= INFRAORBITAL ETHMOIDAL AIR CELL = MAXILLOETHMOIDAL / ORBITOMAXILLARY CELL
= anterior ethmoid air cells inferolateral to ethmoidal bulla, on lateral wall of infundibulum, along inferior margin of orbit / roof of maxillary sinus, protruding into maxillary sinus
Prevalence: 2–10–45%
Significance: may narrow ipsilateral ostiomeatal complex if large → obstruction of ipsilateral maxillary antrum
(b) posterior ethmoid air cells
1–8 cells, larger cells, total area smaller than that of anteromedial group
| Location: | behind the basal (= ground) lamella of the middle turbinate |
| Ostium: | into superior meatus / supreme meatus, ultimately draining into sphenoethmoidal recess of nasal cavity |
Onodi cell
= most posterior ethmoid air cell pneumatized into sphenoid bone ± surrounding the optic canal
Location: superolateral to sphenoid sinus
Frontal Sinus
Size: 28 x 24 x 20 mm in adults, rapid growth until late teens
Walls: posterior wall = anterior cranial fossa; inferior wall = anterior portion of roof of orbit
Ostium: into frontal recess of middle meatus via frontoethmoidal recess (= nasofrontal duct)
Outflow tract: frontal infundibulum + frontal ostium + frontal recess
Plain film: visible at age 6 years
Variations: sinus aplasia in up to 4% (in 90% with Down syndrome)
Frontal Recess = Frontoethmoidal Recess
| Walls: | agger nasi cell anteriorly; lamina papyracea laterally; middle turbinate medially; ethmoid cell with bulla lamella posteriorly |
Frontal Recess Cells (20–33%)
= pneumatization of frontal recess by various anterior ethmoid cells
Relevance: obstruction of frontal sinus outflow
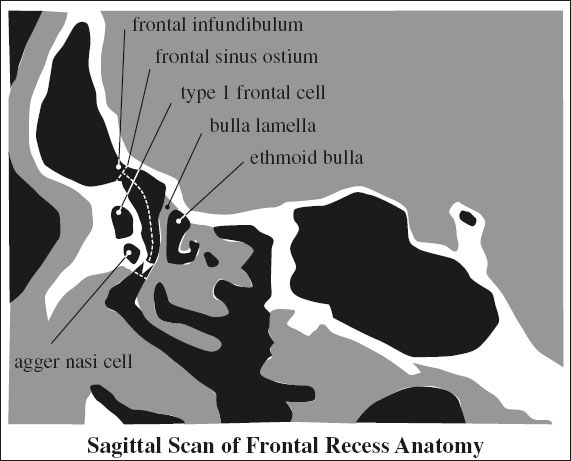
› Type 1 frontal cell (in up to 37%)
= single anterior ethmoid cell within frontal recess above agger nasi cell
› Type 2 frontal cell (in up to 19%)
= tier of > 2 anterior ethmoid cells above agger nasi cell
› Type 3 frontal cell (in up to 7%)
= single massive cell above agger nasi pneumatizing into frontal sinus
› Type 4 frontal cell (2%)
= isolated air cell along anterior wall of frontal sinus not abutting the agger nasi cell
(b) posterior group
1. Supraorbital ethmoid cell (in up to 15%)
= pneumatized orbital plate of frontal bone posterior to frontal recess mimicking septated frontal sinus = anterior ethmoid air cell extending from frontal recess superiorly + laterally over orbit
2. Frontal bullar cell
= pneumatized anterior skull base atop ethmoid bulla with extension into frontal sinus as part of posterior boundary of frontal recess + sinus
3. Suprabullar cell
= atop ethmoid bulla but below level of frontal sinus ostium without extension into frontal sinus as part of posterior boundary of frontal recess
4. Interfrontal sinus septal cell
= pneumatized interfrontal sinus septum; may extend into crista galli
Sphenoid Sinus
Size: 20 x 23 x 17 mm in adults, small evagination of sphenoethmoidal recess at birth, invasion of sphenoid bone begins at age 5 years; aerated extensions into pterygoid plates (44%) + into clinoid processes (13%)
Walls: roof = floor of sella turcica; anterior wall shared with ethmoid sinuses; posterior wall = clivus; inferior wall = roof of nasopharynx
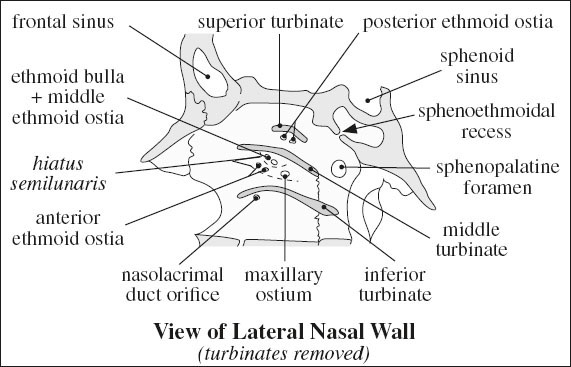
Ostium: 10 mm above sinus floor into sphenoethmoidal recess posterior to superior meatus at level of sphenopalatine foramen
Plain film: appears by 3 years of age; continues to grow posteriorly + inferiorly into the sella until adulthood
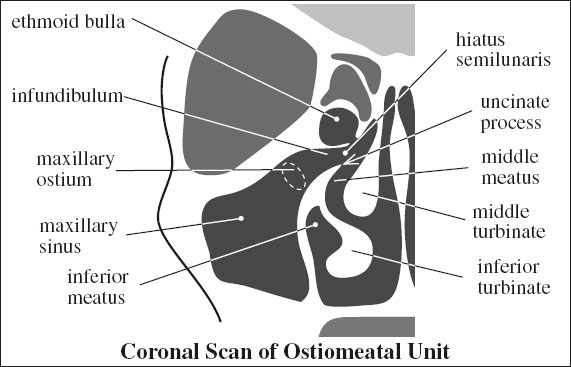
OSTIOMEATAL UNIT
= area of superomedial maxillary sinus + middle meatus as the common mucociliary drainage pathway of frontal maxillary, and anterior + middle ethmoid air cells into the nose
Coronal CT: visualized on two or three 3-mm–thick sections
Components:
Infundibulum
= flattened conelike passage between inferomedial border of orbit / ethmoid bulla (laterally) + uncinate process (medially) + maxillary sinus (inferiorly) + hiatus semilunaris (superiorly)
Uncinate process
= key bony structure in lateral nasal wall below hiatus semilunaris in middle meatus defines hiatus semilunaris together with adjacent ethmoid bulla
Attachment: skull base / middle turbinate / lamina papyracea / agger nasi
√ pneumatized in < 2.5% of patients
Ethmoid bulla
√ located in cephalad recess of middle meatus
Hiatus semilunaris
= final segment for drainage of maxillary sinus; located just inferior to ethmoid bulla in middle meatus
Ostia:
(1) Multiple ostia from anterior ethmoid air cells (at its anterior aspect)
(2) Maxillary ostium infundibulum (at its posterior aspect)
Anatomic variations predisposing to ostiomeatal narrowing:
1. Concha bullosa (4–15%) = aerated / pneumatized middle turbinate
2. Intralamellar cell = air cell within vertical portion of middle turbinate
3. Oversized ethmoid bulla
4. Haller cell
5. Uncinate process bulla
6. Bowed nasal septum
7. Paradoxical middle turbinate = convexity of turbinate directed toward lateral nasal wall (10–26%)
8. Deviation of uncinate process
◊ These conditions are not disease states per se!
FACIAL BUTTRESSES
= areas of relatively increased bone density that support functional units of the face (muscles, eyes, dental occlusion, airways)
› sufficient bone thickness to accommodate metal screw fixation
› linked directly / through another buttress to cranium / skull base
(a) horizontal buttresses
• responsible for facial height
(1) Upper transverse maxillary buttress: temporal squamosa → zygomatic arch → inferior orbital rim → nasofrontal junction
Posterior extension: orbital floor
(2) Lower transverse maxillary buttress: maxilla above alveolar ridge
Posterior extension: hard palate
(3) Upper transverse mandibular
(4) Lower transverse mandibular
(b) vertical buttresses
• responsible for facial profile and width
(1) Medial maxillary buttress: anterior nasal spine → rim of piriform aperture → frontal process of maxilla → nasofrontal junction → frontal bone
Posterior projection: medial orbital wall
Anterior projection: lateral nasal wall
(2) Lateral maxillary buttress: above posterior maxillary molar → zygomaticomaxillary suture → body of zygoma → lateral orbital rim → zygomaticofrontal suture → frontal bone
Posterior projection: lateral orbital wall, lateral wall of maxillary sinus
(3) Posterior maxillary buttress: pterygomaxillary junction
(4) Posterior vertical buttress
BRANCHIAL CLEFT DEVELOPMENT
Branchial apparatus: branchial arches, pharyngeal pouches, branchial grooves, branchial membranes
› 6 paired branchial arches are responsible for formation of lower face + neck; recognizable by 4th week GA
› each branchial arch contains a central core of cartilage + muscle, a blood vessel, and a nerve
› 5 ectodermal “clefts” / grooves on outer aspect of neck + 5 endodermal pharyngeal pouches separate the 6 arches with a closing membrane located at the interface between pouches and clefts
Formation: during 4th–6th week of embryonic development
1st Branchial Arch = maxillomandibular arch
(a) large ventral / mandibular prominence
forms: mandible, incus, malleus, muscles of mastication
(b) small dorsal / maxillary prominence
forms: maxilla, zygoma, squamous portion of temporal bone, cheek, portions of external ear
nerve: mandibular division of trigeminal nerve (CN V3)
pouch forms: mastoid air cells + eustachian tube
cleft forms: external auditory canal + tympanic cavity
2nd Branchial Arch = hyoid arch
nerve: facial nerve (CN VII)
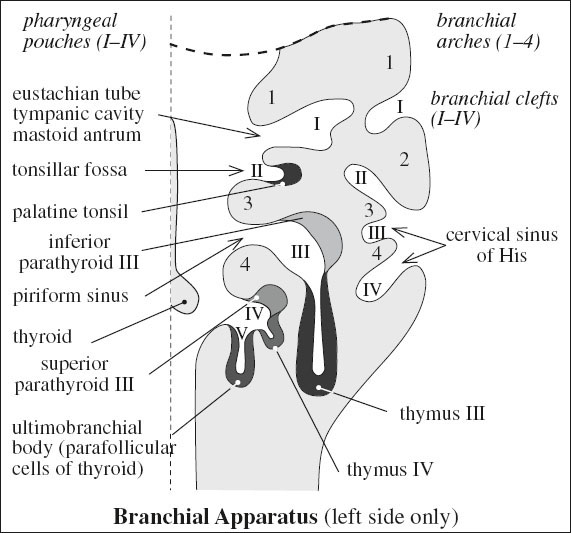
arch forms: thyroid gland, stapes, portions of external ear, muscles of facial expression
pouch forms: palatine tonsil + tonsillar fossa
→ cleft involutes completely by 9th fetal week; 2nd arch overgrows 2nd + 3rd + 4th clefts to form cervical sinus, which creates a tract that runs from the supraclavicular area just lateral to carotid sheath, turns medially at mandibular angle between external + internal carotid artery, and terminates in tonsillar fossa
3rd Branchial Arch
sinks into retrohyoid depression
nerve: glossopharyngeal nerve (CN IX)
arch forms: glossoepiglottic fold, superior constrictor m., internal carotid a., parts of hyoid bone
pouch forms:
(a) thymus gland, which descends into mediastinum by 9th fetal week
(b) inferior parathyroid glands passing down with the thymus
4th Branchial Arch
sinks into retrohyoid depression
nerve: superior laryngeal branch of vagus nerve (CN X)
| arch forms: | epiglottis + aryepiglottic folds, thyroid cartilage, cricothyroid m., left component of aortic arch, right component of right proximal subclavian a. |
| pouch forms: | superior parathyroid glands, apex of piriform fossa |
| cleft forms: | ultimobranchial body, which provides parafollicular (“C”) cells of thyroid |
5th + 6th Branchial Arches
cannot be recognized externally
nerve: recurrent laryngeal branch of vagus nerve (CN X)
TONGUE
= complex of muscle groups + fibrous scaffolding
A. FIBROUS SCAFFOLDING
1. Hyoglossal membrane
anchors inferior posterior edge of tongue to hyoid bone
2. Midline lingual septum
inserts into hyoglossal membrane + extends superiorly along midline of tongue dividing tongue into halves + providing attachments for transverse intrinsic muscles
B. INTRINSIC MUSCLES (named for their orientation):
Function: wide range of motion for mobile tongue
› vertical + transverse
› inferior + superior longitudinal
C. EXTRINSIC MUSCLES
Function: raising + lowering of tongue, forward + backward motion
1. Genioglossus m.
Origin: symphysis menti on back of mandible
Insertion: dorsum of tongue (interdigitating with intrinsic tongue muscles); hyoid bone (few inferolateral fibers)
2. Geniohyoid m.
Origin: symphysis menti on back of mandible
Insertion: hyoid bone
3. Hyoglossus m.
Origin: hyoid bone
Insertion: lateral aspect of tongue
4. Styloglossus m.
5. Palatoglossus m.
Anatomic subdivision:
(A) Mobile tongue (part of oral cavity)
= frenulum to circumvallate papillae
› “Root of tongue”
= region deep to mobile tongue + anterior to base of tongue
| Parts: | (1) | Lingual septum |
| (2) | Genioglossus-geniohyoid complex = both genioglossus m. + geniohyoid m. |
Borders:
(a) anterior: mandible
(b) lateral: sublingual space
(c) inferior: U-shaped mylohyoid m. underneath geniohyoid m.
(c) superior: indistinct ← genioglossus m. fans out and blends with intrinsic tongue muscles
(B) Base of tongue (part of oropharynx)
= posterior to circumvallate papillae
ORAL CAVITY
= most ventral portion of aerodigestive tract
Borders:
| (a) inferior: | circumvallate papillae |
| (b) superior: | soft palate |
| (c) lateral: | anterior tonsillar pillars |
Anatomic subdivisions:
lips; floor of mouth; oral tongue (= anterior ⅔ of tongue); buccal mucosa; upper + lower gingiva; hard palate;
retromolar trigone
Sites of squamous cell carcinoma: lower lip > oral tongue > floor of mouth (in 75%)
Floor of Mouth
= horizontally aligned U-shaped space situated in the part of the oral cavity that lies beneath the tongue between mucosal surface and mylohyoid muscle sling
Anatomic components:
1. Squamous epithelium of mucosal surface
2. Mylohyoid muscle sling (paired)
[mylai, Greek = molar (mill) teeth]
separates floor of mouth from R + L submandibular spaces and midline submental space
Origin: inner surface of mandible from symphysis menti to last molar posteriorly
Insertion: fibrous median raphe (medially), posterior aspect of hyoid bone (midline); free edge (posterolaterally) allowing communication between sublingual + submandibular space
• palpable lump ← herniated sublingual salivary gland mylohyoid defect into adjacent submandibular space
√ boutonniere = defect in mylohyoid m. (77% of CTs)
3. Sublingual space
= located on both sides of tongue, superomedial to mylohyoid m. and lateral to midline geniohyoid-genioglossus muscle complex
Content:
› lingual artery (medial to hyoglossus m.)
› lingual vein + main submandibular duct (lateral to hyoglossus m.) coursing between hyoglossus + mylohyoid mm.
√ higher T1 + T2 signal ← higher fat + connective tissue content
4. Submandibular space
5. Submental space
Content: salivary glands (see below); nerves (lingual n. = branch of mandibular division of trigeminal nerve with input from chorda tympani branch of facial n.), distal portions of hypoglossal n. and glossopharyngeal n.
Salivary Glands at Floor of Mouth
1. Sublingual glands
Excretion via:
(a) Rivinus ducts = numerous small ducts that open at mucosa of floor of mouth
(b) Bartholin duct = formation of a common duct from joining of several of more anterior ducts typically emptying into main submandibular duct
2. Deep portion of submandibular glands
Excretion via: Wharton duct = main submandibular duct coursing anteriorly through sublingual space from deep aspect of submandibular gland
Orifice: sublingual papilla on ipsilateral side of frenulum, anterior to sublingual gland
3. Subepithelial minor salivary glands
PHARYNX
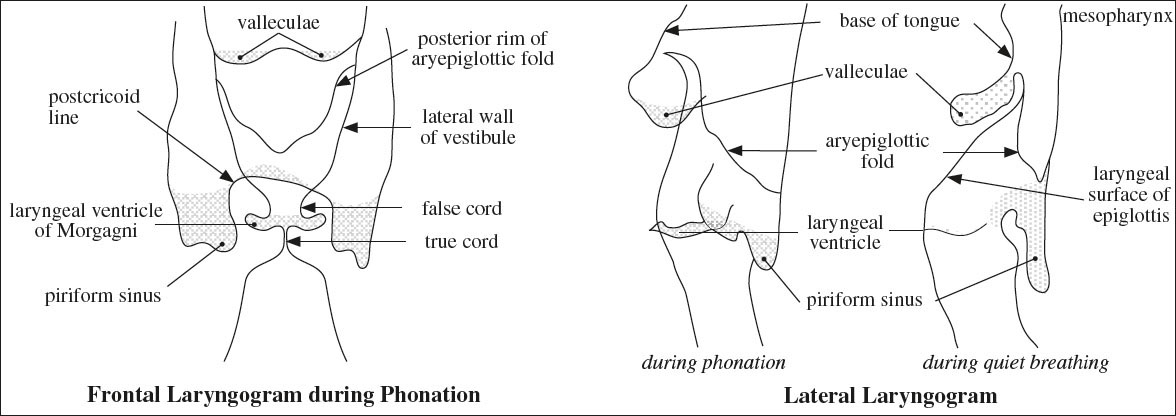
Barium Pharyngography:
Patient maneuvers:
(a) modified Valsalva maneuver = patient puffs out cheeks as if blowing a trumpet
(b) phonation = patient phonating letter E → widening of oropharynx + deepening of valleculae with forward movement of tongue
Technique: videofluoroscopic recording
› patient standing in upright position
› initial swallow with high-density barium assessing for aspiration, leak, stricture, obstruction, delayed emptying on lateral view
› second swallow to coat oro- and hypopharynx in LAT + AP projection during maneuvers
› solid-column evaluation for inferior hypopharynx
The pharynx is divided into oropharynx and hypopharynx by the pharyngoepiglottic fold, which is not seen at barium pharyngography. Instead the base of the free margin of the epiglottis / hyoid bone are used as a proxy landmark.
Normal variants:
1. Lateral protrusion of superior ⅓ of lateral hypopharyngeal wall
Cause: weakening of thyrohyoid membrane in elderly / glassblower / trumpet player
√ symmetric bilateral outward bulge of superior aspect of lateral wall of piriform sinus, more pronounced during modified Valsalva maneuver
2. Mild asymmetry of vallecular pouches due to lymphoid tissue
Structural abnormalities of the pharynx are diagnosed by a change in the normal coated surfaces / an alteration in density.
Oropharynx
consists of
(a) oropharyngeal mucosa (pharyngeal wall between nasopharynx + pharyngoepiglottic fold)
(b) soft palate
(c) palatine tonsils
(d) base of tongue (= posterior ⅓ of tongue)
Borders:
(a) superior: soft palate and Passavant ridge (= ridge of pharyngeal muscle that opposes the soft palate when soft palate is elevated)
[Philippas G. Passavant, German surgeon, 1815–1893]
(b) anterior: plane formed by the posterior border of soft palate, anterior tonsillar pillars, circumvallate papillae
(c) posterior: posterior pharyngeal wall
(d) inferior: valleculae
[valles, Latin = valley → vallecula = little valley]
(e) lateral: tonsillar region consisting of anterior tonsillar pillar (= palatoglossus m.) + palatine / faucial tonsil + posterior tonsillar pillar (= palatopharyngeus muscle)
Anatomic subdivisions: base of tongue; tonsils
Tonsillar complex: tonsillar fossa + tonsillar pillars
Barium Pharyngography:
√ valleculae = paired symmetric structures divided by median glossoepiglottic fold posteroinferior to tongue base
√ free margin of epiglottis projects posterior + superior to valleculae
√ cornua of hyoid project on end with change in position during swallowing
√ slightly nodular surface of base of tongue superior to valleculae
√ aryepiglottic fold covers posterior surface of arytenoid cartilage
Hypopharynx
= LARYNGOPHARYNX
= compartment of aerodigestive tract posterior to supraglottic larynx bridging oropharynx above + esophagus below
Origin: derived from 4th branchial arch (= buccopharyngeal bud) → rich lymphatic drainage directed cranially to upper deep jugular chain (levels II + III)
Superior boundary: valleculae at level of hyoid bone
Inferior boundary: lower edge of cricopharyngeus m. = lower edge of cricoid cartilage
1. Piriform sinus [pirum, Latin = pear; forma, Latin = shape → pear-shaped]
= two symmetric lateral stalactites of air hanging from hypopharynx behind larynx
› inferior wall: level of cricoarytenoid joint
› anteromedial wall: lateral wall of aryepiglottic fold
› lateral wall: abuts posterior ala of thyroid cartilage
› posterior wall: most lateral aspect of posterior hypopharyngeal wall
2. Postcricoid area = pharyngoesophageal junction extends from level of arytenoid cartilages to inferior border of cricoid cartilage
› anterior wall of hypopharynx = posterior wall of lower larynx = “party wall”
3. Posterior hypopharyngeal wall extends from level of valleculae to cricoarytenoid joints
Barium Pharyngography:
√ lateral walls of piriform sinuses = lateral margins of hypopharynx
√ “postcricoid line” = coated mucosal surface ← larynx pressing on anterior wall of hypopharynx
√ barium coating of inner anterior surface of laryngeal vestibule ± laryngeal ventricle ← laryngeal penetration + aspiration
LARYNX
Vertical length: 44 mm (males), 36 mm (females), at 4th–6th cervical vertebrae (from tip of epiglottis to lower end of cricoid cartilage)
| Function: | (1) | Protection against aspiration |
| (2) | Phonation |
Lymphatic drainage:
(a) supraglottis: rich drainage directed cranially to upper deep jugular chain (levels II + III)
(b) glottis + subglottis: sparse drainage directed inferiorly to lower deep jugular + paratracheal nodes (levels IV + VI)
Supraglottis
extends from tip of epiglottis to laryngeal ventricle
derived from 4th branchial arch (= buccopharyngeal bud)
1. Vestibule = airspace within supraglottic larynx
2. Epiglottis
= leaf-shaped cartilage that functions as a lid to endolarynx
(a) petiole = stem of epiglottis
(b) thyroepiglottic ligament = connects petiole to thyroid cartilage inferiorly
(c) hyoepiglottic ligament = connects epiglottis to hyoid bone anteriorly, covered by a mucosal fold between the valleculae (glossoepiglottic fold)
(d) “free margin” = superior portion of epiglottis
3. False vocal cords
= ventricular folds = inferior continuation of aryepiglottic folds = mucosal surface of ventricular ligaments; forming superior border of laryngeal ventricle
4. Arytenoid cartilages
5. Aryepiglottic folds
= mucosal reflections between cephalad portion (= arytenoid processes) of arytenoid cartilage + inferolateral margin of epiglottis
√ soft-tissue folds forming border between lateral piriform sinuses + central laryngeal lumen
6. Laryngeal ventricle of Morgagni
= slitlike fusiform cavity between true + false cords
Boundary: crescentic edge of false cords superiorly + straight margin of true cords inferiorly
√ generally not visible on axial scans
7. Laryngeal saccule of Hilton = laryngeal appendix
= small conical mucosa-lined blind pouch (diverticulum) arising from anterosuperior third of laryngeal ventricle
Boundary: superiorly between ventricular fold (= false vocal cord) and aryepiglottic fold medially + inner surface of thyroid cartilage laterally
Function: lubrication of vocal folds
√ relatively large in infancy
√ usually involutes by 6th year of life
8. Preepiglottic space
Boundary: hypoepiglottic lig. (superiorly), thyrohyoid membrane (anteriorly), thyroepiglottic lig. (inferiorly), epiglottis (posteriorly)
9. Paraglottic (paralaryngeal) space
Boundary: quadrangular membrane + medial piriform sinus wall (superiorly), conus elasticus (inferiorly), thyroid cartilage (laterally)
√ low-density tissue between true + false cords
√ contiguous with preepiglottic space anterosuperiorly + aryepiglottic folds superiorly
Glottis
Boundary: from laryngeal ventricles to imaginary plane 1 cm below laryngeal ventricles
Origin: 5th branchial arch (= tracheobronchial bud)
1. True vocal cords
= extend from vocal process of arytenoid cartilage to anterior commissure
√ vocal cords adduct during phonation of “E” / breath holding
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree