Allergic Lung Diseases: Hypersensitivity Pneumonitis and Eosinophilic Lung Disease
W. Richard Webb
HYPERSENSITIVITY PNEUMONITIS
Hypersensitivity pneumonitis (HP), also known as extrinsic allergic alveolitis, is an allergic lung disease caused by the inhalation of antigens contained in a variety of organic dusts. Farmer’s lung, the best-known HP syndrome, results from the inhalation of fungal organisms (thermophilic actinomycetes) growing in moist hay. Many other HP syndromes have been reported, and the list continues to grow. As with farmer’s lung, HP syndromes are usually named after the setting in which exposure occurs or the organic substance involved. These include bird fancier’s lung (bird proteins), mushroom worker’s lung (thermophilic actinomycetes), malt worker’s lung (Aspergillus species), maple bark disease (Cryptostroma species), bagassosis (thermophilic actinomycetes in sugarcane fibers), building-associated HP, and hot-tub lung (mycobacteria). In about 50% of cases, the responsible antigen cannot be determined despite a careful history and environmental assessment.
Acute exposure of susceptible individuals to an offending antigen produces fever, chills, dry cough, and dyspnea; longterm exposure can produce progressive shortness of breath with few or minimal systemic symptoms. Recurrent acute episodes are common with recurrent exposure.
Although the mechanisms by which HP occurs are unclear, it is associated with circulating antibodies (IgG and IgM). These, however, are not specific to HP, as they are commonly present in exposed individuals who are asymptomatic. There is a reduced incidence of HP in tobacco smokers.
The prognosis of patients with HP is good if the patient is removed from the antigenic environment. If not, progressive fibrosis can lead to significant respiratory disability and death.
The clinical, radiographic, and pathologic abnormalities occurring in patients with HP are similar regardless of the organic antigen responsible. These abnormalities can be classified into acute, subacute, and chronic stages. Often manifestations of more than one stage coexist.
Acute Stage
Exposure to large amounts of antigen in susceptible individuals may result in acute lung injury with dyspnea (Table 16-1). The acute stage of HP is characterized by alveolar filling by a neutrophilic inflammatory exudate and pulmonary edema or hemorrhage due to diffuse alveolar damage.
Radiographs typically show ill-defined air-space consolidation, predominantly in the middle and lower lung zones, but they may be normal even in the face of marked symptoms. Ill-defined air-space nodules can also be seen with acute exposure. High-resolution CT (HRCT) in this stage may show bilateral air-space consolidation and small, illdefined, centrilobular nodules.
Subacute Stage
Continued exposure to the antigen leads to progressive symptoms over a period of weeks or months. This is termed the subacute stage of HP. This stage of HP is characterized by alveolitis; interstitial infiltrates; small, irregular, poorly defined granulomas; and cellular bronchiolitis. Histologic abnormalities are usually most severe in a peribronchiolar distribution.
Radiographic Findings
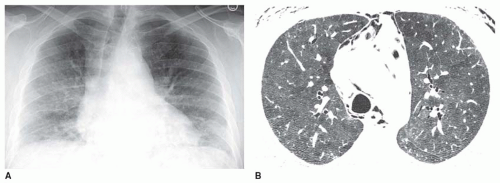
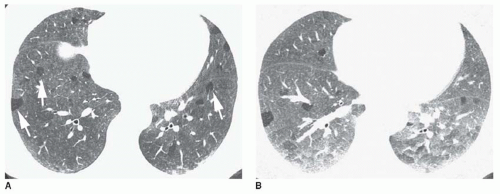
After resolution of the acute abnormalities, which may take several days, or between episodes of acute exposure, a poorly defined nodular pattern or an ill-defined increase in lung density with obscuration of vascular margins (i.e., groundglass opacity) may be visible on radiographs (Fig. 16-1). As in patients with acute disease, radiographs may be normal in the face of symptoms and an abnormal biopsy (Table 16-2).
HRCT Findings
HRCT is often first performed in the subacute stage of HP, weeks to months following first exposure to the antigen.
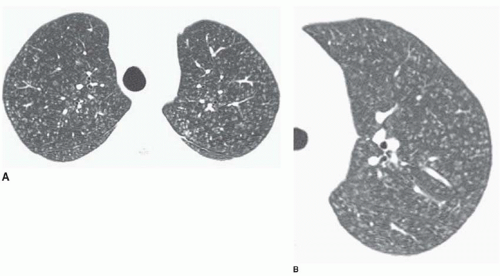
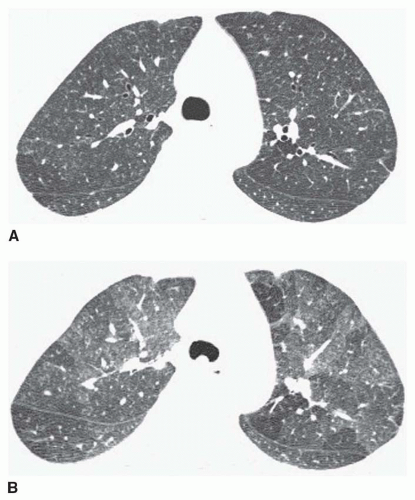
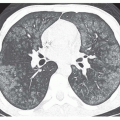
HRCT is more sensitive than chest radiographs in HP and may show typical features when chest films are normal. Typical HRCT findings include patchy ground-glass opacity (75% to 90%; see Figs. 16-1B, 16-2, and 16-3) and small illdefined centrilobular nodules of ground-glass opacity, usually 3 to 5 mm in diameter (40% to 60%; see Figs. 16-2 and 16-4,16-5 and 16-6). These findings reflect the typical histologic abnormalities of HP; patchy ground-glass opacity correlates with the presence of alveolitis, while centrilobular nodules correlate with ill-defined peribronchiolar granulomas. These abnormalities are often seen in conjunction and may be diffuse or most marked in the middle or lower lung zones. The presence of ground-glass opacity nodules or patchy groundglass opacity in a patient with known antigen exposure and typical symptoms is usually diagnostic in clinical practice.
HRCT is more sensitive than chest radiographs in HP and may show typical features when chest films are normal. Typical HRCT findings include patchy ground-glass opacity (75% to 90%; see Figs. 16-1B, 16-2, and 16-3) and small illdefined centrilobular nodules of ground-glass opacity, usually 3 to 5 mm in diameter (40% to 60%; see Figs. 16-2 and 16-4,16-5 and 16-6). These findings reflect the typical histologic abnormalities of HP; patchy ground-glass opacity correlates with the presence of alveolitis, while centrilobular nodules correlate with ill-defined peribronchiolar granulomas. These abnormalities are often seen in conjunction and may be diffuse or most marked in the middle or lower lung zones. The presence of ground-glass opacity nodules or patchy groundglass opacity in a patient with known antigen exposure and typical symptoms is usually diagnostic in clinical practice.
TABLE 16.1 Acute Hypersensitivity Pneumonitis | ||||
|---|---|---|---|---|
|
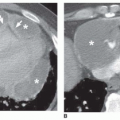
Another common manifestation of subacute HP is the presence of focal areas of decreased attenuation (mosaic perfusion) on inspiratory HRCT (75% to 85%; see Figs. 16-2B, 16-7, and 16-8) or air trapping on expiratory HRCT (90%; see Figs. 16-8 and 16-9). These areas usually have sharply defined margins and a configuration consistent with involvement of single or multiple adjacent pulmonary lobules. The areas of decreased attenuation and air trapping result from the bronchiolitis seen in patients with HP. In some patients with HP, evidence of expiratory air trapping is seen in the absence of inspiratory scan abnormalities.
TABLE 16.2 Subacute Hypersensitivity Pneumonitis | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||
A combination of increased lung attenuation (groundglass opacity) and decreased lung attenuation (mosaic perfusion) on inspiratory scans is termed the “headcheese sign” because it resembles a sausage of the same name (see Figs. 16-2B, 16-7, and 16-8). The headcheese sign is common in HP and is suggestive of the diagnosis.
In about 10% of patients with HP, thin-walled lung cysts are visible, ranging in size from a few millimeters to more than 2 cm in diameter. In most patients, fewer than five cysts are visible. The cysts are randomly distributed and often associated with ground-glass opacity or mosaic perfusion. They likely result from bronchiolitis and bronchiolar obstruction.
Findings of subacute HP usually resolve within weeks to months if exposure to the antigen is ended or the patient is treated. If exposure is ongoing or repeated exposure occurs, radiographic findings of fibrosis often develop (Fig. 16-10), being superimposed on the nodular opacities or groundglass opacity typical of subacute disease.
Chronic Stage
The chronic stage of HP is characterized by the presence of fibrosis, which may develop months or years after the initial exposure (Table 16-3).
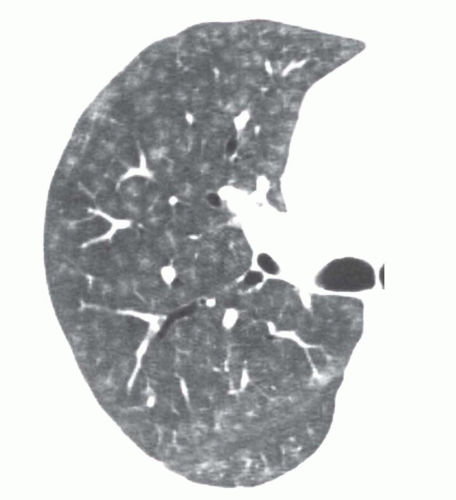
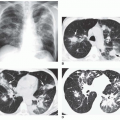
 FIG. 16.3. Subacute hypersensitivity pneumonitis with patchy ground-glass opacity. Scans through the upper and lower lobes show patchy areas of ground-glass opacity. |
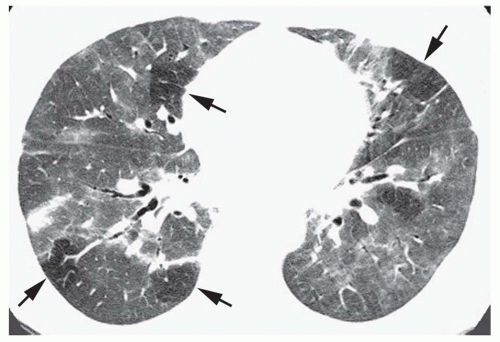
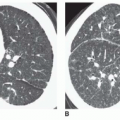
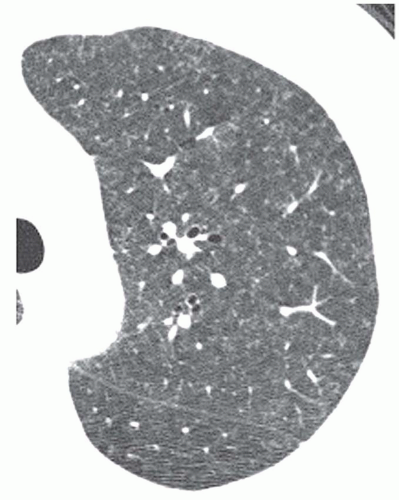 FIG. 16.6. Subacute hypersensitivity pneumonitis with diffuse centrilobular nodules, representing “hot-tub lung.” Small, ill-defined nodules are visible. |
Radiographic Findings
On chest radiographs, radiographic findings of fibrosis include irregular reticular opacities that predominate in the middle lung or lower lung zones and may be parahilar, peribronchovascular, or peripheral in distribution (Fig. 16-11A). A patchy distribution is common. In some cases, fibrosis in HP can mimic the appearance of idiopathic pulmonary fibrosis (IPF) with honeycombing.
HRCT Findings
On HRCT, chronic HP is characterized by fibrosis, although findings of subacute disease are often superimposed (Figs. 16-11,16-12 and 16-13). CT scans show irregular reticular opacities that may be associated with patchy bilateral areas of ground-glass opacity (90%), small ill-defined nodules (60%), areas of reduced lung attenuation due to mosaic perfusion, and air trapping on expiratory scans. In HP, fibrosis is often patchy in distribution or parahilar (see Fig. 16-13), lacking the subpleural predominance of IPF; in some cases it is predominantly subpleural. Honeycombing is not common (20% of cases), but unlike IPF, it may be upper lobe in distribution or often appears patchy or peribronchovascular rather than subpleural (Fig. 16-14).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree