9
Appendix
Appendicitis
Overview
 Most common in teenage years and patients in their 20s
Most common in teenage years and patients in their 20s
 Rate of appendectomy for appendicitis is 10 per 10,000 patients per year
Rate of appendectomy for appendicitis is 10 per 10,000 patients per year
 Usually due to lymphoid hyperplasia or fecalith causing luminal obstruction
Usually due to lymphoid hyperplasia or fecalith causing luminal obstruction
Signs and Symptoms
 Anorexia (90%)
Anorexia (90%)
 Abdominal pain: Periumbilical migrating to RLQ
Abdominal pain: Periumbilical migrating to RLQ
 Nausea and vomiting (70%)
Nausea and vomiting (70%)
 Low-grade fever
Low-grade fever
Physical Examination Findings
 Point tenderness typically over McBurney point
Point tenderness typically over McBurney point
 Psoas sign: Pain with extension of right thigh while in left lateral decubitus position
Psoas sign: Pain with extension of right thigh while in left lateral decubitus position
 Obturator sign: Pain with passive rotation of flexed right hip
Obturator sign: Pain with passive rotation of flexed right hip
 Rovsing’s sign: Pain in RLQ while palpating LLQ
Rovsing’s sign: Pain in RLQ while palpating LLQ
 Rectal examination may reveal a pelvic mass or abscess
Rectal examination may reveal a pelvic mass or abscess
Laboratory Findings
 Patients can have a normal WBC count, but usually mild leukocytosis in the range of 10,000 to 18,000/mm3
Patients can have a normal WBC count, but usually mild leukocytosis in the range of 10,000 to 18,000/mm3
 Urinalysis may be positive with pyuria, hematuria, and albuminuria
Urinalysis may be positive with pyuria, hematuria, and albuminuria
Treatment
 IV fluid resuscitation and peri-operative antibiotics
IV fluid resuscitation and peri-operative antibiotics
 Laparoscopic or open appendectomy
Laparoscopic or open appendectomy
 For perforated appendix, may undergo appendectomy if there is no inflammatory phlegmon. If there is an inflammatory phlegmon, conservative management with IV antibiotic, with percutaneous drainage of any associated abscess
For perforated appendix, may undergo appendectomy if there is no inflammatory phlegmon. If there is an inflammatory phlegmon, conservative management with IV antibiotic, with percutaneous drainage of any associated abscess
KEY POINT
 The risk of a ruptured appendicitis increases at 24 hours from the initial presentation of signs and symptoms
The risk of a ruptured appendicitis increases at 24 hours from the initial presentation of signs and symptoms
RADIOLOGY
Appendicitis
 Plain film findings
Plain film findings
• Usually normal
• Adynamic ileus may be seen
• Sometimes, a calcified appendicolith in the right lower quadrant is seen
 US findings
US findings
• Blind-ending tubular structure that is noncompressible, outer wall to outer wall diameter greater than 6 mm
• If identified, an appendicolith casts a clean posterior acoustic shadow
• Tenderness over appendix
• False negative can result from retrocecal appendicitis, gangrenous or perforated appendicitis, gas-filled appendix, and massively enlarged appendix
 CT findings (Fig. 9.1)
CT findings (Fig. 9.1)
• Appendix measuring greater than 6 mm in diameter, failure of appendix to fill with oral contrast or air up to its tip
• Adjacent cecal thickening due to edema at the origin of the appendix
• Inflammation/fatty stranding/fluid in the retroperitoneum/frank abscess
• Appendicolith
 MRI findings
MRI findings
• Dilated, thickened appendix with adjacent inflammation seen on contrast-enhanced T1-weighted and T2-weighted images
FIGURE 9.1 A,B
A. Vertebra
B. Psoas muscle
C. Colon
D. Stomach
E. Spleen
F. Bladder
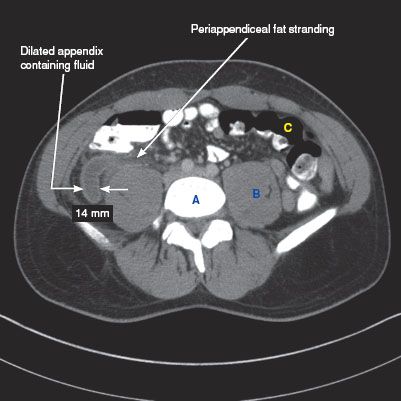
FIGURE 9.1 A
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree