Overview
Location
• The heart is found within the thoracic cavity in a space called the middle mediastinum.
• Posterior to the ribs and lungs, it is located between the third to fifth intercostal spaces.
• The upper portion, or base of the heart, lies closer to the sternum than the lower portion, or apex, which lies inferior and to the left of midline.
• The apex is slightly more anterior than the base.
Anatomy
• The heart is a muscle consisting of 3 layers:
1. Epicardium (smooth, thin outer layer).
2. Myocardium (thicker, muscular layer).
3. Endocardium (smooth, thin inner surface).
• The heart sits within a sac called the pericardium and is surrounded by a small amount of serous fluid to prevent friction as the heart beats.
• The heart has 4 chambers:
• Two upper chambers, the right and left atria.
• Two lower chambers, the right and left ventricles.
• The upper portion of both atria have a small triangular extension called an appendage (also called auricle) that is tightly lined with muscle called pectinate muscle.
• The lining of the right atrium (RA) is mostly smooth with some pectinate muscle on the free wall. It receives unoxygenated blood from 3 major sources:
1. Superior vena cava (SVC): enters the chamber from above.
2. Inferior vena cava (IVC): enters from below.
3. Coronary sinus: found between the IVC and the opening to the right ventricle (RV).
• The IVC and coronary sinus have prominent edges that represent remnants of valves that once covered them during fetal days. These are the eustachian valve and the thebesian valve respectively.
• The midposterior RA wall is also the interatrial septum. It has a thinner area in the midportion representing the fossa ovalis.
• The left atrium (LA) is also smooth walled and receives oxygenated blood from four pulmonary veins. This is the most posterior chamber.
• The right ventricle (RV) is the most anterior chamber whose inner surface is lined with bands of muscle called trabeculae carneae. There is a dense band of tissue in the distal part of the chamber that runs perpendicular to the interventricular septum called the moderator band.
• The interventricular septum (IVS) separates the RV from the LV and consists of mostly muscular tissue with the exception of a small portion of membranous tissue near the insertion of the valves.
• The left ventricle (LV) is more trabeculated than the RV and the walls are also much thicker. The LV makes up the apex of the heart.
• The heart also has 4 valves that control blood flow in and out of the chambers:
• 2 atrioventricular (A-V) valves that control the blood flow from the atria to the ventricles
• 2 semilunar valves that control blood flow from the ventricles to the great vessels.
• The mitral and tricuspid valves are the A-V valves. Their leaflets attach to a ring of dense tissue between the chambers called the annulus fibrosus. From the free edges of the leaflets are multiple strong, thin fibers called chordae tendineae. These chordae attach to cone-shaped projections of muscle from the ventricular walls called papillary muscles.
• The mitral valve is located between the LA and LV and has 2 leaflets: the anterior leaflet and the posterior leaflet. Also known as the bicuspid valve, its cords attach to the anterolateral and posteromedial papillary muscles.
• The tricuspid valve is found between the RA and RV and has 3 leaflets: the anterior, posterior, and septal. There are 3 papillary muscles in the RV where the tricuspid cords attach: the anterior, posterior, and septal papillary muscles.
• The semilunar valves are the aortic and pulmonic valves. They are crescent shaped and have no cords or papillary muscles associated with them.
• The aortic valve is found in the left heart between the LV and the aortic root and has 3 cusps:
1. Right coronary
2. Left coronary
3. Noncoronary
• The pulmonic valve is located between the RV and the main pulmonary artery. It has 3 cusps:
1. Anterior
2. Right
3. Left
• The main pulmonary artery and the aorta comprise the great vessels. These are found at the base or superior aspect of the heart. A short ligament, the ligamentum arteriosum, connects the two.
• The aorta arises from the ventricle and is divided into three regions: the ascending, arch, and descending aorta. There are 3 vessels that originate from the arch: the brachiocephalic (also called innominate), left common carotid, and left subclavian arteries. The brachiocephalic branch is directed rightward and bifurcates into the right common carotid and right subclavian arteries.
• The main pulmonary artery (PA) begins at the infundibular region of the RV and moves anteriorly before it bifurcates into the right and left pulmonary arteries. The right PA is directed toward the right lung and moves posterior to the aortic arch. The left PA branches in the direction of the left lung.
• Just beyond the aortic valve are 3 small, crescent-shaped pouches called the sinus of Valsalva. Each is associated with one of the aortic cusps. The right coronary artery originates from the right cusp sinus and the left coronary artery from the left cusp sinus. The remaining sinus has no coronary artery associated with it, hence the name noncoronary cusp.
• The left main coronary artery bifurcates shortly after its origin into the left anterior descending (LAD) and the left circumflex artery. These are found embedded in fat on the exterior surface of the heart. The fat is there to protect the vessels. The LAD runs inferiorly down the anterior interventricular sulcus which is a groove separating the RV from the LV. The left circumflex is located posterolateral to the LAD and runs partly in the atrioventricular groove (also called coronary sulcus), which is the separation between the RA and RV on the external surface of the heart.
• The right coronary artery (RCA) eventually bifurcates but not so quickly as the left, and is also embedded in fat wrapping around the heart in the right atrioventricular groove. The branches of the RCA are the right posterior descending and the marginal artery. The posterior descending artery is found in the posterior interventricular sulcus.
• The cardiac veins drain into the coronary sinus, which is found in the left atrioventricular groove (coronary sulcus) on the posterior surface of the heart between the LA and LV.
Physiology
• The heart is the center of the circulatory system responsible for directing the flow of deoxygenated blood to the lungs and then distributing the reoxygenated blood to the rest of the body.
• The heart has its own intrinsic conduction system consisting of specialized tissue called nodes. The nodes create the impulse that regulates the heart’s rate of contraction. The sinoatrial (SA) node, found in the upper portion of the RA near the SVC, is considered the initial pacemaker of the heart. When it fires, an impulse is sent by way of internodal pathways across the atria, causing them to depolarize and contract. The atrioventricular (AV) node, found in the lower portion of the right interatrial septum, is then stimulated and directs the pulse toward the ventricles by way of the Bundle of His, which then bifurcates into the right and left bundle branches. These extend towards the apex of the heart by way of the interventricular septum. Multiple small bands called Purkinje fibers branch off the main bundle branches, across the ventricles, and into the muscle cells, spreading the impulse through the ventricles and causing them to depolarize and contract simultaneously.
• The conduction system emits an electrical impulse that can be detected on the surface of the body, which is how we get an electrocardiogram (ECG). The ECG consists of 3 distinct phases:
1. The P wave is a small bump corresponding to atrial contraction and depolarization.
2. The QRS complex, which is a series of downward and upward deflections, relates to ventricular contraction and depolarization.
3. The T wave is a small bump representing ventricular repolarization. Atrial repolarization is not observed on the ECG because it occurs at the same time as the QRS complex.

• There are 2 parts to the cardiac cycle: systole (muscular contraction) and diastole (muscular relaxation).
Sonographic Appearance
• The pericardium is the most reflective structure and appears almost white.
• The papillary muscles and myocardium are medium gray and homogeneous in echo texture.
• The valves are slightly more echogenic than the walls when perpendicular to the ultrasound beam.
• The area within the chambers and great vessels, as well as any other fluid space, is anechoic.
Preparation
Patient Prep
• A basic ECG is attached to the patient to assist with the timing of the cardiac cycle. Leads are attached to the right chest, left chest, and left hip region—avoiding hair, if possible.
Patient Position
• Left lateral decubitus for most views with the left arm extended above the head and the right arm at the patient’s side.
• Subxiphoid: left lateral decubitus or supine. Bend the knees to relax the stomach muscles if needed.
• Suprasternal: the patient is supine with the neck extended. A pillow can also be placed under the shoulders allowing the head to drop back, hyperextending the neck even further.
Transducer
• 2.5 MHz.
• 3.5 MHz recommended for smaller, thinner patients.
• Use a 5.0-MHz transducer when structures in the near field need to be further evaluated (e.g., LV apex).
Breathing Techniques
• For the majority of patients, normal respiration.
• When ribs or lungs interfere, having the patient either hold his or her breath or expel all air and not breathe, may improve the image. You may also need to slide an interspace to follow the movement of the heart. Experiment to find the best possible picture.
Transducer Orientation
• Images are taken from 4 routine positions on the chest wall:
1. Parasternal
2. Apical
3. Subxiphoid (also called subcostal)
4. Suprasternal

Adult Heart Survey • 2D Examination
The purpose of the 2D examination is to:
• Identify the chambers and walls and valves of the heart, and evaluate their size, thickness, and motion.
• Assess the anatomical relationships of structures to rule out congenital defects.
• Document the presence of any pathology including tumors or fluid surrounding the heart, or thrombi within.
Parasternal Views
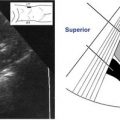
1. Begin with parasternal long axis by placing the transducer to the left side of the sternum in the second to third intercostal space with the indicator on the transducer directed towards 10 o’clock. Evaluate the sizes of the LA, LV, aortic root, and the RV. Assess for thickness and motion of the AV, MV, IVS, and posterior wall of the LV.

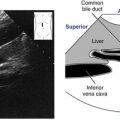
2. Maintaining the same interspace and 10 o’clock orientation, angle the transducer inferior and medial towards the umbilicus. This produces the right ventricular inflow view and visualizes the more anterior structure of the heart: the RA, TV, and RV. A remnant of the eustachian valve (a normal variant) may also be observed in the RA.

3. To obtain the right ventricular outflow view, the transducer is now angled superior and lateral towards the left shoulder. The indicator is still directed towards 10 o’clock. This will open the pulmonary artery and allow for assessment of the pulmonic valve.

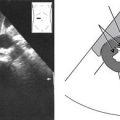
4. Rotate the transducer 90 degrees clockwise towards 1 o’clock, maintaining the same interspace as above and keeping the transducer close to the sternum. The parasternal short-axis views are observed here, beginning with the aortic valve level. Tilt the transducer towards the right shoulder. Start by visualizing the area above the aortic valve for the presence of pathology, then slowly sweep towards the level of the aortic valve. The AV should be in the center of the screen with the LA, RA, RV, and PA surrounding it. Evaluate for the presence of 3 aortic cusps and note the thickness and motion of all the valves.

5. Continue to slowly sweep laterally through the left ventricular outflow tract region towards the mitral valve. Only the angle of the transducer has changed and the ultrasound beam is now pointing almost directly anterior to posterior. Both leaflets of the mitral valve should be observed as well as its biphasic motion.

6. Slowly angle the transducer further lateral, towards the left hip. The cross section of the LV appears round with the papillary muscles indenting the inner surface, giving the cavity a mushroom like appearance. Assess LV function for focal or global abnormalities. Continue to sweep laterally, beyond the papillary muscles as deep into the ventricle as possible allowing for further assessment of LV function.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree