sarcomatous change (Figs.12.3, 12.4, and 12.5) [71].

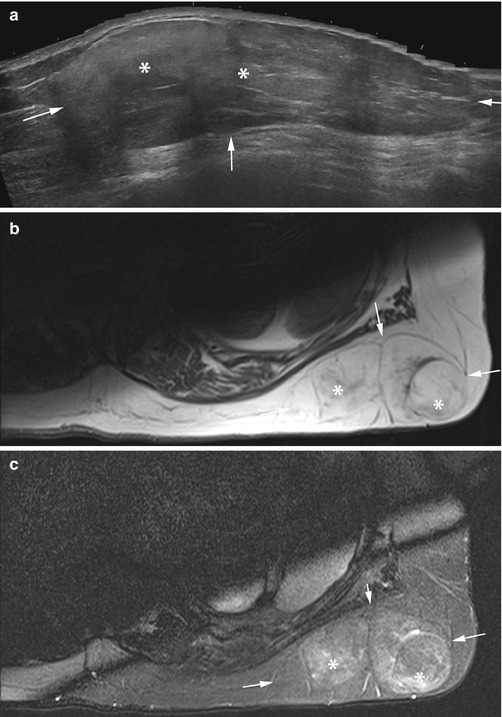


Fig. 12.3
(a–c) Subcutaneous lipoma of the neck. (a) Ultrasound. (b) Sagittal SE T1-weighted MR image. (c) Sagittal STIR image. The distal aspect of the mass (*) is homogenous on ultrasound and fat SI on MRI. The proximal mass (arrowheads) is heterogeneous on ultrasound (a) and edematous on MRI but with no nodular mass (b–c). Histology confirmed lipoma, MDM2 negative, and proximal fat necrosis
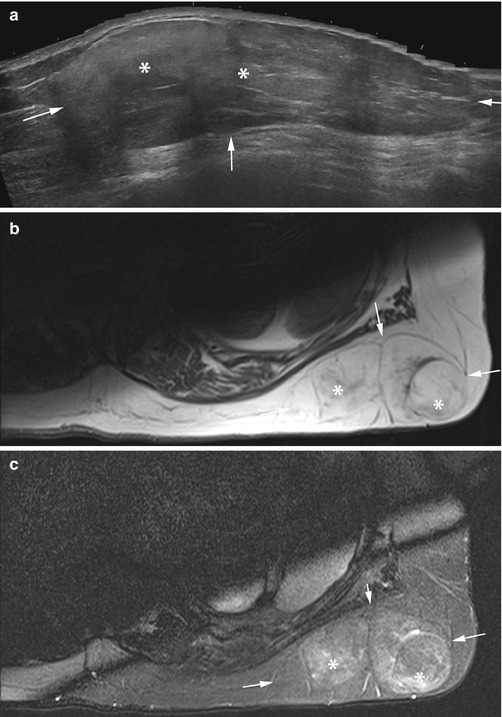
Fig. 12.4
(a–c) Subcutaneous lipoma of the back. (a) Ultrasound. (b) Axial SE T1-weighted MR image. (c) Axial fat-suppressed SE T2-weighted MR image. The majority of the mass (arrows) is homogenous on ultrasound and fat SI on MRI. The superficial aspects of the mass (*) are slightly heterogeneous on ultrasound (a) and edematous on MRI but with no nodular mass (b–c). Histology confirmed lipoma, MDM2 negative, and congested edematous fat superficially

Fig. 12.5
(a–c) Intramuscular lipoma of the left gluteus medius thigh. (a) CT scan. (b) Axial SE-T1-weighted MR image. (c) Axial TSE T2-weighted fat-suppressed MR image. Large mass in gluteus medius muscle (arrows) of the left thigh with low attenuation values on CT (a). The signal intensity on different MR sequences equals that of fat (b, c). Note the presence of small focus of higher-density calcification on CT (a) and lower SI (b, c) on MRI (small arrow)
12.2.1.1 Intramuscular and Intermuscular Lipoma
On gross inspection of intramuscular and intermuscular lipomas, fat has replaced the muscle tissue. Microscopically mature lipocytes infiltrate the muscle fibers, which may show some degree of atrophy. Widespread invasion of one or more muscles may occur. Intramuscular lipoma has also been referred to as “infiltrating lipoma” due to its frequently infiltrative aspect on histological examination. Intramuscular lipoma is more frequent than the intermuscular variant, and it can affect both the muscular and intermuscular tissues [5, 47].
Intramuscular lipoma affects all age groups, mostly occurring in patients over 40 years of age, and, although rare, it has also been reported in children [35, 49]. Most authors have described a male predominance. These lesions tend to involve most commonly the large muscles of the extremities, especially of the thigh, trunk, shoulder, and upper arm [31, 49].
The clinical picture is one of a painless, slow-growing lesion, but occasionally the symptoms may be very different from those of the common subcutaneous variety, and intramuscular lipoma may present as a rapidly growing mass with nerve entrapment (Figs.12.2 and 12.6). The size of the lipoma varies from a small mass of less than 3 cm to more than 20 cm in diameter [31, 49, 57]. The imaging findings in these heterotopic lipomas are basically the same as in other lipomas [57]. Although most of the intramuscular lipomas are well-defined lesions on CT or MR images, they also may show infiltrative margins if they extend between the muscle fibers, corresponding to the infiltrative type of intramuscular lipoma (Figs.12.6 and 12.7) [35, 47, 57]. On CT and on MR images, some intramuscular lipomas are septate, inhomogeneous masses, with tissue attenuation and interspersed regions of decreased signal on T1- and T2-weighted images, which probably represent either muscle or fibrous tissue within the mass [57] (Fig. 12.8). Matsumoto et al. have reported the MR findings of 17 cases of intramuscular lipoma, 12 being homogeneous and the remaining 5 inhomogeneous with intermingled muscle fibers that were isointense with normal muscle on both T1- and T2-weighted images [57]. On ultrasound the masses usually appear homogenous, but the muscle fibers can cause reverberation artifact obscuring intrinsic detail unless the probe position is altered (Fig.12.8c).


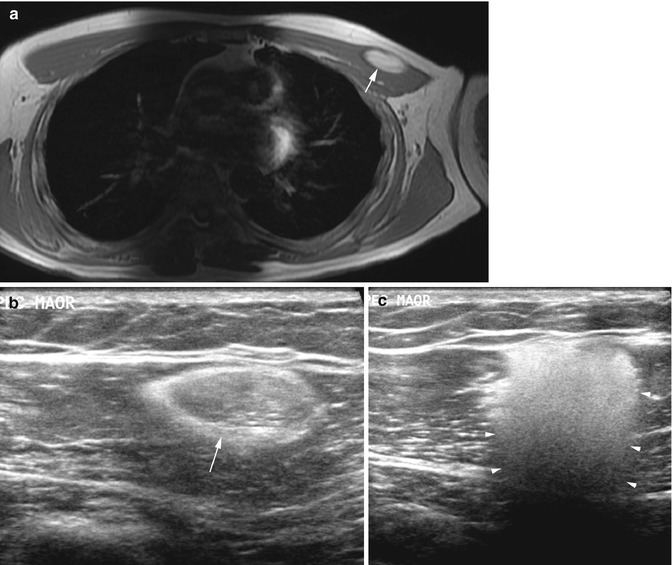

Fig. 12.6
(a–c) Intramuscular lipoma of the right arm. (a) Ultrasound. (b) Axial SE T1-weighted MR image. (c) Axial fat-suppressed SE T2-weighted MR image. On ultrasound the mass is homogenous and hyperechoic (a), and the signal intensity on different MR sequences equals that of fat (b, c). The radial neurovascular bundle, (large arrows) septi (small arrowheads), and relationship to brachioradialis (*) are shown with both techniques, but MRI gives a better overview and better definition of the whole mass especially the deeper aspect (large arrowhead)

Fig. 12.7
(a–c) Intramuscular lipoma of left serratus anterior. (a) Axial SE T1-weighted MR image. (b) Axial fat-suppressed SE T2-weighted MR image. (c) Coronal SE T1-weighted MR image. The mass (arrows) is homogenous with a signal intensity on all sequences equal to fat (a–c). The deeper aspect is more ill-defined due to interdigitation with the muscle fibers (*) but still benign in appearance
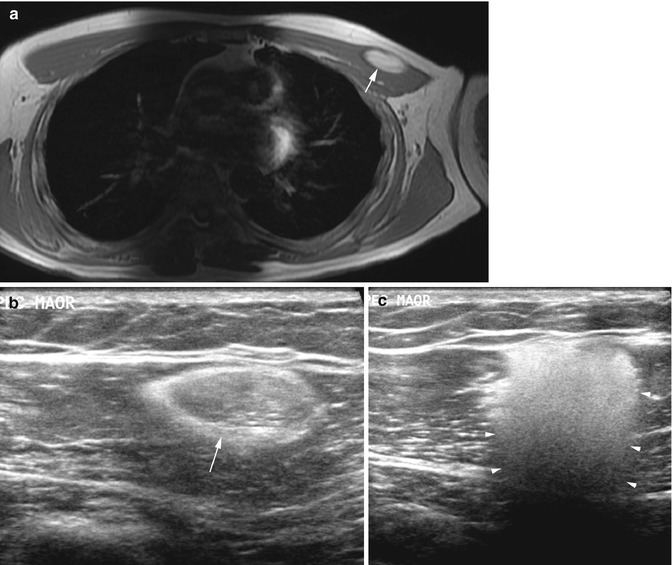
Fig. 12.8
(a–c) Intramuscular lipoma of left pectoralis major. (a) Axial SE T1-weighted MR image. (b, c) Ultrasound images. On MRI (a) and ultrasound (b) the mass is homogenous (arrow). Careful ultrasound technique is required as angulation can result in reverberation artifact (arrowheads) (c) due to the multiple muscle fibers within the lipoma
Although the absence of contrast enhancement and unilobularity are useful signs in the differential diagnosis of intramuscular lipoma from well-differentiated liposarcoma/atypical lipomatous tumor (Table 12.1), these signs are not 100 % reliable [68]. This makes the differential diagnosis with well-differentiated liposarcoma difficult radiologically, and this may also extend to histological examination [57]. Additional cytogenetic analysis is often the crucial test for confirming or excluding sarcomatous change [63]. Please see Sect. 12.3.1 later.
Table 12.1
Differential diagnostic criteria between lipoma and liposarcoma
Lipoma | Intramuscular lipoma | Liposarcoma | |
|---|---|---|---|
Age | Adult (mean 52 years) | Adult | Adult (mean 65 years) |
Location | Superficially located (subcutaneous fat) | Muscle | Muscles/fascias |
Back, shoulder, neck, arm, thigh, abdomen | Thigh, shoulder, arm | Muscle/fascia | |
Thigh, retroperitoneum | |||
Size | <5 cm (80 %) | Frequently >5 cm | Exceptionally <5 cm |
<10 cm (95 %) | |||
Margins | Well defined | Infiltrating or well defined | Usually well defined |
Shape | Uninodular | Uninodular (>85 %) | Multinodular (>90 %) |
Septa or nodules | Absent or <2 mm | Intermingled muscle fibers | Thick (>2 mm) |
Hypo on FS T2-WI | Isointense to muscle | Hyper on FS T2-WI | |
No or weak enhancement | Enhancement rare | Strong enhancement |
12.2.1.2 Multiple Lipomas
Some patients, especially males, may have multiple lipomas, which are grossly and microscopically similar to other lipomas. They occur predominantly in the back, shoulder, and upper arms, sometimes in a symmetrical distribution [31]. A familiar disorder exists, referred to as “familial multiple lipoma” which shows this typical clinical presentation. Associated hyperlipidemia and hypercholesterolemia have been described in some cases [31, 49, 72].
12.2.2 Lipomatosis
Lipomatosis, also known as diffuse lipomatosis, represents a diffuse overgrowth of mature adipose tissue histologically similar to simple lipoma. The fatty tissue extensively infiltrates the adjacent structures and contiguous muscles, leading to deformities and limb asymmetry. The distinction between infiltrating lipoma and lipomatosis can be arbitrary at times, and some authors use the two terms interchangeably [48]. However, lipomatosis implies a more extensive process with diffuse involvement of the subcutaneous and muscular tissue, while the intramuscular lipoma is always confined to a muscle or intermuscular tissue space.
Diffuse lipomatosis is an extremely rare condition that affects most commonly large portions of the trunk or an extremity. Most cases occur during the first 2 years of life, but they also have been reported in adolescents and adults [31, 49]. Lipomatosis may also be associated with osseous hypertrophy and macrodactyly, but unlike neural fibrolipoma/macrodystrophia lipomatosa, nerves are not involved, and the condition is not confined to the extremities.
The radiological findings in lipomatosis include the presence of fatty tissue diffusely distributed within and between the involved muscles (Fig. 12.9). “Infiltrating congenital lipomatosis of the face” is a related entity present at birth or in infancy, consisting of an unencapsulated, infiltrating fatty mass characteristically involving the face [19, 67]. MR images depict an infiltrating fatty mass, and distortion of the facial bones and displacement of the airway by the lesion have been reported.


Fig. 12.9
(a, b) Diffuse lipomatosis of the thighs and legs in a 66-year-old woman. (a) Coronal SE T1-weighted MR image of the thighs. (b) Coronal SE T1-weighted MR image of the legs. Fat is diffusely distributed within and between the muscles of both thighs (a) and legs (b) and the subcutaneous fat. Although there is an asymmetry of the size of the limbs, the MR appearances are similar in both sides
12.2.2.1 Multiple Symmetrical Lipomatosis
This rare condition, predominantly affecting middle-aged men, is also known as Madelung disease or Launois-Bensaude syndrome. A familial occurrence has been described. The exact cause is unknown, although a hyperplastic mechanism has been considered [21, 55]. Symmetrical lipomatosis is usually associated with excessive alcohol intake, liver disease, diabetes, hyperlipidemia, hyperuricemia, malignant tumors of the upper airway, and neuropathy. Occurrence is usually sporadic, but some investigators believe an underlying hereditary factor may be present in the form of a mitochondrial dysfunction that disturbs the lipid metabolism.
Patients with symmetrical lipomatosis present with massive symmetrical deposition of mature fat in the neck, but also the cheeks, breast, upper arm, axilla, chest, abdominal wall, and groin may be involved [31, 49]. The fatty accumulation progresses frequently over many years and is painless. These fatty masses are unencapsulated, so they are poorly circumscribed with involvement of the subcutaneous fat and deep tissues, mostly posterior relative to the trapezius and sternocleidomastoid muscles, in the supraclavicular fossa, or between the paraspinal muscles. However, deep fat accumulation may be independent of involvement of adjacent subcutaneous fat, which can be atrophic. This suggests a local formation of fatty masses, rather than penetration of adipocytic tissue by subcutaneous fat. This preferential involvement of compartments distinguishes this disease from obesity. When symmetrical lipomatosis involves the deep soft tissues of the neck and mediastinum, it may cause dysphagia, hoarseness, severe respiratory insufficiency by extrinsic compression of the trachea, and signs of vascular compression (superior vena cava syndrome) [22, 31, 49, 56].
On CT and MR images, symmetric accumulation of fatty, unencapsulated, deep, or superficial masses have been reported (Figs. 12.10 and 12.11), with calcifications rarely being observed [22, 56]. Surgical debulking is the treatment of choice, but recurrence is common.



Fig. 12.10
(a, b) Madelung disease in a 53-year-old man with a history of alcohol abuse. (a) Axial SE T1-weighted MR image of the neck. (b) Axial FS SE T1-weighted MR image of the neck. Symmetric fatty deposits under trapezius and sternocleidomastoid muscles and anteriorly in the neck

Fig. 12.11
(a, b) Madelung disease. (a) Sagittal SE T1-weighted MR image. (b) Axial SE T1-weighted MR image of the neck. Diffuse fatty deposition (*) throughout the subcutaneous tissues in the neck
12.2.2.2 Adiposis Dolorosa (Dercum Disease)
This condition must be differentiated from symmetrical lipomatosis. It consists of diffuse or nodular painful, multiple subcutaneous fatty deposits (Fig.12.12). Adiposis dolorosa predominates in postmenopausal women and affects predominantly the regions of the pelvic girdle and the thigh. The patients complain of marked asthenia, depression, and psychogenic disturbances. The inheritance is autosomal dominant with variable penetrance [27].


Fig. 12.12
Adiposis dolorosa in a 34-year-old man with bilateral diffuse lipomata. Extended field-of-view longitudinal ultrasound of the right thigh shows multiple lipomas (arrows) throughout the subcutaneous tissues
12.2.2.3 Shoulder Girdle Lipomatosis
This syndrome was first described by Enzi et al., involving the scapulohumeral girdle, with fatty infiltration of muscles in six female adult patients [22]. This is a subtype of lipomatosis with different clinical, pathological, and radiological findings. It presents unilateral gradual enlargement and deformity of the shoulder and proximal part of the arm, with shoulder girdle muscle weakness, and motor and sensory neuropathy in the involved limb [22, 59]. Enzi et al. have also noted respiratory symptoms due to compression of the upper airway or infiltration of the laryngeal wall by fatty tissue [22]. MR imaging demonstrates diffuse accumulation of fat, within or between the involved muscles, with high SI identical to normal subcutaneous fat, on T1- and T2-weighted images, without cellular or edematous areas [59].
Bannayan-Zonana syndrome is a rare hamartomatous disorder, which affects men in 68 % of cases. Inheritance is autosomal dominant with variable expression. This syndrome is characterized by the presence of moderate macrocephaly, multiple hemangiomas, and subcutaneous and visceral lipomas (in up to 76 % of cases) [27].
12.2.3 Lipomatosis of Nerve
Lipomatosis of nerve has also been designated in the past as fibrolipomatous hamartoma, fibrofatty overgrowth, lipomatous hamartoma, lipofibroma, neurolipoma, intraneural lipoma, fatty infiltration of the nerve, and neural fibrolipoma. In 2013 the WHO continued with the designation of lipomatosis of nerve [26, 61]. The common term “neural fibrolipoma” is, however, still frequently used because it reflects the nature of this entity. It is a very rare tumor, characterized by a proliferation of fatty and fibrous components that surrounds the thickened nerve bundles and infiltrates both the epineurium and the perineurium. No vascular abnormalities are associated with the lesion [31, 49]. The cause is unknown, but some consider this condition as a congenital lesion, since it is occasionally present at birth, whereas others believe a relationship exists with a history of prior trauma. This tumor affects predominantly children or young adults, although a late presentation at the age of 75 years has been reported recently [23, 55]. According to Enzinger et al., males are affected more frequently than females, although a similar incidence has also been noted [31, 44, 49].
Lipomatosis of nerve occurs chiefly in the volar aspects of the hands, wrist, and forearm and usually involves the median nerve, although occasional involvement of other nerves such as the cubital, radial, ulnar, tibial, superficial peroneal, and sciatic has also been reported [17, 55, 66]. This entity is less common in the lower extremities. A soft tissue mass is frequently present several years before onset of symptoms. Lipomatosis of nerve usually gives rise to pain, paresthesia, or decreased sensation or muscle strength, in the area innervated by the affected nerves. According to some authors, in 27–66 % of patients with lipomatosis of nerve, there is associated bone overgrowth and macrodactyly of either the fingers or the toes, a condition described as macrodystrophia lipomatosa [31, 49]. Macrodactyly has also been noted in association with neurofibromatosis and vascular lesions or as idiopathic conditions. On plain radiographs, lipomatosis of nerve may manifest by a soft tissue mass or will only be suspected by indirect signs such as the presence of macrodactyly, usually affecting the second and third digits of the hand or foot [12, 48, 78]. There is a soft tissue and osseous hypertrophy, including long, broad, and splayed phalanges (Fig. 12.13). Calcifications on plain radiographs due to metaplastic bone formation have been noted [55].


Fig. 12.13
Macrodystrophia lipomatosa. Posteroanterior radiograph. Osseous and soft tissue enlargement, affecting the second digit
CT and MRI can be used to identify the neural origin of the tumor due to the presence of tortuous tubular structures, corresponding to enlarged nerve bundles within a predominantly fatty mass (Fig. 12.14). These structures, clearly depicted on MR images, show low SI on both T1- and T2-weighted images according to their fibrous content [12, 17, 23, 55, 66]. The tumor has the tendency to spread along the branches of the nerve, with a significant variation in the distribution of fat along the nerves and their innervated muscle [17]. The lesion consists of serpiginous low-intensity nerve fibers interspersed by fatty tissue [55]. The contrast between the low-signal nerve fascicles and surrounding high-signal fat results in a “cable-like” appearance of the tumor when visualized on axial planes on T1-weighted MR images and a “spaghettilike” appearance on coronal planes [23, 55]. The MR imaging findings of lipomatosis of nerve are very characteristic allowing a confident diagnosis and obviating the need for biopsy [55]. Lipomatosis of nerve must be differentiated from a nerve sheath lipoma. MRI allows differentiation between these two entities, since lipoma manifests as a focal mass separated from the nerve bundles. Resection of involved neural elements causes considerable sensory and motor deficits, but the symptoms can be relieved by carpal tunnel release [12].


Fig. 12.14
(a, b) Lipomatosis of nerve of the median nerve at the level of the carpal tunnel in a 40-year-old man. (a) Axial SE T1-weighted MR image. (b) Axial gradient echo T2*-weighted MR image. These MR images show a heterogeneous mass within the carpal tunnel. There is a mixed SI of fatty components, fibrous components, and neural fascicles (a, b). The signal intensity and localization are highly characteristic of a neurofibrolipoma of the median nerve
12.2.4 Lipoblastoma
Lipoblastoma is a well-encapsulated lesion, confined to the subcutis, and is composed of lobules of fat with septations, lipocytes, and lipoblasts (immature fat cells) and poorly differentiated mesenchymal cells in a myxoid stroma with lipoblasts in different stages of development [31, 49]. Cytogenetic analysis has shown it be associated with excess or structural rearrangements of chromosome 8 within the tumor cells [63]. If it infiltrates the subcutis and adjacent muscles and extends across anatomical planes, it was previously referred to as lipoblastomatosis, but now diffuse lipoblastoma is the preferred term. Lipoblastoma is approximately twice as common as diffuse lipoblastoma, which is generally more deeply located [31, 49].
Eighty-eight percent of lipoblastomas occur in patients below 3 years of age, 55 % of the cases in patients below 1 year of age, and in some instances they are present at birth. The occurrence of lipoblastoma in patients older than 8 years of age is rare, although it has been documented in some patients of 10–18 years of age and affects boys more often than girls [15, 31]. This entity most commonly occurs in the extremities, but lipoblastoma may be apparent in other locations such as the trunk, head, neck, axilla, prevertebral soft tissues, mediastinum, or retroperitoneum [35, 44].
In a review of 25 cases, Collins et al. have reported 11 lipoblastomas and 14 cases of diffuse lipoblastoma, with 19 cases (79 %) occurring in boys; 84 % of the patients were less than 5 years old. These lesions measured 1–21 cm in greatest dimension, but 60 % measured less than 5 cm [15]. The relative number of lipoblastoma and diffuse lipoblastoma in a series of 114 cases of the Armed Forces Institute of Pathology (AFIP), was 88 well-circumscribed lesions (lipoblastomas) compared with 26 diffuse forms (diffuse lipoblastoma) [49].
Lipoblastoma usually is a painless, soft tissue mass. The symptoms, although rare, are determined by the size and the location of the tumor. Surgical excision is the treatment of choice and is usually curative in lipoblastoma. Recurrence is rare and affects patients with the diffuse rather than the circumscribed type [15, 31]. Besides recurrence, lipoblastoma may have the capacity to differentiate into mature lesions, such as a lipoma or even fibrolipoma [15, 35, 70].
On ultrasound, lipoblastoma manifests as a mass of mixed echogenicity, with highly echogenic regions interspersed with areas of diminished echogenicity.
The appearance on CT scans varies according to the amount of the adipose and other soft tissue components. Lipoblastoma usually is seen as a fatty mass with scattered foci of soft tissue density.
On MR images lipoblastoma is mostly bright on T1- and T2-weighted images, but it may be hypointense to subcutaneous fat on T1-weighted images, without the signal characteristics of a fatty tumor [35, 70]. Some hyperintense areas on T2-weighted MR images have been described, consistent with cystic or myxoid areas (Figs. 12.15, 12.16, and 12.17). Lipoblastoma does not enhance or shows poor enhancement after intravenous gadolinium administration.




Fig. 12.15
(a, b) Lipoblastoma of the buttocks in a 5-year-old boy. (a) Axial SE T1-weighted MR image. (b) Axial TSE T2-weighted MR image. The lesion is located in the medial part of the gluteus maximus muscle protruding into the left ischiorectal fossa. On T1-WI the mass is heterogeneous and ill-defined with interspersed areas of high SI (a). On T2-WI the lesion is well defined and of overall high SI (b). The presence of fatty components is indicative for the lipomatous nature of the tumor. Although MR images do not allow differentiation from liposarcoma, the age of the patient is much in favor of a lipoblastoma

Fig. 12.16
(a, b) Lipoblastoma of the thigh in a 30-year-old woman. (a) Sagittal SE T1-weighted MR image. (b) Axial SE T2-weighted MR image. Dumbbell-shaped lesion located between the distal femoral diaphysis and the vastus intermedius muscle. The lesion is isointense to muscle on T1-weighted images (a) and has a very high SI on T2-weighted images (b). The presence of abundant immature fat cells is probably responsible for the lower SI of the lesion on T1-weighted images. As a consequence such lesions are hard to differentiate from myxoid tumors

Fig. 12.17
(a–d) Lipoblastoma of the buttocks in a 5-year-old boy. (a) Axial SE T1-weighted MR image. (b) Coronal FS TSE T2-weighted MR image. (c) Axial FS SE T1-weighted MR image. (d) Axial FS SE T1-weighted MR image after gadolinium contrast administration. The lesion is located within the left buttocks. On T1-WI the mass is heterogeneous, isointense to subcutaneous tissue, and ill-defined with interspersed strands of low SI (a). These strands are slightly hyperintense on FS T2-WI (b), and only a faint contrast enhancement is seen in these nonadipocytic areas (d). The presence of fatty components is indicative for the lipomatous nature of the tumor. The age of the patient is an important clue in favor of a lipoblastoma
The demonstration of a fatty mass on CT or MRI examination in an infant or child should raise the possibility of a lipoblastoma or diffuse lipoblastoma. Lipoma, lipoma variants, and liposarcoma are uncommon in infants and children. Radiologically and even on microscopic examination, lipoblastoma may be misdiagnosed as liposarcoma, especially myxoid liposarcoma. However, in the case of lipoblastoma, the clinical setting is quite distinct, since lipoblastoma occurs in children, while liposarcoma is very uncommon in this age group. Miller et al., in a review of 149 adipocytic tumors at a children’s hospital, have reported 7 lipoblastomas and 2 liposarcomas [60]. The liposarcoma patients were aged 9 and 14 years, and the children with lipoblastoma were younger, but 29 % were more than 3 years of age. In a review of more than 2,500 cases of liposarcoma at the AFIP, only two cases of liposarcoma occurred in children below 10 years old [49].
12.2.5 Angiolipoma
This tumor is composed of mature fat cells and a network of small vessels, containing typical fibrin thrombi. These features allow differentiation from lipoma and from intramuscular hemangioma with prominent fatty elements [31]. It occurs in young adults, being rare in children and in patients older than 50 years.
Angiolipomas have been divided into noninfiltrating and infiltrating types [20]. The most common type is the noninfiltrating type, which presents as a small (median size, 2 cm), encapsulated, subcutaneous nodule located in the trunk, upper arm, and particularly the forearm, rarely affecting the face, hands, or feet [31, 47]. Multiplicity of these lesions is frequent. The infiltrating angiolipoma is a rare, locally aggressive, and unencapsulated variant containing foci of angiomatous proliferation [47]. Imaging is only required in the infiltrating variant of this tumor. On plain radiographs this tumor may show as a mass of fat density, with serpiginous densities and punctate calcifications. On CT scans it usually shows as a poorly delineated heterogeneous intramuscular lesion, with attenuation values ranging from those of fat to those of muscle. This variant has a hypervascular pattern on angiography that can be incorrectly diagnosed as a soft tissue sarcoma.
On ultrasound the appearance will depend on the degree of vascular proliferation and calcification. If minor appearances are usually homogenous and similar to simple lipoma but if vascular tissues predominates multiple hypoechoic areas, calcification and increased Doppler signal can be present [7]. On MR images, angiolipoma shows a mixed composition of both fatty and vascular elements. Signal intensities depend on the relative proportion of tumor components. The nonfatty areas exhibit low SI on T1-weighted images and high SI on T2-weighted images and enhance markedly after intravenous injection of gadolinium contrast (Figs. 12.18 and 12.19). The excision of this tumor is rarely radical, due to its poorly circumscribed margins and muscle invasion, and local recurrence is common.



Fig. 12.18
(a–c) Angiolipoma of the left hemiscrotum. (a) Ultrasound. (b) Axial SE T1-weighted MR image. (c) Axial fat-suppressed SE T2-weighted MR image. The mass (arrows) shows predominant fat signal on ultrasound (*) and MR images. Within the lesion there are multiple vessels (arrowheads), hypoechoic on ultrasound, low SI on T1-weighted images, and increased SI on T2-weighted images (a–c)

Fig. 12.19
(a–d) Angiolipoma of the left triceps. (a) Axial SE T1-weighted MR image. (b) Axial fat-suppressed SE T2-weighted MR image. (c) Axial fat-suppressed SE T1-weighted MR image post gadolinium. (d) Ultrasound. The mass (arrow) within the lateral head of triceps shows some fat signal on MR images with linear areas of low SI on T1-weighted images which have increased SI on T2-weighted and T1-weighted post gadolinium images (a–c). On ultrasound the lesion is hyperechoic with multiple vessels with increased Doppler signal (d). MRI does not allow differentiation between intramuscular angioma and angiolipoma. Tiny fatty components can be found in both lesions
12.2.6 Myolipoma of Soft Tissue
Myolipoma of soft tissue is a rare benign tumor exhibiting features of mature smooth muscle and mature adipose tissue [26]. It is also known as “extrauterine lipoleiomyoma.” The lesion is most frequently located in the abdominal cavity, retroperitoneum, and inguinal areas and more rarely in the subcutis of the trunk and extremities [61]. The majority of the lesions (especially the deeply located abdominal lesions) are large at initial presentation, ranging from 17 to 25 cm in diameter [61].
Due to the presence of nonadipocytic elements within the tumor, imaging does not allow distinction from a well-differentiated liposarcoma. Coarse calcification may be seen in large lesions. On immunohistochemical analysis, smooth muscle components are strongly positive for smooth muscle actin and desmin. Treatment consists of surgical resection. No recurrence or malignant transformation has been described.
12.2.7 Chondroid Lipoma
This is a rare adipocytic tumor, with a variable background of mature fat with cells resembling lipoblasts and brown fat cells, showing features of both lipoma and hibernoma. It contains myxoid and chondroid material and pathologically mimics myxoid liposarcoma and myxoid chondrosarcoma [31, 34]. Meis et al. have reported 20 patients, with an average age of 36 years (range 14–70 years old), with tumors measuring 1.5–11 cm in size (median, 4 cm). Cytogenetic analysis has shown it be associated with translocation between the 11 and 16 chromosomes [63].
Chondroid lipoma manifests as a well-circumscribed mass in the subcutis, superficial fascia, or muscles of the extremities and occasionally in the trunk and head and neck [11, 61] and is mostly found in women. The lesion appears as a well-defined mass with prominent fluidlike areas at sonography and CT. Areas of bright echogenicity have been described also [34]. Calcification is usually present on CT scans and radiographs [34, 61]. The presence and nature of the calcifications – which can be irregular and curvilinear – can raise the possibility of either a malignant diagnosis (including synovial sarcoma, malignant peripheral nerve sheath tumor, epithelioid hemangioendothelioma) or a benign diagnosis (e.g., myositis ossificans) [34]. On MR images, a predominant low SI is seen on T1-weighted images, with only a few strands of high SI identical to fat, either in the periphery or the center of the lesion [61]. These lacy strands of high SI on T1-weighted images are suppressed on STIR images. On T2-weighted MR images, the mass is inhomogeneous and hyperintense, reflecting the largely myxoid consistency of the tumor (Fig. 12.20.). Other features of the mass, such as fine septations and a lobulated margin, suggest cartilage matrix [53]. However, chondroid lipoma demonstrates a whole spectrum of cellular and matrix content, which is reflected in variable MR imaging characteristics [11]. Based on the MRI characteristics, chondroid lipoma is difficult to distinguish from myxoid liposarcoma, extraskeletal myxoid chondrosarcoma, and ancient schwannoma [11]. Because MR imaging cannot differentiate absolutely between malignant and benign lesions, biopsy is required to make a final diagnosis [34].


Fig. 12.20
(a–d) Chondroid lipoma within the plantar aspect of the right foot. (a) Plain radiograph. (b) CT scan. (c) Sagittal SE T1-weighted MR image. (d) Sagittal FS SE T1-weighted MR image after gadolinium contrast administration. The lesion lies separate to the metatarsals with chondroid calcification (arrow) and a more proximal fatty component (*). After gadolinium administration, there is a heterogeneous enhancement (d) of the chondroid component
12.2.8 Spindle Cell Lipoma and Pleomorphic Lipoma
In these two clinically and pathologically related variants, the mature fat is replaced by collagen-forming spindle cells. Pleomorphic lipoma is considered as a pleomorphic variant of spindle cell lipoma, and it is distinguished by the presence of a marked cellular pleomorphism and scattered bizarre giant cells. Histologically the differential diagnosis from liposarcoma may be difficult [31]. Cytogenetic analysis has shown it be associated with cells showing abnormalities of chromosome 13 including deletions and monosomy, while immunohistochemistry staining is strongly positive for CD34 [63]. Spindle cell and pleomorphic lipomas typically present as a well-circumscribed nodule, confined to the subcutis of the neck or shoulder region in male patients older than 45 years. These lipomas usually manifest as a slow-growing, painless, solitary mass, with an average size between 3 and 5 cm. Although rare, multiple spindle cell lipomas have been described [25]. Fanburg-Smith et al. have reported 7 familial and 11 nonfamilial cases of multiple spindle cell lipomas, all occurring in male patients, and most of them in the sixth to eighth decades of life [25]. These patients had between 2 and more than 220 lesions, on the posterior neck or back and also involving the shoulders.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree