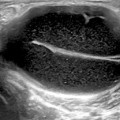
Fig. 4.1
a Picture of ankle depicting the distinct areas of synovio-entheseal complex. b Enthesis organ, composed of the ligament insertion points into bone, the adjacent synovium and bursa as well as the underlying bone, detected by ultrasound (US) examination in b mode combined with power Doppler in ankylosing spondylitis patient. Abnormal vascularization associated with marked swelling and decreased echogenicity of the enthesis at the cortical junction can be seen, as well as erosion of the calcaneus bone. Tendon thickness at the level of the enthesis is 7.2 mm and is associated with a retro-calcaneal bursa with enhanced vascularity
However, there is a difference between “enthesopathy” and “enthesitis.” The Outcome Measures in Rheumatology (OMERACT) ultrasound group suggested a definition of enthesopathy: “An abnormal hypoechoic region with loss of normal fibrillar architecture and/or thickened tendon or ligament in its bony attachment, seen in 2 perpendicular planes that may exhibit Doppler signal and/or bony changes including enthesophytes, erosions or irregularity.” This definition merged both acute and chronic inflammatory manifestations with structural damage findings [15]. Therefore, the association of enthesis in any pathologic process whether traumatic, inflammatory, metabolic, or degenerative is denoted “enthesopathy,” whereas “enthesitis” is confined to the occurrence of tendon/ligament or capsule inflammation at its insertion site into the bone [16]. The latter is the classical feature of spondyloarthritis (Fig. 4.2).
Fig. 4.2
a Picture of a flexor tendon clarifying the role synovio-entheseal complex in the pathogenesis of enthesitis. Dots show sites of inflammation—enthesis. b Grayscale US of a finger showing enhanced vascularity at the synovio-entheseal complex. US ultrasound
Generally, inflammation may occur at any enthesis site. Mechanical factors, together with physiological and anatomical characteristics of the enthesis, have been proposed as contributing factors which may impact the localization of enthesitis. This might explain the finding that most of the clinically relevant enthesitis sites are present in the lower limbs; particularly heel enthesis (Achilles enthesitis) which is the main form of enthesitis included in the Assessment of SpondyloArthritis (ASAS) international society criteria [1]. Planter fasciitis is another frequently involved site [17, 18].
Sonographic Pattern of Enthesitis
A large number of research studies have applied US to the assessment of enthesitis in spondyloarthritis . The commonest entheseal sites to be ultrasonographically examined in standard clinical practice include: Achilles tendon and plantar fascia insertions to the calcaneus, tibialis anterior tendon insertion, greater trochanter, pubis, patella (at insertions of the quadriceps femoris and patellar tendons), medial, and lateral epicondyles. Sonographically, enthesitis appear as loss of normal fibrillar pattern, increased fusiform thickness (Fig. 4.3), peri-tendinous fluid, a linear intra-substance tear, calcific deposits (Fig. 4.4), or intralesional focal changes at the tendon insertion. In addition, periosteal changes such as erosions or new bone formation may also be seen at the tendon insertion. Enlarged bursa is usually considered as a sonographic manifestation of bursitis. Enhanced vascularity assessed by power Doppler (PD) at the involved entheses may also add further information about the activity status at the assessed site as reflected by its degree of vascularity (Fig. 4.5). Table 4.1 summarizes the different sonographic patterns of enthesitis .
Fig. 4.3
Sonographic B-mode image of Achilles tendinitis showing increased fusiform thickness of the tendon with enhanced vascularity
Fig. 4.4
a Sonographic B-mode image showing calcification of the patellar tendon. b Sonographic B-mode image showing calcification of the Achilles tendon
Fig. 4.5
Sonographic B-mode image with power Doppler of the elbow showing tenosynovitis of the common extensor origin with enhanced vascularity
Table 4.1
Sonographic patterns of enthesitis
Lesion | Sonographic pattern |
|---|---|
Loss of the fibrillar pattern | The tendon displays heterogeneous echogenicity |
Tendon thickening | The thickness of the affected tendon is greater than that of the contralateral tendon |
Intrasubstance tears | A hypoechoic band within the substance of the tendon associated with discontinuity of the tendon fibers |
Intratendinous calcifications | Internal foci of high-density echoes with posterior shadowing |
Peritendinous fluid | Anechoic fluid is observed along the superficial aspect of the tendon |
Bursitis | Enlarged bursa |
Tips for US Assessment of Enthesitis
Curvilinear transducer is recommended as it can cover a wider cross section of the scanned area as compared to linear transducers.
Always assess in two perpendicular planes.
In B mode, search for the following abnormal findings at the tendon insertion, and any one of them is considered to be a feature of enthesitis: thickening or intratendinous focal changes of the tendon, calcific deposits, or periosteal changes.
An enlarged bursa is considered to be an evidence of bursitis
Enhanced vascularity evaluated by PD should be assessed at these sites: cortical bone insertion, body of tendon, bursa, and the junction between tendon and enthesis. The detection of vascularization at one of these sites is considered abnormal,
US enthesitis can be stratified according to different combinations of abnormal grayscale US and/or PD feature.
Enthesitis Scoring Tools
In a trial to standardize the quantitative assessment of enthesitis, numerous scoring tools have been developed . One of the most commonly used is the Glasgow Ultrasound Enthesitis Scoring System (GUESS) [19]. The GUESS was developed based on a study of 35 patients with spondyloarthritis (including seven psoriatic arthritis patients) who underwent independent clinical and ultrasonographic examination of both lower limbs at five entheseal sites: superior pole and inferior pole of patella, tibial tuberosity, Achilles tendon, and plantar aponeurosis. A total of 18 features, each given a score of 1, were scored on each lower limb, the maximum score being 36. The intraobserver k value for analysis of all sites was 0.9.
In another work, D’Agostino et al. [20] implemented a five-stage classification system of ultrasonography enthesitis according to B-mode and PD findings (Table 4.2) where stage 1: vascularization at the cortical junction without abnormal findings in B mode. This represents isolated vascular changes occurring during the initial phase of enthesitis; stage 2a: vascularization associated with swelling and/or decreased echogenicity at the cortical junction in B mode; stage 3a: same as stage 2a, plus erosions of cortical bone and/or calcification of enthesis, and optional surrounding bursitis. Stages 2a and 3a reflect increased vascular alterations associated with graded signs of morphologic alterations. Stage 2b: abnormal findings in B mode as in stage 2a, but without vascularization and stage 3b: abnormal findings in B mode as in stage 3a, but without vascularization. Stages 2b and 3b, which are devoid of vascularization, are suggestive of inactive lesions.
Stage | Description |
|---|---|
1 | Vascularization at the cortical junction without abnormal findings in B mode |
2a | Vascularization associated with swelling and/or decreased echogenicity at the cortical junction in B mode |
3a | Same as stage 2a, plus erosions of cortical bone and/or calcification of enthesis, and optional surrounding bursitis |
2b | Abnormal findings in B mode as in stage 2a, but without vascularization |
3b | Abnormal findings in B mode as in stage 3a, but without vascularization |
Two other scoring systems developed at the patients’ level were published. The Spanish Enthesitis Index (SEI) [21] entails, after giving the patient information about variable enthesis sites, the evaluation of global patient inflammatory activity or enthesis structural damage. The scoring system, however, used grayscale abnormalities only and did not differentiate between involvement of body of the tendon, enthesis, and bursa . The Madrid Sonographic Enthesitis Index (MASEI) [22] combined abnormalities detected by grayscale US and enhanced vascularity as assessed by PD (including bursal involvement). This scoring system was the first to evaluate enthesis in both lower limbs and upper limbs (the attachment of the triceps tendon to the olecranon). Also, the MASEI included assessment of bone erosions, enthesophytes, as well as PD signal .
Critical analysis of the four systems revealed that, although they all included assessment of enthesitis sites for both inflammatory and structural manifestations using grayscale US with or without PD, sensitivity to change was low making none of them a sensitive tool for monitoring the patient’s enthsitis activity status. Furthermore, there is inconsistency among the four scoring tools. While the GUESS and D’Agostino scoring systems were set up to grade enthesis affection (enthesitis level). The MASEI and the SEI were established as enthesitis indices at the patients’ level. Therefore, these scoring systems are uncomparable. Currently, there is an unmet need to agree on a system for use in research trials as well as standard clinical practice [23, 24] .
Subclinical Versus Clinical Enthesitis
The value of US in the diagnosis of enthesitis is that it has been reported to be more sensitive than clinical examination in identify enthesitis, raising the query whether the presence of enthesitis could be missed during standard clinical assessment . A study was carried out in 2002 [25] comparing the detection of enthesitis based on clinical examination versus US. A total of 35 patients (27 AS patients, 7 psoriatic arthritis patient, and 1 patient with reactive arthritis) had their enthesitis clinically assessed in the lower limbs as well as using US and scored according to the GUESS. The study reported significantly higher enthesitis score in the US-assessed group in comparison to clinical assessment. It concluded that US is a good method to assess for enthesitis in spondyloarthritis patients. These findings were confirmed in another study carried out by by Spadaro et al. [23]. A total of 36 AS patients had both clinical and PD ultrasonography assessment of 432 enthesis sites, and 14.8 % were diagnosed to have clinical enthesitis in comparison to 44.4 % were considered abnormal on PD ultrasonography. A third study assessed enthesitis in the feet of 44 subjects with spondyloarthritis (19 AS patients, 5 with psoriatic arthritis, 8 with reactive arthritis, and 12 with undifferentiated spondyloarthritis) [26]. Pathological findings were reported in 25 patients, most of who did not have any foot problem or a complaint. Similarly, upper limb enthesitis was assessed in another study [27]. US was used to assess for enthesitis at the proximal insertion of the deltoid, which mimics clinically impingement syndrome, in 100 symptomatic consecutive spondyloarthritis outpatients, compared to 4 groups of control patients: 100 with rheumatoid arthritis, 100 with osteoarthritis, 100 with painful shoulder, and 50 with shoulders undamaged by local pathological processes. Results revealed the frequency of enthesitis in the course of spondyloarthritis was 9 %. The prognostic value of this subclinical enthesitis was assessed in a recent study [28] carried out to identify predictors of structural joint damage in patients with early spondyloarthritis. Results revealed an increased probability for structural progression in the presence of US verified enthesitis .
Differential Diagnosis of Enthesitis
US plays also an important role in the differential diagnosis of enthesitis, in particular differentiating mechanical or metabolic enthesopathy from inflammatory enthesitis . Beside spondyloarthritis patients, enthesitis have been reported among athletes as a consequence of traumatic injuries. Distinguishing fibromyalgia tender points from enthesitis is another important challenge to be considered. However, in such cases, enthesitis is not associated with intra-articular inflammation (i.e., synovitis). Furthermore, PD technology has allowed the visualization of abnormal vascularity and soft tissue hyperemia in inflammatory conditions [28]. Therefore, that abnormal enhanced vascularity, detected by PD US, at the insertion of tendons, ligaments, fascia, and capsules into the bone is considered as a primary lesion which is seen exclusively in spondyloarthritis patients and may underlie all spondyloarthritis skeletal manifestations [20]. On the other hand, enthesophytosis cannot be considered an explicit manifestation for spondylarthritis-related enthesitis, as it has also been reported in mechanical, osteoarthritic as well as in normal asymptomatic subjects [29




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree