Arteries of the Pelvis
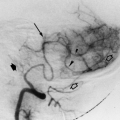
The right and left iliac arteries have been described as the terminal branches of the abdominal aorta (Fig. 19.1). The abdominal aorta bifurcates at the level of the fourth lumbar vertebra, into two large arteries, the right and left common iliac arteries, supplying the pelvis and the lower extremities. The right common iliac artery crosses to the right over the left common iliac vein, very often causing compression of that vein with occlusion or severe stenosis. Compression of the left iliac vein may cause hypertension in the venous circulation of the left lower extremity and deep venous thrombosis, known as iliac compression syndrome, May-Thurner syndrome, or Cockett syndrome. The anatomic abnormality is present in 15% to 20% of the population. The wall of the common iliac vein thickens and progressive occlusion develops. Adhesion of the iliac vein wall is observed in some cases to cause obstruction (Fig. 19.2). The common iliac arteries usually do not have branches above the bifurcation into the external iliac artery and internal iliac artery. Occasional branches of the common iliac arteries are inferior renal polar arteries with an abnormal origin from the common iliac, usually in a situation of multiple renal arteries. Ectopic pelvic kidneys are rare, in about 0.1% of the population, and single or multiple renal arteries may also originate from the iliac arteries, most commonly from the common iliac arteries. The common iliac artery may give small branches to the surrounding tissues, peritoneum psoas muscle, ureter, and pelvic nerves. The common iliac arteries divide into the external iliac artery, which runs parallel to the axis of the common iliac artery, and the internal iliac artery, which is a posteromedial branch.
Common Iliac Arteries
Internal Iliac Arteries (Hypogastric Arteries)
Internal Iliac Arteries (Hypogastric Arteries)
These arteries are about 4 cm in length, resulting from the bifurcation of the common iliac arteries (Figs. 19.1, 19.2, 19.3). The internal iliac arteries terminate in two main stems (bifurcation), one anterior and one posterior, in 57% to 77% of the general population. The branches of the anterior trunk supply the bladder, the uterus, the rectum, the vagina, and through the obturator artery, supply pelvic bone and muscles, inside and outside the pelvis. The posterior trunk branches supply the bones, muscle, and nerves, including proximal lumbar and sacral nerves, which will form the sciatic nerve. Absence of the internal iliac artery is rarely observed.
In the fetus, the internal iliac artery is larger than the external iliac artery and is a direct continuation of the common iliac artery. As the superior vesical artery ascends on the anterior abdominal wall to the umbilicus, it converges with the contralateral superior vesical artery. After passing the umbilical opening, the artery is named umbilical and enters the umbilical cord, coiling around the umbilical vein, thereby reaching the placenta. At birth when the placental circulation ceases, the artery closes down and only the pelvic segment of the internal iliac artery remains, and the remainder turns into a fibrous cord receiving the name of medial umbilical ligament.
Superior Vesical Artery (Fetal Umbilical Artery)
Supplies
Vesical fundus
Ductus deferens
Ureteral arteries
Inferior Vesical Artery (May Arise with the Middle Rectal Artery)
Supplies
Vesical fundus
Prostate (prostatic branches communicate across the midline)
Seminal vesicle
Lower ureter
Ductus deferens
Middle Rectal Artery
Anastomoses with the superior and inferior rectal arteries
Supplies
Lower rectum
Seminal vesicle
Prostate
Bladder walls
Uterine Artery (Fig. 19.8)
The uterine artery is a branch from the anterior division of the internal iliac artery. The artery penetrates the anterior or posterior wall of the uterus itself. At the level of the internal os, the arteries course at right angles to the long axis of the uterus. Below the internal os, the arteries are inclined downward; above this level the inclination is upward. The terminal branch of the uterine artery is the intramural branch, also described as the arcuate artery. The arcuate arteries lie between the outer and the middle third of the uterine wall, either anterior or posterior. The arcuate arteries terminate in medial peripheral and radial branches. Free anastomoses between the arcuate arteries on either side of the uterus can be seen. The blood supply of the tube and the ovary is derived from both the uterine and the ovarian arteries. In general, the uterine supplies the medial half of the ovary and the medial two thirds of the tube, whereas the remainder of the blood supply arises from the ovarian artery. The ovarian artery alone may supply the entire tube and the ovary.
The uterine artery crosses above the ureter, and there is a ureteric branch. It anastomoses with the vaginal arteries, forming the azygos artery of the vagina. The cervicovaginal branch arises directly from the uterine artery in 91% of cases, whereas in 9% its origin is directly from the internal iliac artery (Fig. 19.9, 19.10, 19.11, 19.12). The origin of the uterine artery is extremely variable, but four different patterns have been identified. Type I is defined as the uterine artery arising as the first branch of the inferior gluteal artery (45%). Type II is defined as the uterine artery arising as the second or third branch of the inferior gluteal artery (6%). Type III is a true trifurcation, wherein the origins of the superior gluteal, inferior gluteal, and uterine arteries are at the same level (43%). In type IV, the uterine artery origin is proximal to the bifurcation of the anterior and posterior division (6%). However, in a recent publication, the classification of the uterine artery was inconclusive in 23% of the cases, and not possible to be studied in 39% of the angiograms.
Uterine Artery Supplies
Ureter
Vagina
Uterus
Broad ligament of uterus
Round ligament of uterus
Uterine tube and part of the ovary
The tortuous terminal branches in the uterus are called helicine arteries
Ovarian Artery
Knowledge of the ovarian artery anatomy is important for the success of certain procedures of embolization on pelvic organs such as in uterine fibroids. An important implication of the ovarian artery-to-uterine artery communications is the possibility of ovarian failure and premature menopause after uterine artery embolization. There are three main patterns of anastomoses between the ovarian artery and the uterine artery following a physiologic point of view.
Type Ia—The ovarian artery is the major source of blood supply to the fibroid in the uterus by means of anastomosis with the intramural uterine artery. In this case, the flow in the tubal artery is toward the uterus, without evidence of retrograde reflux in the direction of the ovary (13.2%). Type Ib—The ovarian artery supplies the fibroid in the uterus in a similar manner as that of type Ia. Flow in the tubal artery was toward the uterus; however, reflux into the ovarian artery is seen on the preembolization selective uterine artery angiogram (8.6%). Type II—The ovarian artery supplies the fibroids directly. Some anastomoses to the intramural uterine artery may exist. The flow to the fibroid was independent from the uterine artery (3.9%). Type III—Flow in the tubal artery is toward the ovary on selective uterine angiograms. There is washout of the contrast toward the ovary (6.6%).
Vaginal Artery
The vaginal artery may be two or three arteries and corresponds to the inferior vesical artery in males.
Supplies
Vagina
Vesical fundus
Rectum
Obturator Artery
This artery leaves the pelvis through the obturator canal and has an anterior and a posterior branch (Figs. 19.1, 19.5, 19.6).
Branches
Inside the Pelvis
Iliac branches
Vesical branch
Pubic branch
Outside the Pelvis
Anterior and posterior branches encircle the foramen
Anterior branches supply various muscles and anastomoses with the medial circumflex femoral artery
Posterior branches supply various muscles and anastomoses with the inferior gluteal artery; give an acetabular branch that supplies the acetabular fossa and the femoral head through the ligament of the femoral head
A pubic branch of the inferior epigastric artery may replace the obturator artery. It may be a branch either of the anterior or posterior trunks of the internal iliac artery and may be a branch of the superior or inferior gluteal artery.
The internal pudendal artery is the smaller branch of the anterior trunk of the internal iliac artery.
Supplies the external genitalia.
Branches
Inferior rectal artery (anastomoses with the contralateral inferior rectal artery and with the superior and middle rectal arteries)