Key Points
- •
Use of ultrasound to guide arterial line placement increases success rate of cannulation and reduces periprocedural complications.
- •
Nontraditional arterial cannulation sites with few landmarks can be accessed using ultrasound guidance.
- •
Arteries can be differentiated from veins using ultrasound based on compressibility, pulsatility, and Doppler appearance.
Background
Arterial cannulation is performed to facilitate hemodynamic monitoring, measure cardiac output, and sample arterial blood. Historically, this procedure was performed using landmark-based techniques, and success depended on knowledge of vascular anatomy and clinical experience. A major limitation of landmark-based techniques is variance in patient anatomy due to obesity, edema, vessel thrombosis, and congenital anomalies. Repeated attempts at arterial cannulation may become progressively more difficult secondary to arterial vasospasm, hematoma formation, or intimal dissection.
Ultrasound guidance for arterial cannulation has been shown to increase the success rate of cannulation while reducing the number of attempts, time to cannulation, and complications. In a meta-analysis of randomized controlled trials comparing radial artery cannulation with and without ultrasound guidance, ultrasound guidance improved first-attempt success rates by 71%. Ultrasound guidance has also been shown to facilitate arterial access in patients with low perfusion and after multiple failed attempts using a landmark-based technique. Ultrasound can guide arterial access at traditional insertion sites, such as radial, femoral, brachial, or dorsal pedis arteries, as well as nontraditional insertion sites, such as axillary, ulnar, and temporal arteries, where landmarks are not useful.
Anatomy
Radial Artery
The radial artery is the most common site for arterial cannulation. The artery’s superficial location, ease of access, and low rate of complications make it a favorable site. Also, the dual blood supply to the hand provided by the radial and ulnar arteries minimizes the risk of distal ischemia if a complication arises resulting in loss of radial artery blood flow. The necessity and optimal method to assess adequacy of collateral blood flow to the hand before radial artery cannulation is controversial. The modified Allen test is most commonly used, although a number of studies refute its predictive value.
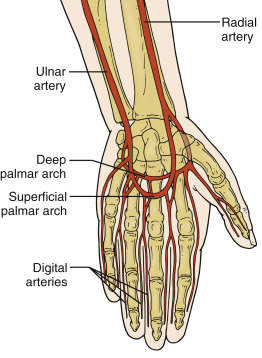
At the level of the wrist, the radial artery is superficial and lies medial to the brachioradialis tendon and lateral to the flexor carpi ulnaris tendon ( Figure 30.1 ). Cannulation proximal to the wrist is more challenging because the artery runs deep through the brachioradialis muscle. Anatomic variants of the origin or course of the radial artery occur in up to 30% of the population.
Brachial Artery
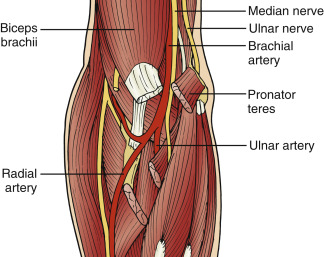
The brachial artery is a continuation of the axillary artery and can be palpated on the medial side of the antecubital fossa. The brachial artery lies along the medial border of the biceps brachii muscle and the lateral border of the pronator teres muscle ( Figure 30.2 ). This location is the most accessible site for brachial artery cannulation. Some prefer a more proximal insertion site where there is less chance of kinking or occluding the catheter. The brachial artery is a less favored site for cannulation because it lacks the benefit of collateral circulation, and obstruction may lead to compromise of radial and ulnar perfusion, resulting in distal ischemia.
Femoral Artery
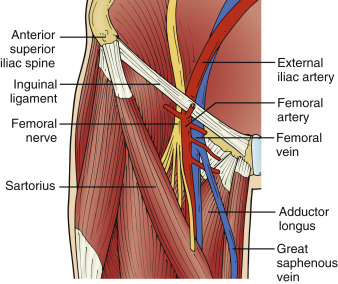
After the external iliac artery crosses beneath the inguinal ligament, it is called the femoral artery . The femoral artery is contained within a neurovascular bundle lateral to the femoral vein and medial to the femoral nerve ( Figure 30.3 ) in the femoral triangle. The superior border of the femoral triangle is the inguinal ligament, the medial border is the adductor longus muscle, and the lateral border is the sartorius muscle. The femoral artery is palpated midway between the anterior superior iliac spine and the symphysis pubis. In 65% of patients, a portion of the common femoral artery overlaps the common femoral vein. The large vessel diameter and abundant collateral circulation make the femoral artery a favorable site for cannulation.
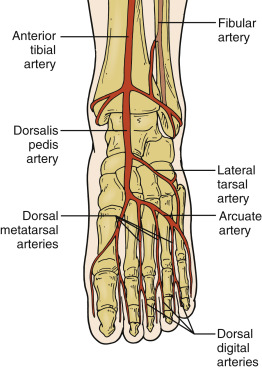
Dorsalis Pedis
The dorsalis pedis artery runs from the level of the ankle along the medial side of the dorsal foot to the great toe ( Figure 30.4 ). The dorsal pedis artery can be palpated between the tendons of the extensor hallucis longus laterally and the extensor digitorum longus medially. The dorsalis pedis artery is a less favored site for cannulation because it is distant from the central circulation and difficult to cannulate in patients with hypotension or peripheral vascular disease.
Technique
The technique for ultrasound-guided arterial cannulation is similar at all sites. A general description of the procedure is followed by site-specific details.
Preparation
A high-frequency (≥7 MHz) linear array transducer is required. Higher-frequency transducers provide better resolution of superficial structures close to the skin surface. The ultrasound screen should be in the direct line of sight of the operator. Aligning the operator, transducer, target vessel, and screen minimizes head turning during needle insertion. The entire procedure should be performed using sterile technique. Skin overlying the insertion site should be sterilized using a chlorhexidine-based solution per local protocol. Procedure supplies should be placed on a sterile field within the operator’s close reach; specifically the guide wire, scalpel, and catheter should be within reach. A sterile transducer cover should be placed over the transducer, using sterile gel both inside and outside of the sterile cover.
Percutaneous cannulation may be performed using an over-the-wire (modified Seldinger technique) or over-the-needle technique. A guide wire is advanced through the needle into the vessel lumen before catheter advancement in the modified Seldinger technique. A 20-gauge, 3–5 cm Teflon catheter is most commonly used for radial, brachial, or dorsalis pedis artery cannulation. For the femoral artery, a longer catheter length is required, usually 12–15 cm.
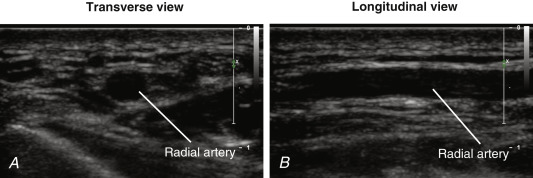
Imaging depth varies depending on the insertion site and patient’s body habitus. The transducer should be held in the operator’s nondominant hand. The artery is identified in a transverse (short-axis ) view ( Figure 30.5 A ), and then the transducer is rotated 90 degrees to visualize the artery in a longitudinal (long-axis) view ( Figure 30.5 B ). Several characteristics differentiate arteries from veins by ultrasound appearance. Arteries are pulsatile with lumens that cannot be fully collapsed by external compression from the transducer. Arterial walls are thicker and more echogenic. Color flow Doppler of arteries shows pulsatile flow that is detected predominantly during systole ( Figure 30.6 ), and the color cannot be completely obliterated with external compression of the vessel. Flow may appear turbulent due to high velocities within the artery. Pulsed-wave Doppler of arteries shows a systolic-diastolic pattern with high velocities.