
Adrenal Vein Sampling
 Anatomy
Anatomy
The adrenal gland’s arterial supply and venous drainage are depicted in Figure 48–1. Three arteries supply each gland: the superior adrenal artery, which arises from the inferior phrenic artery; the middle adrenal artery, which arises from the aorta between the level of the celiac and renal arteries; and the inferior adrenal, which arises from the renal artery. The arteries end in perforating branches, which pass perpendicularly through the capsule to the cortex. There is no direct arterial supply to the medulla.
The venous drainage of the adrenal gland consists of a series of sinusoids and fine venules, which arise in the cortex, parallel to the perforating arteries. These drain centrally through the medulla to join a valveless muscular central vein at right angles. At the corticomedullary junction, there is a rich plexus of sinusoids that drains independently into the central vein. There is no direct venous drainage from the medulla. The junction of the perforating venules and the central vein is lacking in medial musculature,1 and is therefore predisposed to rupture during adrenal venography.2 The adrenal capsular plexus is drained by many venae comitantes, which run adjacent to the small capsular branches of the adrenal arteries. These venae comitantes merge to form adrenal capsular veins, which often communicate with the renal capsular veins, lumbar veins, phrenic veins, and others. The central vein often communicates directly with the capsular veins through perforators at the apex of the gland.
In the left adrenal gland, a solitary central vein passes down the entire length of the gland. It generally joins the inferior phrenic vein, which courses medial to the adrenal gland to form a short phrenicoadrenal trunk, which then joins the left renal vein directly opposite the left gonadal vein. As opposed to the central adrenal vein, the left inferior phrenic vein usually contains a competent valve (Fig. 48–2, arrow); therefore, it is not usually visualized at adrenal venography. The junction of the left adrenal vein with the left renal vein occurs just lateral to the aorta, fluoroscopically at a point approximately 1 cm lateral to the left lateral edge of the vertebral column.
In the right adrenal gland, generally three central venous tributaries—superior, inferior, and posterior—join to form a short central vein. The central vein courses in a cephalad direction to join the inferior vena cava along its posterior right aspect, at the level of T12. In about 10% of cases, the central vein will join the posterior aspect of a hepatic vein near the inferior vena cava; rarely, the right adrenal vein may drain directly into the right renal vein. Other exceptions to standard anatomy have been described, including multiple adrenal veins, connection of the right adrenal vein with the portal system, and the left adrenal vein emptying into the lumbar veins.3–5
 Technique
Technique
To catheterize the adrenal veins, and to perform adrenal vein sampling, a 5 to 7F Cobra-shaped catheter is used.6,7 Occasionally, catheters shaped similar to those in Figure 48–3 may be necessary. One to two tiny sideholes are punched in the distal portion of the catheters, within 1 to 2 mm of the tip, to facilitate aspiration of blood. No premedication is given to avoid iatrogenic suppression of adrenal hormone output. The tip of the catheter is directed into the orifice of each adrenal vein. The patient is treated with heparin, 5000 U intravenously, to avoid venous thrombosis. Three samples (8 to 10 mL) are taken at 5- to 10-minute intervals to compensate for episodic variations in hormone secretion.8 To calculate gradients, simultaneous samples are taken from a peripheral or iliac vein. Blood samples should be drawn before injection of contrast if at all possible.
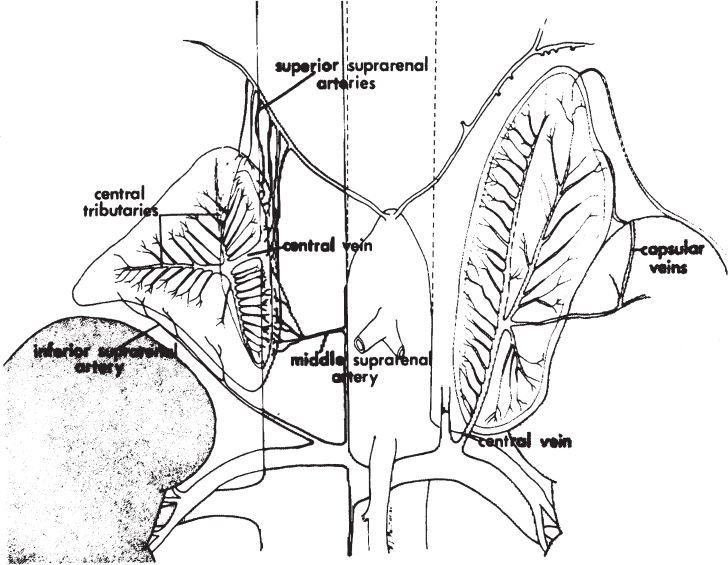
FIGURE 48–1. Representation of the arterial and venous anatomy of the adrenal gland. There is but one central vein on each side; the right arises from the posterolateral aspect of the inferior vena cava, the left from the superior aspect of the left renal vein. (Reproduced with permission from ref. 9.)
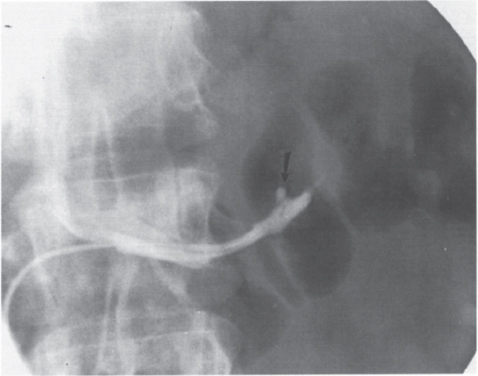
FIGURE 48–2. Normal left phrenicoadrenal trunk. Note the competent valve (arrow) in the terminal part of the left inferior phrenic vein.
Despite appropriate catheterization of the adrenal veins, it may be difficult to aspirate adequate amounts of blood for venous sampling. The problem is usually caused by obstruction of the catheter endholes by the venous walls and is encountered more commonly with the right adrenal vein. Changes in respiration, Valsalva maneuvers, or gravity drainage may assist in sample collection.
If necessary, confirmation of catheter tip position may be performed by gently injecting a small amount of contrast (less than 0.5 mL). Retrograde injection of contrast into the small perpendicular branches of the adrenal vein induces change in the secretory activity of the gland, but diis change is dependent on the amount of contrast being injected. Traditional adrenal venography (3 to 6 mL of contrast) may cause extremely high elevations of adrenal vein cortisol levels,7
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



