Fig. 5.1
Distribution and frequency of the entheseal lesions detected by ultrasound in patients with spondyloarthritis. Total acute lesions and total chronic lesions are represented in black bars, and each of the categories in gray; data are expressed in percentages with regard to all pathological lesions observed. (From [22])
Fig. 5.2
a Achilles tendon enthesitis in a patient diagnosed of psoriatic arthritis. There are thickening and hypoechogenicity of the Achilles tendon (black arrows). In power Doppler ultrasound mode, an increased blood flow can be observed (long axis). b, c Retro-calcaneal bursitis in a patient diagnosed of psoriatic arthritis with Achilles tendon enthesitis. US image reveals hypoechoic swelling of the retro-calcaneal bursa deep to the distal Achilles tendon (white arrows). The peri-bursal area appears hyper-vascular at color Doppler imaging. b Long axis. c Short axis
Clinically, enthesitis in PsA patients may be asymptomatic or can cause local pain which may vary in severity though tend to be more common and intense in the lower limbs. Common sites include enthesitis of the Achilles tendon and plantar fascia at their insertion into the calcaneus bone, which is exacerbated by weight bearing after a period of rest [13, 24] (Table 5.1). However, enthesitis may affect any of the body entheses as reported in the study carried out by Falsety et al. who detected enthesitis at the proximal insertion of the deltoid tendon in up to 17 % of PsA patients causing symptoms very similar to those of impingement syndrome [25] .
Table 5.1
Frequency of ultrasound and Dopplerdetected enthesitis at different sites in patients with psoriatic arthritis. (According to D’Agostino et al. [24])
Enthesitic sites | Frequency of US findings (grayscale and Doppler) in % |
|---|---|
Achilles tendon | 76 |
Plantar fascia | 57 |
Patellar tendon | 60 |
Quadriceps tendon | 26 |
Great trochanter | 43 |
Lateral epicondyle | 19 |
Medial epicondyle | 17 |
MSUS has been demonstrated to be more sensitive in comparison to clinical examination for the detection of enthesitis. Earlier studies revealed that US was able to identify subclinical enthesitis significantly higher than clinical assessment [21, 26]. In a cohort of 162 patients diagnosed with psoriasis sine PsA compared to 60 age/sex-matched controls, another multicenter study group demonstrated a high prevalence of subclinical synovitis (3.2 vs. 1.3 %) and enthesitis (11.6 vs. 5.3 %) on US examination [27]. In another study of Gutierrez et al., enthesitis was observed in 32.9 % and 0.9 % of enthesitis sites on grayscale and PD modes, respectively, in patients with psoriasis compared to 8.4and 0 % in age-matched healthy controls [28].
Some other studies demonstrated that in patients with psoriasis , the early detection of enthesitis on US may have prognostic implications on the prediction of subsequent development of PsA. In a 3.5-year follow-up, US assessment of a psoriatic patients cohort, up to 23 % of psoriatic patients with a higher baseline enthesitis score developed PsA [29]. In addition, the detection of hypervascularity at the entheses in patients with suspected early SpA and PsA was highly predictive of a future establishment of the diagnosis [30] .
Several ultrasonographic enthesitis-scoring indices for SpA, including PsA, have been published in the past decade. The Glasgow ultrasound enthesitis scoring system (GUESS) assesses lower-limb entheses including the superior and inferior pole of the patella, the distal insertion of the patellar tendon, the Achilles tendon, and the plantar fascia entheses [21] . The authors propose a scoring system of 0–36 based on the sum of the different US findings of enthesitis. Alcalde et al., based on the assessment of the same five enthesitis sites in the lower limbs, proposed a new score system of 0–36 based on US findings of acute injury and 0–40 based on findings considered to be chronic disease [22]. As these two previous studies only used grayscale US mode, de Miguel et al. added PD image information to the previous indices, with a further extension to 12 enthesitis sites, including upper-limb entheses, and published the Madrid Sonography Enthesitis Scoring Index (MASEI) [31].
Dactylitis in PsA
Dactylitis or “sausage digit” has classically been recognized as another characteristic feature of PsA [32] appearing in up to 30–48 % of patients according to different studies [33, 34] . In addition to PsA, it may be found in other SpA particularly reactive arthritis, gout , local infections of digits, sarcoidosis, and sickle cell disease. Very occasionally, it has also been reported in rheumatoid arthritis. The relatively high specificity of dactylitis in PsA leads to its inclusion in the clinical criteria for the classification of SpA suggested by Amor et al. [35]. Furthermore, due to its high sensitivity and adequate specificity, dactylitis has been included in the recent classification criteria generated by the CASPAR study group [14].
The clinical presentation of dactylitis is a uniform diffuse swelling affecting fingers in 24 %, toes in 65 % and both hands and feet in 12 % of PsA patients [34]. Dactylitis clinical manifestations may vary from significant local digital pain to an asymptomatic finding. It is accepted that dactylitis may present as an acute condition with painful inflammatory changes, or a chronic course, where the digit still remains swollen despite the disappearance of the pain [34].
Despite the incomplete agreement regarding the different tissue components involved in dactylitis [36–38], a recent meta-analysis published by Bakewell et al. [39] revealed that with the use of MRI and US for the assessment of this condition, the most common features were flexor tendon tenosynovitis and joint synovitis which appeared equally in 90 % of the patients, and extratendinous soft tissue thickening and extensor tendonitis which appeared in up to 50 % of patients. Other components, only qualitatively described in this literature review, were bone, extra and intra-articular osteoproliferation, erosions, bone edema, and plantar/palmar plate abnormalities . According to tissue-specific vascularity using Doppler-mode US or post-gadolinium MRI studies, the elementary components (not quantified) of dactylitis were joint synovitis, flexor tendon tenosynovitis, soft tissue edema, nail-bed abnormalities, bone extra and intra-articular osteoproliferation, and bone edema .
MSUS has demonstrated enough accuracy to identify the different tissue compartments involved in dactylitis, comparable to the findings obtained from MRI examination (Fig. 5.3):
Fig. 5.3
Ultrasound image of the different tissue compartments involved in dactylitis. Comparison with MRI image from the same patient with psoriatic arthritis (long arrows). a Synovitis affecting the metatarsophalangeal joint: distension of the joint capsule with hypoechoic content. b Flexor tendon tenosynovitis consisting of a thickening of the diameter of the tendon, with loss of the normal tendon echotexture. c Extratendinous soft tissue changes which are consistent with thickening of the subcutaneous tissue, with an increase of distance from skin to tendon and changes to the echotexture pattern of the soft tissues around the tendon. MRI magnetic resonance imaging
Joint synovitis, which frequently affects metacarpophalangeal, metatarsophalangeal as well as interphalangeal joints, has US pattern which is similar to and cannot be distinguished from other inflammatory conditions such as rheumatoid arthritis. It consists of a distension of the joint capsule with a hypoechoic content that can be displaced and compressed depending of the proportion of the effusion compared to synovial proliferation. Eventually, it may also exhibit tissue vascularity in Doppler mode.
Flexor tendon tenosynovitis consists of a thickening of the diameter of the flexor tendons and their sheaths, with loss of the normal tendon echotexture and distension of the tendon sheath with hypoechoic content, consistent with effusion and synovial proliferation, which eventually may exhibit vascularity in Doppler mode .
Extratendinous soft tissue changes are commonly seen in association with dactylitis and are consistent with thickening of the subcutaneous tissue, with increased distance from skin to tendon and changes in the echotexture pattern of the soft tissues around the tendon suggestive of subcutaneous tissue edema manifested clinically as local swelling.
Other features less commonly described include extra and intra-articular osteoproliferation, erosions, and plantar/palmar plate abnormalities. These are described in more detail later in this review .
Peripheral Arthritis
Despite peripheral joint synovitis in PsA seemingly undistinguished from other chronic inflammatory arthritic conditions, such as rheumatoid arthritis, some studies have demonstrated differences in the pathology identified by MSUS. In a study published by Fournie et al., they reported extra-synovial abnormalities which seemed to be specific to PsA such as enthesitis, thickening of soft tissues, and Doppler signal at the base of the nail suggestive of periungual psoriatic involvement [40].
US findings in peripheral joints with synovitis include distension of the joint capsule with an abnormal hypoechoic or anechoic intra-articular content—always relative to subdermal fat, but sometimes it may be isoechoic or hyperechoic. It potentially can be displaceable and compressible depending on the prevalence of synovial hypertrophy or effusion. When the predominant content is synovial hypertrophy, Doppler signal within the joint space can be identified (Fig. 5.4). An earlier study documented the higher sensitivity of US as a tool for the detection of synovitis in comparison to physical exam in any of the peripheral joints involved [41].
Fig. 5.4
Ultrasound image of synovitis affecting the third metatarsophalangeal joint of a patient with psoriatic arthritis. There are findings of distension of the joint capsule with an abnormal hypoechoic intra-articular content suggesting synovial hypertrophy ( white arrows) with Doppler signal within the joint space
As there is not any specific scoring system for peripheral synovitis in PsA, any of the semiquantitative US scoring systems published (0–3 where 0 = normal, 1 = mild, 2 = moderate, 3 = severe) for grading synovitis in rheumatoid arthritis could be potentially used also for grading the PsA-inflamed joints [42].
Bone erosions in PsA can be found in up to 60 % of patients [43]. They appear similar to those seen in rheumatoid arthritis and do not have any specific appearance on US exam. The typical image is a discontinuation in the bone surface (cortical defect) which should be visualized in longitudinal and transversal scans (Fig. 5.5). This cortical defect may be filled with inflammatory tissue and, eventually, may exhibit vascularity in Doppler mode (Fig. 5.6). Erosions also can be scored using a binary present/absent system or a 0–3 semiquantitative score [44]
Fig. 5.5
Ultrasound image of bone erosion in psoriatic arthritis. There is a discontinuation in the bone surface (cortical defect) which is visualized in a Longitudinal and b Transversal scans (white arrows)
Fig. 5.6
Ultrasound image of bone erosion in psoriatic arthritis filled with inflammatory tissue exhibiting vascularity in Doppler mode (white arrows)
Axial Disease
Most of the information available about the use of MSUS in axial disease in SpA and PsA has been focused on the sacroiliac joints. Sacroiliitis is an early feature of SpA, including PsA, and frequently is associated with inflammatory back pain and stiffness. However, due to the deep location of the sacroiliac joint, classically there have been some technical issues in obtaining a high-quality image of its anatomy using US. Early in the disease course, when X-ray examination is negative, the inflammation of the sacroiliac joint can be detected in more than a half of patients using MRI, which allows the detection of bone edema adjacent to the sacroiliac joints, as an early finding of sacroiliitis [45]. Therefore, bearing in mind the technical limitations, only a few articles on testing the US usefulness for evaluation of sacroiliac joints have been published.
In a recent study, Spadaro et al. analyzed the ability of US to detect joint effusion in sacroiliac joints in SpA patients. The prevalence of US-detected joint effusion was 38.9 % of sacroiliac joints among the SpA patients cohort compared to 1.7 % in the control group. In addition, the presence of inflammatory back pain was significantly associated with the presence of sacroiliac joint effusion assessed by US [46].
In another study carried out by Bandinelli et al., they reported that US could be a reliable imaging method for assessing the sacroiliac joint space. They compared the sacroiliac joint width and the thickness of the sacrotuberosus as well as posterior sacroiliac ligaments in patients with early SpA to those of healthy controls, revealing that early in the disease course the sacroiliac joint space width and the sacrotuberosus ligament thickness was significantly higher in patients compared with controls [47]
The US examination technique of the sacroiliac joint should be performed with the patient in a prone or knee–chest position. The bony landmarks to identify for guiding the examination are the midline of the sacrum and the iliac wings which can be easily identified as a hyperechogenic surface laterally to the spinous processes of the sacral bone. With the transducer in a transverse position, the sacroiliac joint space is identified as a hypoechoic gap between the hyperechoic margins of the joint, sacrum, and iliac bone. In this location of the transducer, the findings of synovitis with effusion appear as the presence of a hypoechoic area within and slightly over the joint space [48, 46]. At this position, and switching to Doppler mode, eventually, an increased perfusion around or inside the sacroiliac joint can be detected in up to 48 % of patients with sacroiliitis [48](Fig. 5.7).
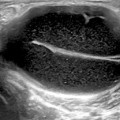
Fig. 5.7
Ultrasound (US) image of right sacroiliitis in a patient with psoriatic spondyloarthropathy (short axis). The US findings of synovitis with effusion appear as the presence of a hypoechoic area within and slightly over the joint space (black arrows). Switching to Doppler mode, there is an increased perfusion inside the sacroiliac joint
Despite the lack of studies to support the real usefulness of the US in the assessment of sacroiliac joints, the few of them previously discussed, would suggest that this imaging modality could be useful in providing real-time, less expensive, comparative, and repeated images of the sacroiliac joints in SpA and PsA.
There are a very limited number of published data on the use of US in the spine in patients with SpA and PsA. Unlu [49], using color and duplex Doppler US, reported how the resistive index of blood vessels of sacroiliac joints and thoracic and lumbar vertebral paraspinal areas was significantly reduced in 39 patients diagnosed with SpA compared to controls. Interestingly, after a course of anti-TNF therapy in the same patients, the authors observed a significant increase in the resistive index at the level of sacroiliac joints and lumbar vertebral paraspinal areas [10




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree