Fig. 7.1
Post-contrast axial CT scan at the level of the upper mediastinum depicts a circumferential granulomas within the wall of the trachea (white arrow) with stenosis of the lumen
Post-intubation injuries occur because of tracheal irritation from the endotracheal tube or for tracheostomy stoma. There are different predisposing factors, including too large a stoma, infection in the stoma and excessive pressure from the connecting systems. Granulation tissue can determine a narrowing of the tracheal lumen (Fig. 7.1).
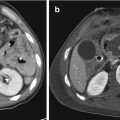
Acquired tracheo-oesophageal fistula (Fig. 7.2) could be the result of prolonged erosion by the endotracheal tube positioned postero-laterally, while the tracheo-innominate artery fistula may result from prolonged cuff erosion inferiorly and anteriorly to the trachea. Inappropriate low stoma may further increase the probability of a direct erosion of the trachea by the innominate artery.


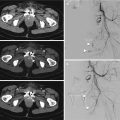
Fig. 7.2
Post-contrast axial CT scan at the level of the upper mediastinum depicts a defect of the posterior wall of the trachea continuing in the lumen of the oesophagus (white arrow head), due to a post-traumatic tracheo-oesophageal fistula
Also penetrating injury to the cervical or mediastinum trachea is often the cause of a tracheo-bronchial rupture. However, high speed traffic accidents are the most frequent cause of tracheal and bronchial injuries.
It is supposed that 50% of patients die at the trauma scene from severe respiratory insufficiency or other associated injuries, especially significant traumatic lesions of thoracic cage, lungs and thoracic aorta [7, 8]. In patients that survive, airway injuries have an overall mortality rate of 30% [9].
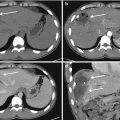
Generally, airway injuries are mainly located on the initial part of the respiratory tract. In 15–27% of cases, rupture is tracheal (Fig. 7.3) and 76% is exclusively bronchial, either on the right main-stem bronchus (47%) (Fig. 7.4) or on the left main-stem bronchus (32%) [10].



Fig. 7.3
Coronal CT reconstruction demonstrates a focal discontinuity of the right wall of the trachea (white arrow) associated with ipsilateral pneumothorax and subcutaneous emphysema

Fig. 7.4
Post-contrast axial CT scan depicts the disruption of the right main-stem bronchus with a visible posterior wall defect (white arrow). There is a bilateral pneumothorax associated with lung contusions and parenchymal haemorrhage of the right inferior lobe due to a diffuse laceration
Laceration of the cervical trachea is rare for the elasticity of the cartilagineus rings and the presence of many hard bones as the jaws, the sternum manubrium, the clavicles ant the cervical spine that protect this upper segment of the airways.
Bronchial injuries occur more commonly than tracheal, usually on the right side and between 2.5 cm from the carina [11] (Fig. 7.4), while 80% of tracheal lacerations occur generally 2 cm above the carena.
Most major airway injuries are not recognized initially. Diagnosis of tracheal rupture may be delayed as a result of its rare incidence, subtle and not specific clinical and radiological manifestation and the presence of additional clinical findings of other more common associated injuries of the thorax and other body districts [6, 12].
A significant number of cases are undiagnosed until complications develop either at the site of rupture, such as bronchial stenosis, or in the lung distal to the rupture such as lung infection and atelectasis (Fig. 7.5) [13, 14].


Fig. 7.5
Post-contrast axial CT scan shows a middle lobe atelectasis associated with an abscess (white arrow)
In fact, in two thirds of airway injuries, the diagnosis is delayed with subsequent high morbidity for serious complications, such as recurrent pneumonia, empyema (Fig. 7.6), pulmonary abscesses, mediastinitis (Fig. 7.7), sepsis, airway obstruction and atelectasis [10, 15].



Fig. 7.6
Post-contrast axial CT scan shows a left side empyema with air-fluid level (white arrow) correlated to pulmonary atelectasis (white arrow head). The right lung shows multiple, lobular, patchy, confluent consolidation areas, due to bronchopneumonia associated with pleuric fluid

Fig. 7.7
Post-contrast CT coronal reconstruction shows multiple neck and mediastinal fluid collections (white arrows) mixed to air bubbles due to a post-traumatic cervical-mediastinitis
Generally, the most frequent symptoms of all blunt airway injuries are dyspnoea (76–100%), hoarseness (46%), subcutaneous emphysema (35–85%) and haemoptysis (14–25%) [16].
In many cases, the diagnosis is missed in the acute phase and is detected only because of persistent lung or lobar atelectasis. Bronchoscopy should be performed in any cases in which the features described previously provide at least some suspicion of an airway lesion.
7.2 Clinical Features
Clinical findings of airway rupture are sometimes unclear and may be hidden by other traumatic injuries. Alternatively, some obvious airway rupture features may be wrongly assigned to lesions of other structures, especially oesophagus.
Pain associated with swallowing and skin contusion, neck emphysema, pneumo-mediastinum and hoarseness are clinical findings that can allow suspecting the diagnosis.
Other symptoms are dyspnoea, cough, bloody saliva, haemoptysis and dysphagia. These symptoms are frequently associated with physical features as cyanosis, pneumothorax, vocal cord paralysis, aphonia and subcutaneous emphysema diffused also into shoulders and chest fat planes (Fig. 7.8).


Fig. 7.8
Chest radiograph shows extensive subcutaneous emphysema diffused into shoulders and chest fat planes; it is also present pneumo-mediastinum, with multiple lucencies along mediastinal planes
The pneumothorax is frequently large and under tension (Fig. 7.9). The air leak may be persistent after introduction of pleural drainage. In these circumstances, the lung fails to expand. One unusual but characteristic feature that may be evidenced in cases of bronchial tear and a large pneumothorax is that bronchial rupture may allow the lung to bulge downwards from the hilum giving rise the “fallen lung” sign (Fig. 7.10). Normally, in the presence of a pneumothorax, the lung recoils towards the hilum, the vascular pedicle persists in its normal site and the lung remains perfused although under-ventilated.



Fig. 7.9
X-ray film performed immediately after the admission, evidences an extensive right pneumothorax with complete collapse of the ipsilateral lung

Fig. 7.10
Post-contrast axial CT scan demonstrates a left undertension pneumothorax. The ipsilateral lung bulges downwards from the hilum, giving the “fallen lung” sign (white arrow); it is also evidenced the presence of pneumopericardium (white arrow head)
If the “fallen lung sign” is present, the consequent ventilation-perfusion discrepancy may result in hypoxia and cyanosis.
It is also necessary to evaluate if tracheal injury is partial or complete.
Clinical signs of partial tracheal rupture include gradually increasing dyspnoea, haemoptysis, hoarseness and subcutaneous emphysema. In complete tracheal rupture, the skin of the anterior neck moves in and out with breathing movement and a gap in the tracheal rings can be felt beneath the moving skin.
Tracheo-bronchial injuries could also be suspected in the presence of subcutaneous cervical emphysema expanding with mechanical ventilation, pneumo-mediastinum and recurrent pneumothorax due to the persisting air leak (Fig. 7.11) [17].


Fig. 7.11
Post-contrast axial CT scan evidences a diffuse subcutaneous chest cage emphysema associated with a large pneumo-mediastinum (white arrow head) and left pneumothorax (white arrow) due to air leak
Sometimes, patients have other blunt lesions as laryngeal trauma, cervical spine or mandibular fractures, oesophageal injury, clavicular, scapular or ribs fractures. Oesophageal perforation is present in up to 20% of cases (Fig. 7.12).


Fig. 7.12
Post-contrast CT axial image at the level of inferior mediastinum shows a mediastinal fluid collection (white arrows) mixed to air bubbles, posteriorly to the oesophagus (white arrow heads), due to oesophageal injury and perforation
Clinical features of tracheal stenosis (Fig. 7.13), as a consequence of a tracheal injury, include dyspnoea on effort, stridor or wheezing and episodes of obstruction even with small amounts of mucus. Other complications could be the development of a tracheo-oesophageal fistula (Fig. 7.14) or a tracheo-innominate fistula.



Fig. 7.13
CT coronal reconstruction of the trachea shows a post-traumatic stenosis (white arrows)

Fig. 7.14
CT coronal reconstruction obtained after administration of oral contrast demonstrates the passage of the c.m. from the lumen of the oesophagus in the lumen of the main right bronchus (white arrows) due to a post-traumatic broncho-oesophageal fistula. The oral contrast is also spread in the lumen of bilateral bronchial tree (white arrow heads)
The most common clinical manifestation of a post-traumatic tracheo-oesophageal fistula is represented by considerable secretion associated with cough and recurrent broncho-pneumonia. Gastric lumen enlargement may also occur.
Tracheo-innominate fistula may be associated with severe haemoptysis.
7.3 CT Technique
CT is considered the more relevant diagnostic tool in patients with blunt chest trauma following the basic and indispensable chest X-ray film [18].
When a closed injury to the airways is suspected, it is important to perform immediate neck and chest CT scan, including three-dimensional image reconstruction of the trachea and the main bronchus.
Traditionally, the gold standard for the diagnosis is bronchoscopy because it enables visualization both the side and extent of the tracheo-bronchial injury. But in patients with severe respiratory insufficiency or in haemodinamically unstable patients, it may be impossible to perform. Bronchoscopy is not only time consuming, but also not always immediately available. Differently from bronchoscopy, CT is non-invasive, quicker and more ready available [5].
CT can clearly demonstrate fascial fat planes, arterial and venous vessels, larynx, trachea, bronchus and oesophagus traumatic lesions (Figs. 7.12 and 7.14), and it is the most important preoperative diagnostic imaging modality for determining the location, extent and type of airway lesions [6, 19].
7.4 MDCT Protocol Design Consideration
The MDCT protocol that is illustrated is designed for 64-row CT scanner; images are acquired at 0.625 collimation, with reconstruction axial slice of 2.5 mm, pitch of 0.984 and gantry rotation time of 0.5 s.
Preliminary unenhanced neck and chest CT is obtained to detect free air bubbles into the superficial and deep fascial fat planes or in fluid collections to depict blood clots inside haemothorax, haemopericardium and haemomediastinum.
Intravenous administration of contrast medium is mandatory for clearly evidencing neck and chest injuries.
Intravenous injection of a volume of 70–90 of iodine c.m. is generally sufficient for evaluating the enhancement of vessel lumen and surrounding other structures.
The contrast medium (c.m.) is injected with an 18–20 gauge needle through the ante-cubital vein by the use of a dual syringe power injector.
The c.m. transit time is determined by using a test-bolus in the ascending aorta lumen.
The optimal delay time corresponds to the peak arrival time of a test-bolus in the aortic lumen. The image acquisition is triggered at an attenuation threshold of 150 UH.
For better viewing, the enhancement alterations of the neck and chest tissues and vessels, contrast agents with higher concentration of iodine (400 mg/mL) and high injection rates (at least 3–4 mL/s) are preferred and are followed by a 30–50 mL saline chaser, also injected at a rate of 3–4 mL/s.
The c.m. arterial phase is mandatory to detect neck and chest arterial injuries.
The portal phase acquisition, obtained with a scan delay of 70 s, gives maximum airway wall, neck and mediastinum tissues and venous lumen enhancement.
In selected cases, orally administration of iodine contrast material could be helpful for demonstrating tracheo-oesophageal fistulization.
Sagittal and coronal MIP reformatted images are useful for localizing the ruptured segment of tracheo-bronchial tree and evaluating the map of the distribution of air bubbles, pneumothorax and blood collections. The post-processing procedure mainly requires a minimum-intensity projection technique for airway imaging. If tracheo-bronchial injury is suspected, three-dimensional (3D) extraction of the airway may be useful by focusing the 3D volume-rendering technique on the tracheo-bronchial tree. This technique is classically utilized for depicting stenosis or distortion of the tracheo-bronchial lumen, but may also allow the diagnosis of tracheo-bronchial injury by demonstrating a wall defect and/or an abnormal position of lobar and segmental bronchi [20].
7.5 Radiological Findings
As the clinical symptoms of acute airway injuries may not be specific and initially hidden by the presence of traumatic lesions of other organs and structures; the chest radiograph and CT scan are both important methods for diagnostic evaluation.
There are two main radiographic manifestations of tracheal and bronchial injuries: evidence of air leakage at the site of rupture and dysfunctional ventilation of the lung distal to the rupture. Evidence of air leakage is the more critical finding, and the absence of air leakage makes the diagnosis of a tear of the tracheo-bronchial tree very difficult (Fig. 7.15) [9].