Age of mother at term (years)
Risk for trisomy 21 (Down syndrome) (%)
Total risk for any chromosome abnormalityb (%)
20c
1/1667
0.06
1/526
0.2
21
1/1429
0.07
1/526
0.2
22
1/1429
0.07
1/500
0.2
23
1/1429
0.07
1/500
0.2
24
1/1250
0.08
1/476
0.2
25
1/1250
0.08
1/476
0.2
26
1/1176
0.09
1/476
0.2
27
1/1111
0.09
1/455
0.2
28
1/1053
0.09
1/435
0.2
29
1/1000
0.10
1/417
0.2
30
1/952
0.11
1/384
0.3
31
1/909
0.11
1/384
0.3
32
1/769
0.13
1/323
0.3
33
1/625
0.16
1/286
0.3
34
1/500
0.20
1/238
0.4
35
1/385
0.26
1/192
0.5
36
1/294
0.34
1/156
0.6
37
1/227
0.44
1/127
0.8
38
1/175
0.57
1/102
1.0
39
1/137
0.73
1/83
1.2
40
1/106
0.94
1/66
1.5
41
1/82
1.2
1/53
1.9
42
1/64
1.6
1/42
2.4
43
1/50
2.0
1/33
3.0
44
1/38
2.6
1/26
3.8
45
1/30
3.3
1/21
4.8
46
1/23
4.3
1/16
6.3
47
1/18
5.6
1/13
7.7
48
1/14
7.1
1/10
10.0
49
1/11
9.1
1/8
12.5
Historically, women over 35 years of age at term were considered “high risk” for chromosome aneuploidy and were offered invasive prenatal diagnosis via fetal karyotyping following amniocentesis or chorionic villus sampling. Age 35 was selected as the cut-off, in part, due to the often-quoted 1 in 200 risk of complications with amniocentesis; the risk of aneuploidy was felt to be approximately equal to or greater than the procedural risk. The cost-effectiveness and utility of this approach was questioned, particularly in light of the procedure-related pregnancy loss rate [23].
Second-Trimester Maternal Serum Biochemical Screening
Second-trimester biochemical maternal serum screening started with the finding that low maternal serum alpha-fetoprotein (MS-AFP) was associated with an increased risk of Down syndrome [3]. Maternal serum screening for aneuploidy then expanded to include multiple additional markers: hCG, unconjugated estriol (uE3), dimeric inhibin A (DIA), and in some laboratories, invasive trophoblast antigen (ITA) [4]. These quadruple (“Quad”) or “Penta” screens provided additional parameters by which to estimate a woman’s risk of fetal aneuploidy in a given pregnancy, with higher sensitivity than age alone (approximately 80 % for Down syndrome at a 5 % false-positive rate). The “pattern” of high or low levels (as calculated by MoM) of these analytes, combined with maternal age, weight, gestational age (ideally confirmed by ultrasound biometry), and race are used to calculate risk for fetal Down syndrome, trisomy 18, and ONTD; see Table 8.2 for a summary. In some centers, a risk for Smith–Lemli–Opitz syndrome (SLOS, an autosomal recessive condition characterized by a range of intellectual disability, growth restriction, and structural anomalies) is also calculated based on low serum estriol. Although no uniformly accepted practice exists, it has been suggested in multiple studies that unexplained extreme values of second-trimester analytes should prompt further investigation and increased maternal-fetal monitoring [24, 25].
Analyte | Trisomy 21 | Trisomy 18 | ONTD | Other risks with high levels (>2.0 MoM) | Other risks with low levels (<0.5 MoM) |
|---|---|---|---|---|---|
MS-AFP | ↓ | ↓ | ↑ | Birth defects (not limited to ONTD or OAWD), fetal death, placental abnormality, IUGR, fetal distress | Fetal death, preterm birtha |
hCG | ↑ | ↓ | – | Birth defects (not limited to trisomy 21), IUGR, fetal distressb | IUGR, birth defectsb |
uE3 | ↓ | ↓ | – | No significant risks | IUGR, fetal death; certain single-gene conditions (X-linked ichthyosis, congenital adrenal hyperplasia) |
DIA | ↑ | ↓ | – | Preeclampsia, fetal death, preterm birth, IUGR | No significant risks |
First-Trimester Maternal Serum Biochemical Screening
In an effort to perform risk assessment for aneuploidy at an earlier gestational age, first-trimester markers for aneuploidy were investigated. Previously used second-trimester markers were explored for utility in the first trimester, but only hCG was found to be informative; elevated hCG is associated with an increased risk for Down syndrome. PAPP-A, another product of the placenta, is found in low levels in maternal serum of affected pregnancies. Low levels of both analytes are concerning for trisomy 18. Taken together, these two markers had a 65 % detection rate at a 5 % false-positive rate for Down syndrome; however, second-trimester maternal serum screening had a higher detection rate. Therefore, additional markers were needed to improve first-trimester screening [5].
First-Trimester Ultrasound Markers for Chromosomal and Genetic Anomalies
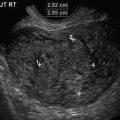
Nuchal translucency (NT), a measurement of the thickness of the subcutaneous fluid at the back of the neck of the fetus in the late first trimester, was observed to be increased in fetuses with Down syndrome. Stringent, efficacious and standardized methods for measurement of the fetal NT were developed in the early 1990s [28]. NT alone was found to have a ~75 % detection rate and ~5 % false-positive rate for Down syndrome [29]. Kagan and colleagues found that 19.2 % of pregnancies with NT >3.4 mm had an abnormal karyotype [30]. Furthermore, the incidence of chromosomal defects increased with NT thickness, from approximately 7 % with an NT of 3.4 mm (95th percentile for crown-rump length) to 75 % for an NT of ≥8.5 mm. The majority of fetuses with Down syndrome had an NT of <4.5 mm, whereas in the majority of fetuses with trisomies 13 or 18, NT measurement was 4.5 to 8.4 mm. Fetuses with Turner syndrome tended to have an NT of 8.5 mm or more (Table 8.3).
Syndrome | Incidence (% of fetuses with increased NT) | Etiology | Inheritance | Features | Testing considerations |
|---|---|---|---|---|---|
Turner syndrome (Monosomy X) | 1 in 2000 females (~6.7 %; associated with larger NTs compared to Down syndrome. Highest incidence (12.3 %) if NT is 5.5–6.5 mm [30] | Presence of a 45,X cell line | Sporadic | Prenatal: cardiac defects and cystic hygroma (resulting in a webbed neck in the postnatal period); associated high risk of IUFD Postnatal: short stature, cardiac and kidney malformations, webbed neck, lymphedema, reduced fertility, and risk for mild developmental and learning delays [35] | May be diagnosed incidental to prenatal screening or testing for fetal trisomy. Low-level mosaicism may be undetectable by standard fetal karyotype and chromosome microarray. FISHa of additional interphase cells may improve detection and identify Y chromosome material, which confers a risk of postnatal gonadoblastoma [34] |
Noonan syndrome | Mutation in genes encoding proteins in Ras/MAPK signaling pathway (most commonly PTPN11, but also SOS1, RAF1, BRAF, MAP2K1, MAP2K2, NRAS, SHOC2, CBL, HRAS, and KRAS) [38] | Autosomal dominant; de novo in 25–70 % of cases [39] | Prenatal: hydrops fetalis, cardiac anomalies; polyhydramnios, bilateral pyelectasis and ventriculomegaly have been reported [40] | Prenatal molecular genetic diagnosis on chorionic villi or amniocytes via a panel of genes is clinically available, though detection rate is only ~70 % [33] | |
Postnatal: wide variability; short stature, congenital heart defect, and developmental delay of variable degree. Other findings can include broad or webbed neck, pectus, cryptorchidism, varied coagulation defects, lymphatic dysplasias, and ocular abnormalities. Apparently asymptomatic individuals exist. Part of a spectrum of disorders (including Leopard syndrome, cardiofaciocutaneous (CFC) syndrome, and Costello syndrome) [38] | |||||
22q11.2 deletion syndrome (DiGeorge syndrome, velocardiofacial syndrome [VCFS]) | 1 in 4000 (~3 % if prenatal heart defects noted [41] | Microdeletion of chromosome 22 at band q11.2; size of deletion may vary | |||
Postnatal: conotruncal heart defects, neonatal hypocalcemia, hypothyroidism, palatal defects, immune deficiency, short stature, gastrointestinal, genitourinary and ophthalmologic disease; normal IQ to mild intellectual disability, autism spectrum disorder, increased risk for psychiatric disorders in adulthood [43] | |||||
Skeletal dysplasias | Estimated at ~1 in 2200 to 4400 live births [49] | Heterogeneous group of genetic conditions | May be autosomal dominant, autosomal recessive or X-linked; many de novo [49] | Prenatal: hydrops, short femurs, abnormal skull shape and mineralization, abnormal profile, abnormal chest. Second-trimester anatomy scan may reveal additional findings. Risk of IUFD, particularly where chest anomalies increase likelihood of pulmonary insufficiency. Some not compatible with long-term survival [49] | Given the large number of genes associated with skeletal anomalies, gene “panels” that simultaneously test multiple genes may assist in determining the correct diagnosis and the recurrence risk of the condition for future pregnancies [33, 50]. If possible, postnatal evaluation by a pediatric geneticist may be beneficial in establishing a diagnosis |
Postnatal: short stature, limb shortening; varies greatly depending on the underlying diagnosis |
While the risk of numerical chromosome anomalies can be clarified by fetal karyotype, microdeletion and microduplication syndromes have been increasingly associated with thickened fetal NT. Chromosomal microarray (CMA, also called array comparative genomic hybridization or array CGH) can interrogate fetal DNA obtained by CVS or amniocentesis and detect small (~1–3 megabases [Mb]) genome-wide deletions or duplications of DNA (copy number variations [CNVs]). This is performed by comparing fetal DNA against a reference genome via a microchip-based reaction. For additional information about this tool, the reader is referred to ACOG Committee Opinion No. 581: the use of chromosomal microarray analysis in prenatal diagnosis [52].
In a 2015 study by Lund and colleagues, in fetuses with isolated NT ≥3.5 mm, clinically significant CNVs were detected in 12.8 % of cases with normal karyotype; an additional 3.2 % had CNVs of uncertain clinical significance [53]. Clinically significant CNVs were detected in 14.3 % of fetuses with an NT of 3.5 to 4 mm, structural anomalies in other systems, and a normal karyotype; detection rate was 16.7 % in similar cases where NT measured ≥4 mm [54]. Notably, chromosomal microarray can detect 22q11.2 deletion syndrome, the CNV most commonly associated with increased NT and cardiac defects (see Table 8.3).
It should be noted that, while the clinical significance of thousands of pathologic and benign CNVs has been well documented, there remain regions of the genome for which the significance of a microduplication or microdeletion is not known. Furthermore, chromosomal microarray may incidentally detect consanguinity (including incest), non-paternity, and genetic abnormalities associated with adult-onset disorders that may be inherited from an asymptomatic parent. Therefore, it is recommended that genetic counseling with informed consent be obtained prior to performing microarray in cases with increased fetal NT [52].
In the event that fetal chromosome abnormality has been ruled out, an increased NT may be indicative of many other genetic and nongenetic conditions. Of the single gene conditions, the most common is Noonan syndrome (see Table 8.3). A link between increased NT and several other single-gene conditions and have been suggested. However, due to the rarity of most of these conditions (most have an incidence of <1 in 10,000), a definitive association between increased NT and these conditions cannot be statistically proven. Furthermore, the single-gene and often de novo molecular cause of these conditions is not amenable to comprehensive prenatal genetic diagnosis [31, 32]. As can be surmised from Table 8.3, many conditions have sonographically diagnosable fetal anomalies, in addition to an increased NT, albeit, not always in the first or early second trimesters.
In addition to nuchal translucency, evaluation of the fetal nasal bone is a benefit of first-trimester ultrasound. Hypoplastic or absent nasal bone has been associated with fetal Down syndrome. Nasal bone evaluation between 11 0/7 to 13 6/7 weeks is included in first-trimester screening for Down syndrome in some centers, as it is independent of other first-trimester markers (free β-hCG, PAPP-A, and NT). In one series, the nasal bone was absent in 2.6 % of the euploid fetuses (though this may vary with ethnicity); it was absent in 59.8 % of the fetuses with trisomy 21, 52.8 % with trisomy 18, 45.0 % with trisomy 13 and in none of the fetuses with Turner syndrome [55]. At a false-positive rate of 5 %, nasal bone evaluation in addition to NT and serum analytes was estimated to achieve a sensitivity of >95 % for trisomy 21, 18 and 13, and is not thought to significantly prolong ultrasound examination time [55, 56]. Much like nuchal translucency, rigorous guidelines have been established for measurement of this feature, which is outside the scope of this chapter (see Chap. 9).
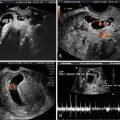
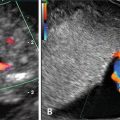
More recently, first-trimester evaluation of flow in the ductus venosus and across the tricuspid valve via Doppler has been proposed to aid in risk assessment and improve detection rate for fetal aneuploidy. In one prospective study, a ductus venosus pulsatility index for veins (DV-PIV) demonstrating a reversed a-wave was estimated to detect 96 %, 92 %, 100 %, and 100 % of trisomies 21, 18, and 13 and Turner syndrome, respectively, at a false-positive rate of 3 %, when combined with maternal age, NT, fetal heart rate, and β-hCH and PAPP-A [57]. In the same cohort of patients, assessment of tricuspid flow for regurgitation demonstrated the same detection rates for chromosomal anomalies as DV-PIV [58].
Benefits of First-Trimester Ultrasound in Detection of Non-chromosomal Fetal Anomalies
Despite increased utilization of noninvasive DNA screening (NIDS) for fetal aneuploidy, first-trimester ultrasound remains a useful screening tool for non-chromosomal conditions that may have a significant impact on prenatal and postnatal outcome. Increased NT is a risk factor for fetal congenital heart defects (CHD), although no pattern of specific CHD has been described. An NT >95th percentile for crown-rump length has been associated with a significantly increased risk for CHD in fetuses with a normal karyotype, with a detection rate for major CHD of ~44 % for a 5.5 % false-positive rate [59]. Doppler evaluation of the tricuspid valve and ductus venosus at first-trimester ultrasound can also improve the detection rate; 32.9 % of euploid fetuses with major CHD had tricuspid valve regurgitation, and 28 % had an abnormal a-wave in the ductus venosus (compared to 1.3 % and 2.1 % of those without CHD, respectively) [60]. The current consensus is that fetal echocardiogram, performed as early as the late first trimester, should be considered in pregnancies with increased NT (>3.5 mm), particularly as some studies have showed improved neonatal outcome in ductal dependent CHD after being identified via NT measurement [31, 61, 62]. Additional discussion on first-trimester detection of CHD is found in Chap. 11.
First-trimester increased NT has also been associated with fetal death, with risk appearing to directly correlate with NT measurement; overall risk is ~4 %, ranging from ~2 % at 3.5 mm to ~17 % at >6.5 mm [33, 63]. It may be an early indicator of structural anomalies, including but not limited to body stalk anomaly, diaphragmatic hernia, omphalocele, orofacial clefts, fetal akinesia sequence and megacystis. The overall incidence of structural anomaly with NT >3.5 mm is estimated at ~12 % in the presence of a normal fetal karyotype [32, 33, 63]. Fetal infection is often cited as a possible cause for increased NT. Parvovirus B19 infection is the only specific pathogen associated with increased NT, most likely secondary to myocardial dysfunction or fetal anemia [64].
In twin gestations, first-trimester markers (including NT, nasal bone, tricuspid valve flow, and DV-PIV) may be helpful in risk assessment for aneuploidy as they are independent measurements for each fetus, regardless of chorionicity; however, NT is also helpful in assessing risk of twin-to-twin transfusion syndrome for monochorionic twins [65].
Current Methods of First-Trimester Maternal Serum Aneuploidy Screening
In 2007, the American College of Obstetrics and Gynecology published a practice bulletin stating that “first-trimester screening using both nuchal translucency measurement and biochemical markers is an effective screening test for Down syndrome in the general population… Screening and invasive diagnostic testing for aneuploidy should be available to all women who present for prenatal care before 20 weeks of gestation regardless of maternal age”[4].
There are many current screening methodologies to address these recommendations, using different combinations of first-trimester ultrasound, first-trimester biochemical markers, and second-trimester biochemical markers to generate a risk assessment for aneuploidy. First-trimester analyte screening uses PAPP-A and hCG analytes; first-trimester combined screening adds nuchal translucency with or without nasal bone measurement. Similarly, integrated and serum integrated screening combine first-trimester PAPP-A measurement with second-trimester analytes, with our without first-trimester ultrasound parameters, respectively. Stepwise sequential and contingency screening allow for women defined as “high-risk” to be notified of increased risk after first-trimester screening, with the option of invasive prenatal testing; women in a “moderate-risk” category may receive second-trimester analyte screening to give an aneuploidy and ONTD risk assessment with the highest detection rate. Women identified as “low-risk” after first-trimester methods are not offered second-trimester analyte measurement in contingency screening [8].
The wide array of options may appear complicated to health care providers and patients alike; the benefits, limitations and possible scenarios for use are summarized in Table 8.4.
Screening Method | Detection rate (DR) | Procedure | Advantages | Limitations | Clinician likely to utilize test | |
|---|---|---|---|---|---|---|
Trisomy 21a (%) | Trisomy 18b (%) | |||||
First-trimester analyte screening | 62–63 | ~82 | Free beta-hCG and PAPP-A drawn at 9–13 6/7 weeks | First-trimester result, NT not required, one visit, CVS an option if screen positive | Lower DR compared to options utilizing NT; no screening for ONTD | Clinician with early-to-care population with no access to certified NT provider, but does have access to CVS, and prefers one visit for screening |
Combined first-trimester screening | 78–91 | 91–96 | Nuchal translucency ± nasal bone measurement and trimester analyte screening at ~10–13 6/7 weeks | First-trimester result, one visit, CVS an option if screen positive | NT required, lower DR compared to integrated screen; no screening for ONTD | Clinician with early-to-care population who has access to certified NT provider and CVS, and prefers one visit for screening |
Integrated screening | 94–96 | 91–96 | PAPP-A and NT measurement at ~10–14 weeks; AFP, hCG, uE3 and DIA drawn at 15–21 6/7 weeks | Highest DR of all maternal serum screening tests | Two visits and NT required; results given in second trimester | Clinician with early-to-care patient population who has access to a certified NT provider, but does not have access to CVS |
Serum integrated screening | 87–88 | ~82 | PAPP-A only at ~10–14 weeks; AFP, hCG, uE3 and DIA drawn at 15–21 6/7 weeks | Highest DR for screening when NT is not available; NT not required | Two visits, results given in second trimester, lower DR compared to screens that include NT | Clinician with early-to-care population who does not have access to certified NT provider or CVS |
Stepwise sequential screening | 91–95 | 91–96 | PAPP-A, b-hCG, and NT in first trimester; risk reported if elevated. If low risk, AFP, hCG, uE3, and DIA in second trimester | First-trimester result for highest risk patients allows option of CVS; DR higher than combined FTS while allowing for some first-trimester results | Two visits for most patients; NT required; lower DR compared to integrated screen | Clinician with early-to-care population and high follow-up compliance, with access to a certified NT provider and CVS, who wants information early enough to offer CVS if risk is high, and wants to avoid moderate risk group created by contingency screening |
Contingency screening | 91–92 | 91–96 | PAPP-A, b-hCG, and NT in first trimester; results reported; high risk offered diagnostic testing, low-risk screening complete; moderate risk group receives AFP, hCG, uE3, and DIA in second trimester | First-trimester results for high- and low-risk patients, minimizing number of patients needing a second visit | Two visits for moderate risk group; NT required; Initial moderate risk group may not feel as reassured with second trimester negative screen result as initial low-risk group; no screening for ONTD in low-risk group | Clinician with an early-to-care population and high follow-up compliance who has access to a certified NT provider and to CVS, and who feels the benefit of a one visit screen for most patients outweighs the anxiety caused for patients who fall into the moderate-risk group and are later re-stratified to a low-risk group |
Multiple marker serum screening | 75–83 | 60–70 | AFP, hCG, uE3, DIA (± ITA) drawn between 15 and 21 6/7 weeks | Allows for screening in women presenting for care after first trimester; one visit | Results given in second trimester; lower DR compared to screens involving first-trimester elements; risk of conflicting assessments if performed without knowledge of prior combined first-trimester screeningc | Clinician with patients who present primarily in the second trimester for screening or patients whose insurance does not cover NT screening. |
Noninvasive DNA screening (NIDS)d | >99 | >97 | Maternal blood sample drawn between 10 and 21 6/7 weekse | First- or second-trimester result in one visit, NT not required, highest DR | New technology with shorter publication history and less information on payer coverage | Clinician comfortable with new technology who wants a screening test with high DR and low FPR that can be applied in first and second trimesters |