Indication
Association with cardiac defects (%)
Other structural anomalies [103]
21
Increased nuchal translucency [104]
7
Tricuspid regurgitation [47]
5.1
Previous history of CHD [37]
8.7
Abnormal ductus venosus [105]
7.5
Monochorionic twins [52]
5.5 (9.3 in cases with TTS)
Aberrant right subclavian artery [75]
5.1
Assisted reproductive techniques [53]
4.3
Consanguinity [106]
4.4
What Constitutes a Normal Early Fetal Cardiac Examination?
Demonstration of normal situs, cardiac connections, atrioventricular junction, right- and left-sided symmetry and septo-aortic continuity are constituents of a normal early cardiac examination [56]. However, in order to conclude that the fetal heart appears normal, the following parameters should be evaluated.
Heart-to-Chest Ratio
Cardiac Axis
The complex process of cardiac looping during embryonic development is demonstrated by the cardiac axis being fairly midline at 8 weeks and then gradually levo-rotating by 12 weeks after which it stabilizes at the end of the first trimester [59]. Fetuses with cardiac defects might show an abnormal deviation of the cardiac axis in relation to gestational age [60]. Mc Brien et al. [59] studied the normal changes in the fetal cardiac axis between 8 and 15 weeks of gestation and reported that the cardiac axis is orientated more to the midline of the thorax in early gestation, and then rotates to the left with advancing gestation. The authors noted that the cardiac axis changed from 39° at 11 weeks to 50° at 14 weeks. Sinskovskaya et al. [60] reported a normal variation in the cardiac axis from 34.5° at 11 weeks to 56.8° at 13 + 6 weeks of gestation, and that an abnormal cardiac axis in early gestation can be associated with coarctation of the aorta, Ebstein’s anomaly, transposition of the great vessels and heterotaxy. The same group recently showed that 74.1 % of fetuses with confirmed congenital heart defects had an abnormal cardiac axis when evaluated between 11 and 14 + 6 weeks/days of gestation [61].
Cardiac Planes (Table 11.2)
Table 11.2
Visualization of fetal cardiac structures during the early ultrasound fetal cardiac examination at 11–13 + 6 weeks of gestation
10 weeks | 11 weeks | 12 weeks | 13 weeks | 13 + 6 weeks | |
|---|---|---|---|---|---|
4-chamber view | Yes | Yes | Yes | Yes | Yes |
Outflow tracts | No | No | Yes | Yes | Yes |
Aortic and ductal arch | No | No | Yes | Yes | Yes |
Superior and inferior venae cavae | No | No | Yes | Yes | Yes |
Pulmonary veins | No | No | No | Yes | Yes |
Marques Carvalho et al. [62] explored the feasibility of obtaining the 4-chamber view and outflow tracts with transvaginal ultrasound in early pregnancy. The authors obtained the three planes in 37 % of fetuses at 11 weeks of gestation, and in 85 % of fetuses at 12 weeks of gestation. At 14 weeks, the three planes were obtained in 100 % of fetuses. The required time for examination at 14 weeks did not exceed 20 min. The authors concluded that after a crown-to-rump length of 64 mm, obtaining these three cardiac planes was completely feasible.
Carvalho et al. [56] suggested that the routine examination of the fetal heart at 11–13 + 6 weeks should include the following: the visceral situs solitus, cardiac position (axis), normal and symmetric 4-chamber view, two separate atrioventricular valves, normal aortic and pulmonary outflow tracts, two great arteries of similar size, and evidence of aortic and ductal arches. The authors mentioned that septal defects cannot be completely excluded, and that evolving cardiac lesions might not be visible in early pregnancy. Krapp et al. [63] reported that during the 11–13 + 6 week scan, the 4-chamber view could be visualized in 96 % of fetuses, the left ventricular outflow tract in 97 %, the 3-vessel view in 98 %, and the aortic arch in 72 % of fetuses, whereas the pulmonary veins were observed in 23 % of cases. Yagel et al. [64] proposed the following planes for fetal heart examination: upper abdomen, 4-chamber view, 5-chamber view, bifurcation of the pulmonary artery, 3-vessel and trachea, and the short axis of the right ventricle. The transvaginal route was suggested to be better than transabdominal ultrasound for detailed examination of the fetal heart. The authors reported that all proposed cardiac planes were obtained in 98 % of fetuses at 11–12 weeks, and in 100 % of fetuses at 13–15 weeks of gestation. They reported a 64 % detection rate for CHD when the cardiac examination was performed before 15 weeks of gestation and an extra 17 % detection when the heart was reevaluated at 20–24 weeks, with an overall detection rate of 85 % for CHD. Khalil et al. [65] proposed the following steps for cardiac evaluation in early pregnancy: assessment of the fetal position, orientation of the fetal heart, visualization of the 4-chamber view, assessment of the tricuspid valve and tricuspid regurgitation, visualization of the outflow tracts, and identification of the aortic and pulmonary arches. Abu-Rustum et al. [24] reported the following success rate for visualization of the cardiac structures during an early fetal cardiac scan: 4-chamber view (100 %), presence/absence of tricuspid regurgitation (100 %), crossing of the great vessels (90 %), bifurcation of the pulmonary artery (81 %), 3-vessel view (55 %), aortic arch (76 %), superior and inferior venae cavae (65 %), and ductus venosus (99 %). They also suggested that operators should perform a minimum of 70 fetal heart examinations at 11–13 + 6 weeks to gain reliable experience for obtaining the proposed anatomical planes with an allocated time of up to 10 min for fetal cardiac evaluation.
Operator Experience and Route of Ultrasound Examination
Allan [66] suggested that experience and technological resources are the main factors associated with differences in the detection rate of CHD, when transvaginal and transabdominal ultrasound examinations are compared. She suggested that the success of transabdominal examination can be attributed to the participation of a pediatric cardiologist in the scanning process, whereas transvaginal studies are mainly performed by obstetricians with limited experience in cardiac scanning. She concluded that it is not enough to only obtain the cardiac planes, but to also have the proper knowledge to interpret the images; and that another important factor for improving the detection of cardiac anomalies is the development of technical skills to improve the scanning plane, either by adjusting the position of the US probe or by changing the position of the mother [66]. Tegnander et al. [67] evaluated the detection of fetal cardiac anomalies by comparing operators with different levels of experience. Sonographers with previous experience of more than 2000 examinations had a 52 % detection rate of CHD as compared with a 32.5 % detection rate of operators previously performing fewer than 2000 cardiac examinations. This difference remained unchanged between the two groups of sonographers when detection of isolated CHD, or CHD with associated anomalies was analyzed. The authors concluded that it is necessary to become proficient in the visualization and interpretation of the 4-chamber view and of the left and right ventricular outflows before obtaining other anatomical cardiac planes. They suggested that, despite using a state-of-the art ultrasound system and/or the combination of different ultrasound techniques, operator experience still remains the key factor in improving the detection rate of CHD.
Well-trained operators can achieve a good detection rate of CHD early in pregnancy. Hartge et al. [68] studied a group of 3521 pregnant women presenting with 77 (2.1 %) fetuses with CHD. The ultrasound scans were performed by highly trained operators, using state-of-the art ultrasound systems with high frequency transvaginal probes. They reported 85.7 % detection rate of cardiac anomalies at 11–13 + 6 weeks of gestation. The authors mentioned that, in 64.2 % of cases, only the transabdominal route for ultrasound evaluation was needed and, in the remaining 35.8 % of patients, both transabdominal and transvaginal routes were used. The authors reported that conditions such as coarctation of the aorta, hypoplastic left heart resulting from aortic stenosis, and Tetralogy of Fallot might not be identified early in pregnancy. They concluded that well trained operators and high technology US systems are necessary to achieve a high detection rate of CHD in early pregnancy.
Rasiah et al. [69] performed a systematic review of the diagnostic performance of fetal echocardiography in the first trimester of pregnancy. They identified ten studies done in tertiary centers with good quality control that met the inclusion criteria. They reported a combined sensitivity of 85 % (95 % CI, 78–90 %) and specificity of 99 % (95 % CI, 98–100 %), positive likelihood ratio (LR) of 59.6 (95 % CI, 26.5–133.6), and negative LR of 0.25 (95 % CI, 0.1–0.6) for identification of congenital heart defects. The authors mentioned that, although transvaginal ultrasound is thought to be a better modality for visualization of the fetal heart, the training and experience of the operators and high quality US systems can lead to similar detection rates using transabdominal ultrasound.
When Is the Optimal Time to Perform Early Fetal Cardiac Evaluation?
Carvalho et al. [56] suggested, aside from operator experience, gestational age at examination is an important factor associated with a successful evaluation of the fetal heart. Haak et al. [70] reported that at 11 weeks successful evaluation of the heart can be achieved in about 20 % of fetuses, whereas at 13 weeks of gestation the success rate for fetal cardiac evaluation increases to 92 %.
Smrcek et al. [71] studied fetuses from 10 to 15 weeks of gestation to evaluate the following cardiac planes: 4-chamber view, 3-vessel view, origin and crossing of the great arteries, aortic and ductal arches, superior and inferior venae cavae, and at least two pulmonary veins. They were able to identify all structures at 10 weeks of gestation, except for the superior and inferior vena cava, which were visualized at 11 weeks. The pulmonary veins were observed in 80 % of fetuses between 12 and 14 weeks, and in 100 % of fetuses at 15 weeks of gestation. The authors reported an increment in the detection rate of cardiac defects, from 67 % at 10 weeks to 100 % at 15 weeks of gestation. They mentioned that, between 10 and 13 weeks, the transvaginal route for ultrasound examination was better than the transabdominal route; that, between 12 and 14 weeks of gestation, both transabdominal and transvaginal ultrasound had a similar detection rate; and from 15 weeks of gestation onward, the transabdominal route was better. The authors mentioned that complementary use of color directional Doppler and power Doppler, and not limiting the scanning time, can improve the optimal visualization of the fetal heart.
Vimpelli et al. [72] evaluated the feasibility of performing the cardiac examination at different weeks during the first trimester of pregnancy. The authors aimed to obtain the following planes: 4-chamber, longitudinal views of the aorta and pulmonary trunks, crossing of the great arteries, and aortic and ductal arches. The authors reported that visualization of all structures varied from 43 % at 11 weeks to 62 % at 13 + 6 weeks. The 4-chamber view was obtained in 74 % of cases at 13 + 6 weeks. McAuliffe et al. [73] evaluated a high-risk group of 160 women, defined by previous history of congenital heart disease, increased nuchal translucency, or the presence of a non-cardiac malformation during the nuchal scan. The authors evaluated the following cardiac parameters: 4-chamber view, symmetry of the cardiac chambers, atrioventricular valves, outflow tracts, crossing of the great arteries, and, when possible, the ductal and aortic arches. The mean gestational age at examination was 13.5 weeks, and the prevalence of cardiac defects was 12.5 % (n = 20). The 4-chamber view was seen in 100 % of fetuses, the tricuspid and mitral valves in 96 %, the outflow tracts in 95 %, the aortic and ductal arches in 45 %, and the pulmonary veins in 16 %. From 20 fetuses with CHD, 14 (70 %) were identified during the first trimester scan; the authors reported a specificity of 98 %, a positive predictive value (PPV) of 87.5 % and a negative predictive value (NPV) of 96 %.
Indirect Markers for Early Fetal Cardiac Evaluation
Borrell et al. [43] analyzed the contribution of increased nuchal translucency, tricuspid regurgitation, and reversed A wave in the ductus venosus in the identification of fetal cardiac defects in chromosomally normal fetuses. They reported that, among fetuses identified at 11–14 weeks with congenital heart disease, 40 % also had increased nuchal translucency, and 39 % had reversed A wave in the ductus venosus.
Clur et al. [74] reported that increased nuchal translucency, abnormal ductus venosus, and tricuspid regurgitation were the most frequent extra-cardiac ultrasound findings related with congenital heart disease. They showed that fetuses with normal chromosomes, but with increased nuchal translucency and reversed A wave in the ductus venosus, had an 83 % prevalence of cardiac defects. The authors also proposed that analysis of the pulsatility index of the ductus venosus, instead of presence/absence of atrial flow, might increase to 70 % the detection rate of fetal cardiac anomalies.
Pereira et al. [47] studied 85 euploid fetuses with major congenital heart defects and found an increased nuchal translucency (>95th percentile) in 35.3 %, tricuspid regurgitation in 32.9 %, and reversed A wave in the ductus venosus in 28.2 % of fetuses during first trimester ultrasound screening. In fact, any one of these markers was identified in 57.6 % of fetuses with cardiac defects and in 8 % of structurally normal fetuses. They concluded that these three markers improved the performance of screening for congenital heart defects in the first trimester.
Rembouskos et al. [75] suggested an association between aberrant right subclavian artery (ARSA) and fetal cardiac defects. The authors studied 4566 fetuses and identified 89 fetuses with ARSA, of which 12 fetuses had a chromosomal anomaly. The prevalence of fetal cardiac defects in chromosomally normal fetuses with ARSA was 4/77 (5.1 %), including Tetralogy of Fallot (n = 1), aberrant umbilical vein (n = 1) and tricuspid atresia (n = 2). The authors suggested that early fetal echocardiography is indicated in the presence of ARSA.
Sinkovskaya et al. [60, 61] evaluated the performance of cardiac axis measurement in early gestation for detection of major fetal cardiac defects. They examined the cardiac axis between 11 and 14 + 6 weeks in fetuses with confirmed congenital heart defects across three tertiary centers. They documented an extreme left or right deviation of the cardiac axis in 74.1 % of fetuses with congenital heart defects. In their study the cardiac axis performed better than enlarged nuchal translucency, tricuspid regurgitation, or reversed A wave in the ductus venosus, alone or combined, in detecting major fetal cardiac defects.
Clinical Application: Imaging the Fetal Heart in Early Pregnancy, Practical Recommendations
It is necessary for the operator to adjust the settings of the ultrasound system prior to a fetal cardiac examination. Even though this is an individual process, some basic principles might contribute to improved image quality.
Frequency and Depth
High-frequency transducers are a better option if the fetal heart is located close to the ultrasound probe. Transvaginal high-frequency ultrasound probes emitting at 9–12 MHz might be preferable at 11–12 weeks of gestation when the fetus is located close to the probe, whereas probes emitting at 5–9 MHz might be preferred at 12–13 weeks of gestation when the fetus is located away from the transducer. Transabdominal examination might be better with a linear 9-MHz probe if the fetus is located close to the maternal abdominal wall; if not, a 2- to 5- or 4- to 6-MHz probe might provide better ultrasound images. During B-mode, system settings should be optimized to obtain images with a high frame rate, increased contrast and high resolution along with the use of low persistence, a single acoustic focal zone and a relatively narrow image field. Depth adjustment and magnification should be employed when possible. Harmonic imaging can also be used to improve image quality and particularly for patients with increased maternal abdominal wall thickness.
Identification of the Scanning Planes
Transvaginal ultrasound might provide adequate images when performed between 11 and 12 weeks of gestation and when the fetus is in an optimal position. In some cases the required planes might not be immediately acquired, as the possibility of modifying the position of the uterus and the fetus and manipulating the ultrasound probe is limited. A prolonged transvaginal examination might be uncomfortable. In patients with increased body mass index, or with previous cesarean section or abdominal surgery, the transvaginal route for fetal cardiac examination should be preferred. Transabdominal examination from 13 weeks onwards offers the possibility to freely manipulate the ultrasound probe, and to change the position of the patient and of the scanning bed to acquire the fetal cardiac planes. The scanning time can also be prolonged.
A cross sectional plane of the fetal thorax with the heart in an apical projection and the fetal spine in the lower part of the ultrasound screen is the optimal image for cardiac examination. The 4-chamber view, 5-chamber view, crossing of the big arteries, and 3-vessel view can be obtained from this projection by performing a slow sweep towards the fetal head and maintaining cross sectional images of the studied planes (Fig. 11.1). The two outflow tracts can be visualized by rotating the ultrasound probe clockwise or anticlockwise from the 4-chamber view (Fig. 11.2). By rotating the probe 90° from the 4-chamber view, a sagittal plane of the thorax is obtained, and by gently moving the ultrasound probe from side to side, the aortic and ductal arches, and inferior and superior vena cava can be observed (Fig. 11.3). Color directional Doppler might be helpful in assessing the integrity of the interventricular septum, to visualize the crossing of the great arteries, and to document the direction of flow in the aortic arch (Fig. 11.4). Spectral Doppler is probably not necessary at this stage unless evaluation of the fetal cardiac function is necessary.





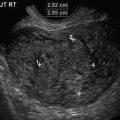
Fig. 11.1
Cross-sectional image of the fetal heart at the level of the 4-chamber view at 13 + 5 weeks /days of gestation. (a) 4-chamber view. (b) Highlighted anatomical structures: LA left atrium, LV left ventricle, RA right atrium, RV right ventricle. Note the pulmonary veins reaching the left atrium. (c) Heart-to-thorax ratio. (d) Cardiac axis

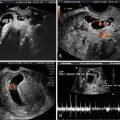
Fig. 11.2
Outflow tracts and 3-vessel view. (a) Left outflow tract and aorta (LA left atrium, RV right ventricle). (b) Right outflow tract and pulmonary valve obtained from a short axis. (c) 3-vessel view. (d) Slightly oblique plane from the 3-vessel view to obtain the pulmonary valve

Fig. 11.3
Sagittal images. (a) Aortic arch and descending aorta. (b) Pulmonary artery and ductal arch (RV right ventricle). (c) Ductal arch and descending aorta. (d) Inferior and superior venae cavae

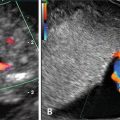
Fig. 11.4
High-definition color directional Doppler. (a) Cross-sectional view of the fetal heart and interventricular septum (LA left atrium, LV left ventricle, RA right atrium, RV right ventricle). (b) Joint of the aorta and pulmonary artery with blood flow moving in the same direction. (c) Ductal arch and descending aorta. (d) Inferior and superior venae cavae
Clinical Application: Detection of Cardiac Anomalies
There is a great variation in the detection rate of congenital heart disease due to non-modifiable factors, such as: the prevalence of the disease, the presence of high-risk ultrasound markers, the type of CHD and some modifiable factors, such as: the population screened, gestational age selected at scanning, operator experience and ultrasound system and techniques used (Table 11.3).
Table 11.3
Studies on the diagnostic capacity of early ultrasound for the identification of congenital heart disease
Study | Total (n) | Scan route | GA (weeks) | Prevalence of CHD (n [%]) | Early detection (n [%]) |
|---|---|---|---|---|---|
Hernadi and Torocsik [107] | 3991 | TA, TV | 11–14 | 1 (0.02) | – |
D’Ottavio et al. [108] | 4078 | TV | 13–14 | 12 (0.29) | 3 (25.0) |
Bilardo et al. [109] | 1690 | TA | 10–14 | 4 (0.23) | – |
Hafner et al. [110] | 4233 | TA | 10–14 | 14 (0.33) | 1 (7.1) |
Hyett et al. [41] | 29,154 | TA | 10–14 | 43 (0.15) | 1 (2.3) |
Schwarzler et al. [111] | 4523 | TA | 10–14 | 9 (0.20) | – |
Mavrides et al. [112] | 7339 | TA | 10–14 | 24 (0.33) | 4 (16.7) |
Michailidis and Economides [113] | 6650 | TA, TV | 10–14 | 9 (0.14) | 2 (22.2) |
Orvos et al. [114] | 4309 | TV | 10–13 | 32 (0.74) | – |
Taipale et al. [115] | 4789 | TV | 10–16 | 18 (0.38) | 1 (5.6) |
Chen et al. [116] | 1609 | TA, TV | 12–14 | 7 (0.44) | 4 (57.1) |
Bahado Singh et al. [42] | 8167 | TA | 10–14 | 6 (0.07) | – |
Bruns et al. [117] | 3664 | ? | 11–14 | 9 (0.25) | – |
Becker and Wegner [29] | 3094 | TA, TV | 11–14 | 11 (0.36) | 6 (54.5)a |
Cedergren and Selbing [118] | 2708 | TA | 11–14 | 3 (0.11) | – |
Dane et al. [119] | 1290 | TA | 11–14 | 1 (0.08) | – |
Westin et al. [81] | 16,260 | TA | 12–14 | 29 (0.18) | – |
Muller et al. [120] | 4144 | TA | 10–14 | 13 (0.31) | – |
Chen et al. [121] | 7642 | TA | 10–14 | 19 (0.25) | 7 (36.8) |
Oztekin et al. [122] | 1805 | TA | 11–14 | 2 (0.11) | – |
Hildebrand et al. [79] | 21,189 | ? | 11–14 | 62 (0.29) | 0 |
Syngelaki et al. [80] | 44,859 | TA, TV | 11–13 | 106 (0.24) | 36 (34) |
Volpe et al. [76] | 4445 | TA, TV | 11–14 | 28 (0.63) | 23 (82.1) |
Grande et al. [123] | 13,723 | TA, TV | 11-14 | 44 (0.32) | 25 (56.8) |
Hartge et al. [68] | 3521 | TA, TV | 11–13 + 6 | 77 (2.1) | 66 (85.7) |
Iliescu et al. [77] | 5472 | TA, TV | 12–13 + 6 | 30 (0.54) | 27 (90) |
Persico et al. [83] | 886 | TA | 11–13 | 100 (11.2) | 96 (96) |
Eleftheriades et al. [82] | 3774 | TA | 11–13 + 6 | 29 (0.77) | 13 (44.8) |
Volpe et al. [100] | 870 | TA | 11–14 | 62 (0.17) | 56 (90.3) |
Rossi et al. [78] (systematic review) | 78,002 | TA, TV | 11–14 | 418 (0.53) | 118/224b (53) |
Low-Risk Population
Volpe 2011 et al. [76] studied 4445 low risk fetuses with a 0.9 % prevalence of cardiac defects (n = 42), 28 major and 14 minor. A total of 39 cases were identified prenatally, 29 (69 %) during the first-trimester scan and 10 (23.8 %) in later stages of pregnancy. The authors mentioned that increased nuchal translucency, tricuspid regurgitation and reversed A wave in the ductus venosus were associated with a higher prevalence of fetal cardiac defects. The presence of these ultrasound markers should be considered an indication for targeted fetal cardiac evaluation. The authors reported that an abnormal 4-chamber view had a 50 % detection rate for major cardiac defects (Figs. 11.5 and 11.6).



Fig. 11.5
Abnormal 4-chamber view; dilatation of the right atrium due to tricuspid insufficiency

Fig. 11.6
Abnormal 4-chamber view; atrioventricular septal canal (power Doppler ultrasound)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree