Fig. 10.1
Early gestational sac with hCG = 420 mIU/mL
Discriminatory Value
The discriminatory value is that level of hCG above which all normal intrauterine pregnancies should be seen. An early study, using transabdominal ultrasound, advocated a level of 6500 mIU/mL [2]. Clearly, the introduction of transvaginal sonography revolutionized early pregnancy assessment. In 1987, relatively early in the use of TVS, Nyberg et al. reported that the discriminatory level was 1800 mIU/mL (Third International Standard) [3]. As equipment improved the general consensus was that the discriminatory level was between 1000 and 1500 mIU/mL in most centers. This level has become progressively more important with the increased adoption of medical management of ectopic pregnancy. Unfortunately, there are rising numbers of early IUPs being treated with methotrexate, being erroneously diagnosed as an ectopic pregnancy, based on the lack of an intrauterine gestational sac when the hCG is above the discriminatory value. This clearly has both medical and legal implications [4]. The reliance on the previous discriminatory values was contested in a paper by Doubilet and Benson in 2011 [5]. This retrospective review assessed the hCG level in 202 patients evaluated over 10 years, who had a TVS and β-hCG on the same day, had no visualized intrauterine fluid collection on their initial study, but were subsequently found to have an intrauterine pregnancy, with embryonic fetal cardiac activity. They found that 10.4 % of such pregnancies had an hCG > 1500 mIU/mL, with 4.5 % having an hCG above 2000 mIU/mL (Fig. 10.2). This challenged the medical community to reevaluate our current hCG discriminatory level. Connolly et al., in 2013, reported on 651 patients with known intrauterine pregnancies who had a TVS and β-hCG within 6 h of each other. They evaluated the initial ultrasound findings which were visualized 99 % of the time, in correlation with the hCG level (Table 10.1). They determined that the discriminatory value was 3510 mIU/mL, much higher than previously advocated. It is estimated that women with an hCG above 2000 mIU/ML and no visualized gestational sac are more likely to have a nonviable intrauterine pregnancy (65 %) than an ectopic pregnancy (33 %), with the remainder (2 %) being viable intrauterine pregnancies. Thus, in a patient with a pregnancy of unknown location [6], with an hCG level over 2000 mIU/mL and who is hemodynamically stable, observation and follow-up are recommended until the clinical diagnosis is clarified (Fig. 10.3) [7, 8].



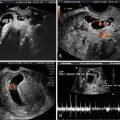
Fig. 10.2
Gestational sac finally visualized when the hCG = 1570 mIU/mL
hCG (mIU/mL) | Gestational sac | Yolk sac | Embryo |
|---|---|---|---|
Threshold value | 390 | 1094 | 1394 |
Discriminatory value | 3510 | 17,716 | 47,685 |

Fig. 10.3
Pregnancy of unknown location with hCG = 3810 mIU/mL. Patient ultimately had IUP with twin gestation
The “New Rules” Regarding Early Pregnancy Failure
Several developmental milestones are observed in normal intrauterine pregnancy, including an intrauterine sac at 5 weeks; a yolk sac at 5.5 weeks, and an embryonic pole and fetal heart activity at 6–6.5 weeks of gestation [9, 10]. Early pregnancy failure was felt to be present when these milestones were not met. However, there is significant interobserver and intraobserver variability (±18.78 %) in measuring the mean sac diameter, and the crown-rump length [11]. As a result, there are recognized limitations of our current definitions of a nonviable pregnancy based on ultrasound evaluation [12]. Abdallah et al. evaluated 1060 women with a diagnosis of an intrauterine pregnancy of unknown viability, of which 473 (44.6 %) remained viable and (55.4 %) nonviable by the 11- to 14-week scan. There was a 4.4 % false-positive rate for a nonviable pregnancy using the traditional cutoff for mean sac diameter (MSD) of 16 mm. This rate dropped to 0.5 % using 20 mm, with no false positives when a MSD of ≥21 mm was used. Considering the inherent variability identified, these authors recommended a cutoff for MSD ≥ 25 mm, a level where no false positives would be encountered (Fig. 10.4). The lack of fetal cardiac activity with a crown-rump length (CRL) = 4 or 5 mm had a false-positive rate of 8.3 %. There were no false-positive results using a CRL cutoff of 5.3 mm. However, considering the identified variability, they recommended using a CRL ≥ 7 mm as the cutoff for determining a nonviable pregnancy (Fig. 10.5). It was recommended that observation with a repeat ultrasound in ~7 days was appropriate in hemodynamically stable patients who did not warrant the more stringent cutoffs identified by their study.