HEART SIZE
Cardiothoracic Ratio
= CT ratio = widest transverse cardiac diameter ÷ widest inside thoracic diameter
| < 0.5 | = | normal in > 1 month old (45% sensitive, 85% specific, 59% accurate) |
| < 0.6 | = | normal in < 1 month old |
Purpose: measurement of LV dilatation
Dependent on:
• lung volume: CT ratio enlarges in expiration
• patient position: CT ratio increases on supine film
Pitfalls:
› no change unless LV volume increases by > ²/³
› no change in moderate enlargement of LA / RV
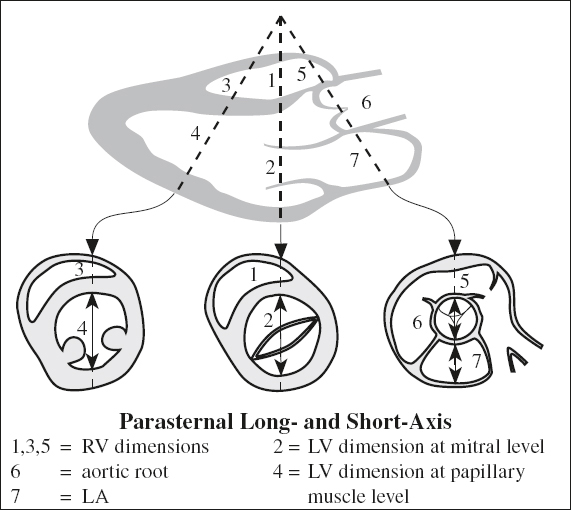
CARDIAC IMAGING PLANES
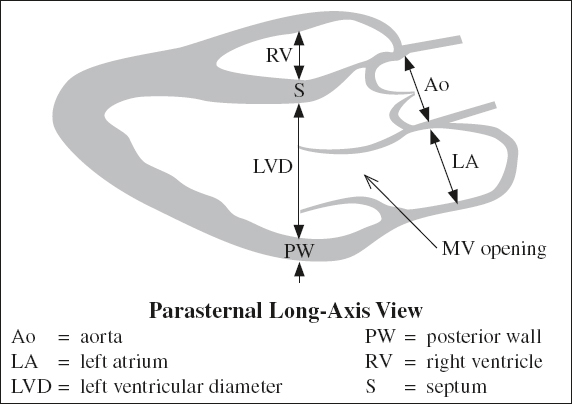
Vertical Long Axis
= parasagittal plane along long axis of LV
Best assessment of:
1. LA and LV (relationship)
2. Inferior + anterior walls of LV myocardium
3. Bicuspid MV (structure & function) versus LV
4. LV (structure & function)
4. LA appendage and coronary sinus
Horizontal Long Axis / 4-Chamber View
= horizontal plane bisecting all 4 chambers
Best assessment of:
1. Chamber size and valve position
2. Septal + apical + lateral LV walls
3. AV valve (subjective assessment in cine mode)
4. Ventricular function (subjective assessment)
5. LA size (quick measurement)
Three-Chamber View
= oblique long-axis view optimizing visualization of LV, LA, aortic root, MV, aortic valve
Best assessment of:
1. LV outflow tract, aortic valve, aortic root, proximal ascending thoracic aorta
2. Posteromedial papillary muscles arising from LV free (lateral) wall
3. Chordae tendineae of MV
Short Axis View
= oblique coronal plane across barrel of LV lumen
1. Basal, middle, apical portions of LV myocardium
2. LV size (easy assessment)
3. LV myocardial contractility (easy assessment)
CARDIAC REPORTING
1. Coronary arteries: origin, course, segmental anatomy
2. Dominance and size of LAD artery, LCx artery, and RCA
3. Number of diagonal + marginal branches
4. Size of heart + cardiac chambers
5. LV function with ejection fraction and wall motion
6. End-diastolic + end-systolic LV volume
7. LV myocardial mass + thickness
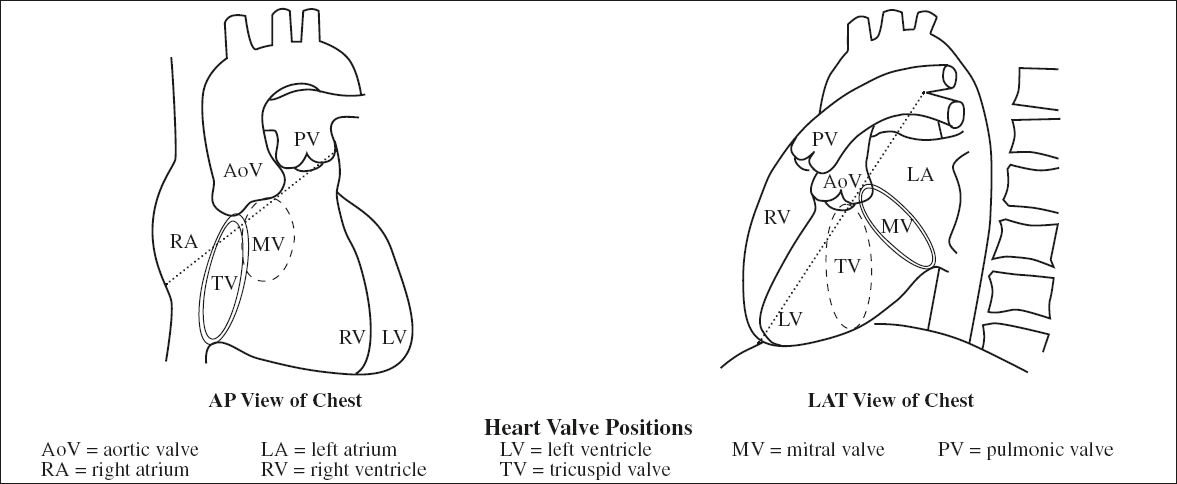
HEART VALVES
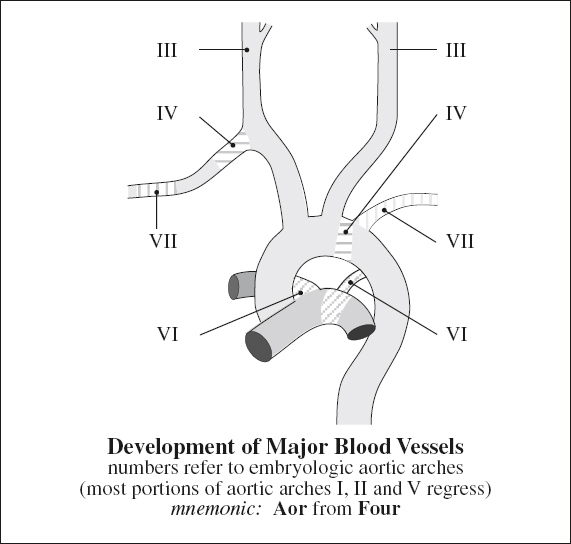
Embryology:
semilunar valves develop simultaneously with formation of RV + right ventricular outflow tract (RVOT) from conotruncal endocardial cushions around distal part of conus
Heart Valve Positions
PA CXR:
reference line = oblique line drawn from distal left mainstem bronchus to right cardiophrenic angle
√ aortic valve resides in profile superior to this line overlying the thoracic spine
√ pulmonic valve just inferior to left mainstem bronchus
√ mitral valve resides inferior to this line centrally located within cardiac silhouette
√ tricuspid valve inferior to this line more basilar and midline
LAT CXR:
reference line = oblique line drawn from carina / right pulmonary artery shadow to anterior cardiophrenic sulcus
√ aortic valve resides superior to this line
√ pulmonic valve anterior + superior to aortic valve
√ mitral valve resides inferoposteriorly to this line
√ tricuspid valve inferior to this line anteriorly
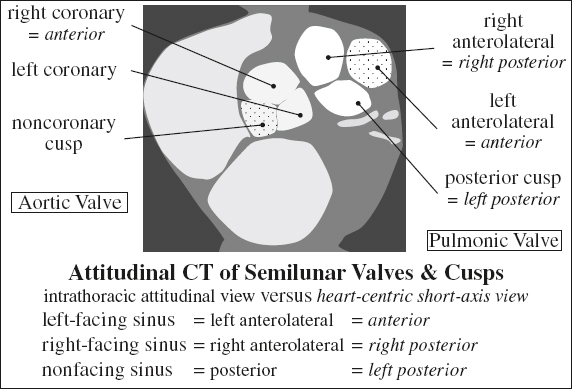
Aortic Valve
= separates LV outflow tract from ascending aorta by a valve composed of annulus, commissures and usually 3 (range, 1 – 4) thin semilunar valve leaflets / cusps
(a) right cusp: inferior to right coronary sinus + origin of RCA
(b) left cusp: inferior to left coronary sinus + origin of LCA

(c) posterior / noncoronary cusp
Nodules of Arantius = thickened fibrous bulge at center of each free cusp margin forming central coaptation area
Commissures = junctions of cusps at attachment to aortic wall at level of sinotubular junction
Area: 2.5 –4.0 cm2
Aortic valve planimetry is optimal during midsystole = 20% of R-R interval or 50–100 msec from R-wave peak!
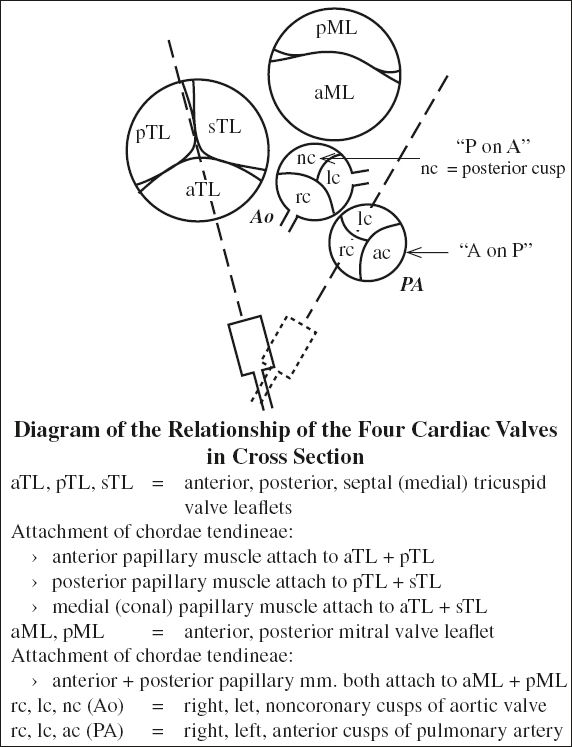
Mitral Valve
= bicuspid valve (= 2 leaflets) anchored on mitral valve annulus + connected to LV papillary muscles by chordae tendineae; MV and aortic valve share fibrous continuity
Area: 4–6 cm2
Circumference: 10 cm
Embryology: develops during 5th–15th week of gestation
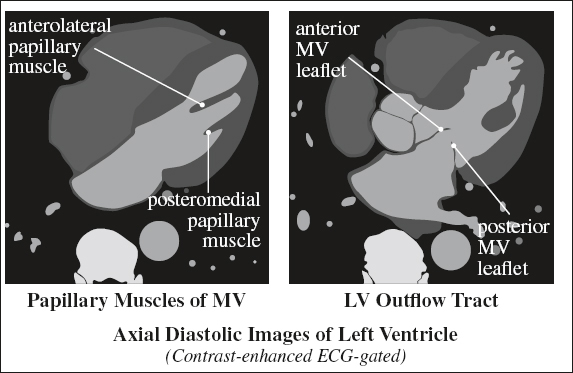
Papillary Muscles of Mitral Valve
Origin: lateral wall of LV
(a) anterolateral papillary muscle
(b) posteromedial papillary muscle (single blood supply)
Prognosis: vulnerable to ischemia + rupture
Mitral Valve Annulus
= D-shaped ring within L atrioventricular groove; imbedded within myocardium as part of cardiac skeleton
(a) straight border = anterior portion of annulus; in fibrous continuity with aortic valve + heart skeleton
(b) curved border = posterior portion of annulus: attached to pliant endocardium
Function: site of valve leaflet attachment
Border: LCx artery + coronary sinus
Mitral Valve Leaflets
Normal thickness: < 5 mm
(a) semicircular anterior leaflet attaches to ⅓ of annulus + forms part of LVOT
Segments: lateral A1, middle A2, medial A3
(b) crescentic posterior leaflet
Segments: lateral P1, middle P2, medial P3
Mitral valve components are best evaluated on reformatted 2-chamber long-axis images perpendicular to the valve during middiastole = 65% of R-R interval for open mitral valve and 5% of R-R for closed mitral valve!
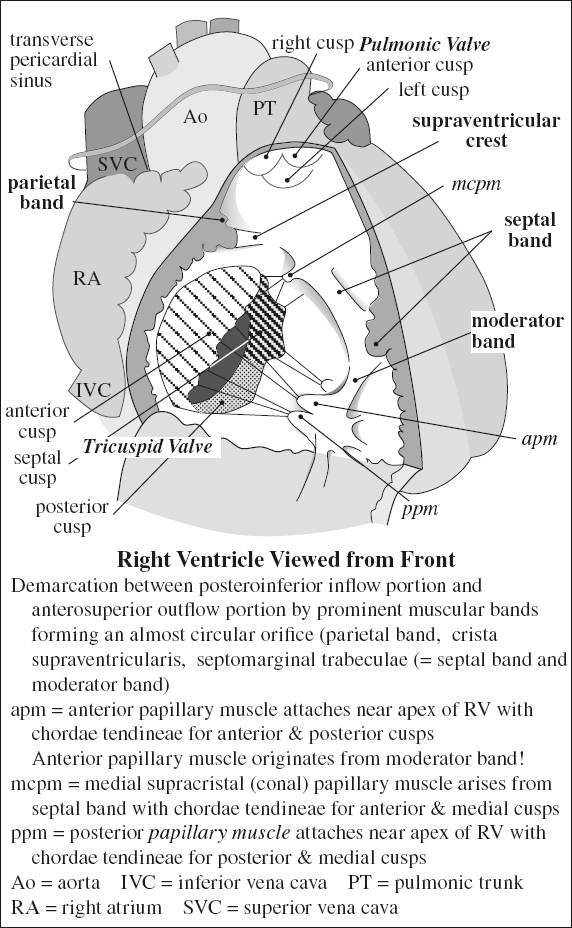
Pulmonic / Pulmonary Valve
= separates RV outflow tract from main pulmonary artery by a semilunar valve composed of 3 cusps (similar to aortic valve although separate from atrioventricular valve)
mnemonic: A cusp on P and P cusp on A anterior cusp (short-axis view) ← pulmonic valve posterior (noncoronary) cusp ← aortic valve
(a) anterior cusp
(b) right cusp
(b) left cusp
Area: 2.0 cm2 / m2 of body surface area
Tricuspid Valve
= right atrioventricular valve separating RA from RV; anchored on tricuspid valve annulus + connected to RV papillary muscles by chordae tendineae; composed of 3 (range, 2 to 4) leaflets
Crista supraventricularis: muscular ridge that separates TV from pulmonary valve
(a) septal leaflet
(b) anterior leaflet
(b) posterior leaflet
VENTRICLES
Right Ventricle
Trabeculae: coarse
Papillary muscles: attached to interventricular septum + free wall; apical moderator band
Differentiating features of RV (from LV):
1. Heavily trabeculated apex
2. Well-developed infundibulum
3. Septal papillary muscles
4. Lack of fibrous continuity of AV valve + outflow tract
Moderator Band
= muscular band extending from interventricular septum to base of anterior papillary muscle
Function: part of right bundle branch conduction system
Right Ventricular Outflow Tract (RVOT)
= smooth muscular infundibulum / conus inferior to PV
In the right ventricle, trabeculae are coarse, and presence of an apical moderator band is CHARACTERISTIC!
Left Ventricle
Trabeculae: thin, delicate, smooth septal surface
Papillary muscles: attached to free wall only
ATRIA
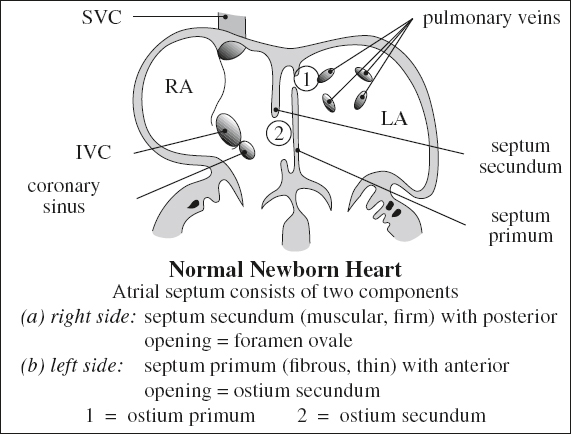
Embryology of Atrial Septa
1. Septum primum = thin partition dividing primitive atrium into right and left atria at 4th week; membrane grows from dorsal atrial wall toward endocardial cushion → ultimately forms thin flap valve of fossa ovalis
2. Ostium primum = temporary orifice between septum primum + endocardial cushions close to AV valves; it becomes obliterated by 5th week
3. Ostium secundum = multiple small coalescing fenestrations in center of septum primum
4. Septum secundum = stiff membrane developing on right side of septum primum growing from right atrial roof → ultimately forms thicker limbus of fossa ovalis
5. Foramen ovale = orifice limited by septum secundum + septum primum
6. Foramen ovale flap = lower edge of septum primum (patent in 6%, probe-patent in 25%); not considered an ASD
Right Atrium (RA)
Components:



(2) venous part
(3) vestibule
Embryology: originates from primitive trabeculated RA (persists as RA appendage) + from sinus venosus forming smooth-walled portion of RA
Right Atrial Appendage
= triangular superior extension of RA that wraps around aortic root
√ pyramidal shape with narrow base
Rx: right atrial lead tip is typically placed at right atrial appendage for pacemaker / internal cardiac defibrillator
Sinus Venosus
› located in posterolateral wall of RA between orifices of SVC and IVC
(a) right horn: gives rise to crista terminalis, eustachian ridge, thebesian valve
(b) left horn: gives rise to coronary sinus
Vestibule of Right Atrium
= smooth muscular rim surrounding tricuspid orifice
Crista Terminalis
= prominent fibromuscular ridge separating smooth-walled venous part of posterior RA (= sinus venosus) from trabeculated muscle fibers of appendage anteriorly
Variations: in size + extent among individuals
Location: junction of sinus venosus and primitive RA
Clinical significance:
thickening of crista terminalis → development of atrial flutter + focal right tachycardias (²/³ arise in crista terminalis) → target for catheter RF ablation
√ vertically oriented smooth muscular ridge varying in size + thickness amongst individuals:
√ small thin valvelike / broad-based structure
√ may be large ← fatty infiltration of crista terminalis in lipomatous hypertrophy of the atrial septum
√ superiorly arches anterior to the orifice of the SVC
√ extends to area of anterior interatrial groove
√ merges with interatrial bundle (= Bachmann bundle)
√ indistinct inferior border located near IVC orifice merging with small trabeculations of inferior portion of cavotricuspid isthmus
› gives rise to thick muscle bundles
(a) anterior pectinate muscles fanning out anteriorly
(b) septum spurium = most prominent anterior pectinate muscle (in 80%) arising from crista terminalis
Mean thickness: 4.5 mm
Sinoatrial Node
= subepicardial spindle-shaped structure as source of cardiac impulse (= dominant pacemaker)
Length: 20 ± 3 mm
Location: in myocardium at superior cavoatrial junction between crista terminalis and SVC
√ surrounds sinoatrial nodal artery, which may course centrally (70%) / eccentrically within node
Koch Triangle
Location: at orifice of coronary sinus
Borders:
› posteriorly: fibrous extension from eustachian valve (tendon of Todaro) = Todaro-eustachian ridge
› anteriorly: attachment of septal leaflet of tricuspid valve
› inferiorly: coronary sinus
› at apex: central fibrous body of heart (= site of penetration of His bundle)
› midportion: contains compact AV node (fast pathway)
› base: bordered by coronary sinus ostium + septal isthmus (= area between edge of coronary sinus ostium + septal tricuspid valve); contains slow pathway
◊ Septal isthmus = frequently target for ablation of slow pathway in AV node reentrant tachycardia!
AV Node
Location: within Koch triangle
Borders:
› coronary sinus ostium
› septal leaflet of tricuspid valve
› tendon of Todaro = fibrous band connecting eustachian and thebesian valves
Importance: electrophysiologists frequently modify this node in dual atrioventricular nodal pathways → AV nodal reentrant tachycardia
Terminal Groove / Sulcus Terminalis
= fat-filled groove on epicardial side corresponding internally to crista terminalis close to cavoatrial junction
› location of sinus node + terminal segment of sinoatrial nodal artery
Eustachian Valve
[Bartolomeo Eustachi (1500 or 1514–1574), one of the founders of the science of human anatomy in Rome, Italy]
= valve of inferior vena cava (guarding entrance into IVC)
Function: directs flow toward foramen ovale
Location: junction of RA and IVC; inserts medially onto eustachian ridge (= border between oval fossa + coronary sinus)
› directs blood from IVC to foramen ovale in fetus
› free border continues as tendon of Todaro
√ thin linear structure, not routinely imaged
◊ Rarely an unusually large muscular valve may pose an obstacle to passage of a catheter!
Cavotricuspid Isthmus
= area between IVC + tricuspid valve of highly variable isthmian anatomy
◊ Target of catheter ablation as treatment of choice for isthmus-dependent atrial flutter!
N.B.: obstacles to successful ablation may be a large eustachian ridge, aneurysmal pouches, or a concave deformation of the entire isthmus
Thebesian Valve
= valve of coronary sinus
[Adam Christian Thebesius (1686–1732), anatomist and municipal physician in Hirschberg, Silesia]
Prevalence: in 80% of cadaveric specimens
Function: prevents reflux from RA into coronary sinus
Location: entry of coronary sinus into RA
Morphology: complete circular (30%), crescentic (35%), absent (20%), threadlike (2%), fenestrated (10%)
√ thin semilunar fold at anteroinferior rim of coronary sinus ostium
Mechanical barrier: large eustachian valve / ridge (25%), > 5 mm deep subthebesian recess (45%), hypoplastic coronary sinus ostium, large thebesian valve
Subthebesian Pouch
= subeustachian sinus = sinus of Keith
= pouchlike atrial wall inferior to orifice of coronary sinus
Depth: 4.3 ± 2.1 (range, 1.5–9.4) mm
◊ Substrate for reentrant circuit during atrial flutter
N.B.: main source of RF procedural difficulty
Interatrial Septum
| Septum | = | wall that can be removed without exposing heart cavity to extracardiac structures |
Parts: flap valve of foramen ovale (septum primum) + part of its anteroinferior margin
◊ Superior rim of fossa (septum secundum = infolded wall between SVC and right pulmonary veins) is not a true septum!
√ thin septum that is difficult to image
√ may contain small amount of fat sparing fossa ovalis
DDx: Lipomatous hypertrophy of interatrial septum
√ characteristic dumbbell shape ← sparing of fossa ovalis
√ abnormal amount of fat in older / obese adults
Fossa Ovalis
= circular indentation in interatrial septum
Variant: patent fossa ovalis / foramen ovale
PATENT FORAMEN OVALE
= PATENT FOSSA OVALIS
Prevalence: 15%
Function: can result in R-to-L shunt
Associated with:
paradoxical emboli, cryptogenic stroke, hypoxemia in patients with obstructive sleep apnea, increased risk for decompression sickness, increased risk for atrial fibrillation after cardiac surgery
√ demonstrated by contrast-enhanced echocardiography
Left Atrium (LA)
Components: venous component, vestibule, appendage
Embryology: originates from primitive trabeculated LA (persists as LA appendage) + from pulmonary veins forming smooth-walled portion of LA
√ smooth walled venous + septal component + vestibule
√ ridge of smooth muscle (± bulbous tip) at junction of LA appendage and entrance of left superior pulmonary vein
Venous Component of Left Atrium
= located posteriorly → pulmonary vein orifices at each corner
Left Atrial Vestibule
= surrounds the mitral orifice
Left Atrial Appendage
= arises from superolateral aspect of LA
√ rough trabeculated surface of tubular shape
√ projects anteriorly over proximal LCx artery
√ 3.5–6.5 mm thick superior wall / dome
Cx: narrow neck predisposes to thrombus deposition
Atrial Appendages
√ linear filling defects (R > L) = pectinate muscles fibers running parallel to each other measuring > 1 mm (in 97%)
DDx: thrombus in LA
CORONARY ARTERIES
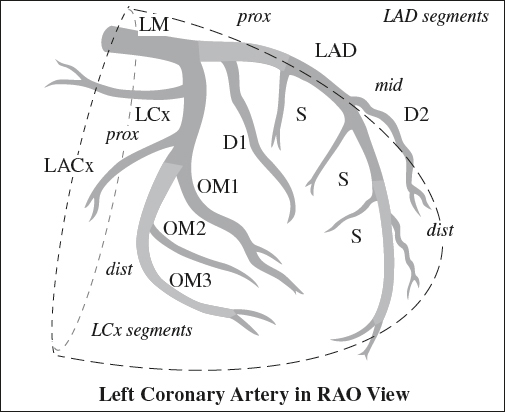
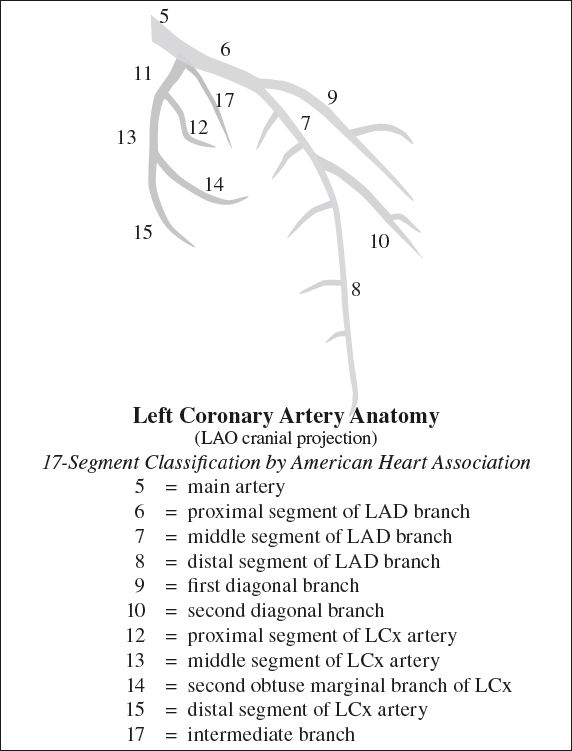
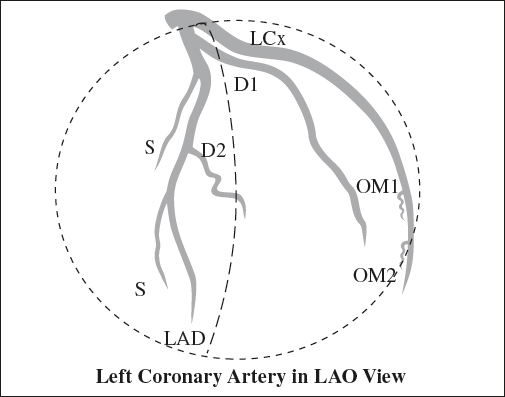
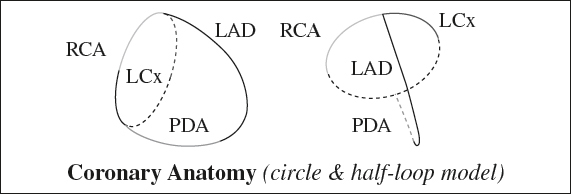
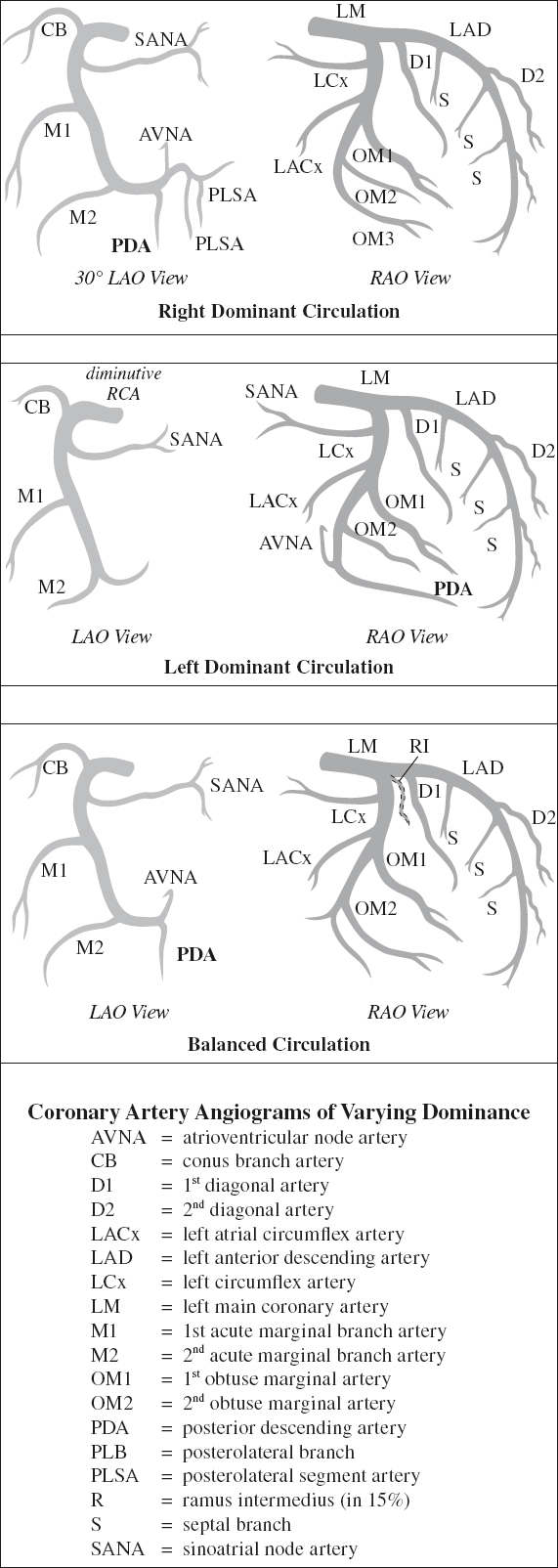
Anatomy of Left Coronary Artery (LCA)
arises from left (posterior) coronary sinus (= left sinus of Valsalva) near sinotubular ridge; passes to left and posterior to pulmonary trunk
1. Left main coronary artery (LM)
Segments: ostium to bifurcation = 5–20 mm short stem
› bifurcates into LAD + LCx
› trifurcates (in 15%) = ramus intermedius (RI) branch coursing laterally toward LV free wall similar to D1
2. Left anterior descending (LAD)
Course: within anterior interventricular groove toward apex
Supply: majority of LV + anterolateral papillary muscle ± small branches to anterior RV wall
Segments:
› proximal: from left main bifurcation to origin of 1st septal branch
› midportion: from 1st septal branch to an acute angle (may coincide with origin of 2nd septal perforator)
– otherwise split halfway between 1st septal perforator and apex into:
› middle LAD
› distal LAD
› apical segment = termination of LAD
(a) Diagonal perforating branches (D1, D2, etc) arise from LAD, course over anterolateral wall of LV
Supply: LV free wall
mnemonic: Diagonals course downward from LAD
(b) Septal perforating branches (S) course medially toward anterior interventricular septum
Supply: majority of interventricular septum + AV bundle + proximal bundle branch
3. Left circumflex artery (LCx) travels within left atrioventricular sulcus (groove);
terminates at obtuse (blunt / round) margin of heart
(a) Obtuse marginal (lateral) branches (OM1, OM2, etc)
for lateral wall of LV
(b) Left atrial circumflex artery (LACX) for atrium
(c) variably: branches to posterolateral + posterior descending artery supplying diaphragmatic portion of LV (= left dominance)
Supply: LV free wall + variable portion of anterolateral papillary muscle
Terminology from surface perspective of apical view:
› rounded obtuse margin of heart formed mainly by LV
› sharp angle = acute margin of heart formed mainly by RV
Segments: proximal + distal (based on origin of large obtuse marginal branches)
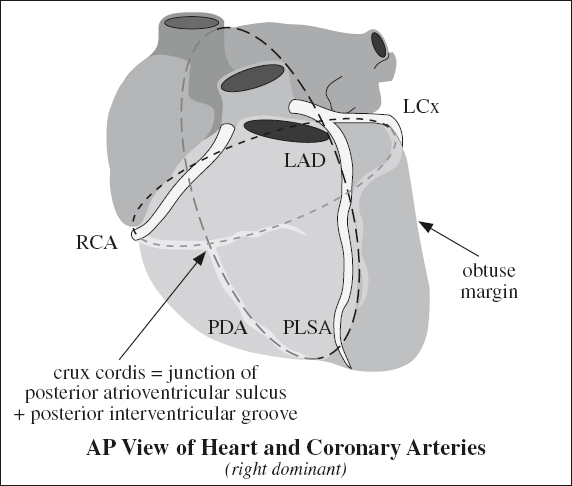
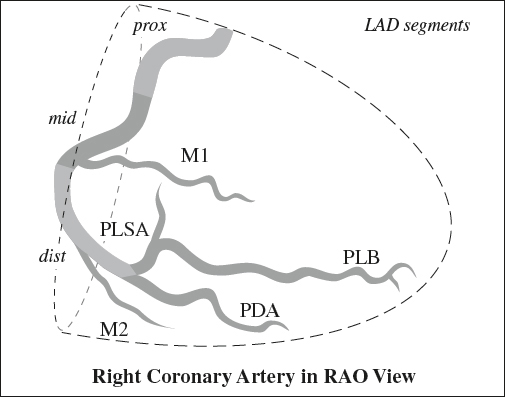
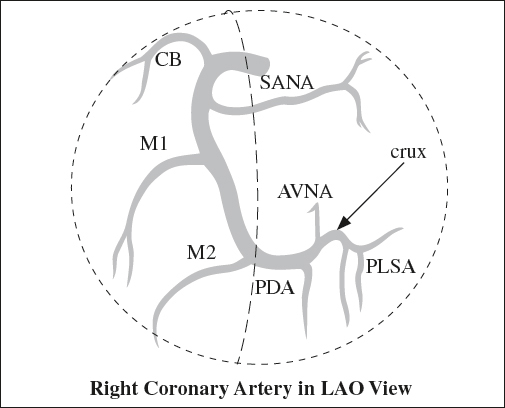
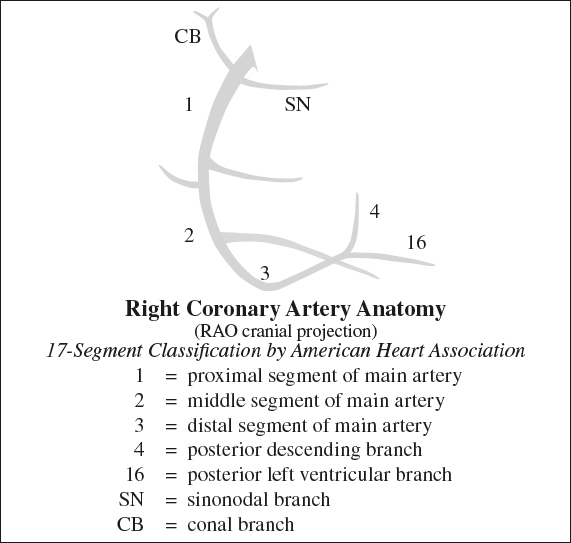
Anatomy of Right Coronary Artery (RCA)
arises from right (anterior) coronary sinus → passes to right + posteriorly to pulmonary artery → travels downward within right atrioventricular sulcus (groove) → rounds the acute margin of the heart toward crux
Terminology based on posterior surface view of heart:
crux cordis = cross formed by
› AV groove (transecting a line formed by)
› posterior interventricular + interatrial sulci
[crux, Latin = cross, junction]
Segments:
› proximal: ostium to halfway to acute margin of heart
› mid:
› distal: acute angle of heart to origin of PDA
1. Conus artery (CB)
= 1st branch of RCA (in 50–60% of patients); may originate directly from coronary sinus of aorta (in 30–35%)
√ forms circle of Vieussens = anastomosis with LAD
Supply: RVOT = conus arteriosus
2. Sinoatrial node artery (SANA)
= 2nd branch of RCA (in 60%) / from LCx (in 40%)
√ courses along anterior interatrial groove toward superior cavoatrial junction
√ at cavoatrial junction circling either anteriorly (precaval) / posteriorly (retrocaval) to enter node
3. Marginal branches (M1, M2, etc) have an anterior course
› acute marginal branch = at junction of middle + distal RCA
Supply: RV
4. Posterior descending artery (PDA)
= origin of PDA determines coronary artery dominance
Origin: usually RCA near crux (in 70%) / distal acute marginal branch (= right dominance)
Supply: posterior third of ventricular septum + diaphragmatic segment of LV + posteromedial papillary muscle
5. Atrioventricular node artery (AVNA)
= small branch to AV node
Origin: apex of U-turn of distal RCA (80–87%) / terminal portion of LCx (8–13%) / both RCA and LCx (2–10%)
Supply: posterior interventricular septum, interatrial septum, AV node, His bundle
√ penetrates base of posterior interatrial septum at crux
√ may course beneath endocardium near ostium of coronary sinus + septal isthmus
◊ High risk for AV nodal artery coagulation during RF ablation!
6. Posterolateral segment arteries (PLSA)
supplies posterolateral wall of LV
Coronary Artery Territory
| septum | = | LAD |
| anterior wall | = | LAD |
| lateral wall | = | LCx |
| posterior wall | = | RCA |
| inferior / diaphragmatic wall | = | RCA |
| apex + inferolateral wall | = | watershed areas |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree