Arthropathies/Connective Tissue Diseases
Thomas H. Berquist
Protocols
Key Facts
Routine radiographs remain the primary screening technique for evaluating arthropathies.
Anteroposterior (AP), lateral, and oblique views of involved joints should be obtained. New digital techniques permit windowing, bone detail techniques, and magnification to more effectively evaluate subtle bone and soft tissue changes.
Radionuclide scans are sensitive for detecting early changes in articular disease. Technetium-99m methylene diphosphonate is injected intravenously (15 to 20 mCi), and images of the involved joints are obtained 2 to 3 hours after injection. Increased radiotracer is seen in bones and joints because of early synovitis and osseous inflammation. Findings are not specific.
Ultrasound has demonstrated increased utility for evaluating ligaments, tendons, and intra-articular pathology. High-frequency transducers are used for superficial structures (>7 to 12 MHz). Transverse, longitudinal, and dynamic images are obtained.
Computed tomography (CT) is used primarily for surgical treatment planning. Bone stock and extent of erosions can be evaluated. Thin sections (1 mm at 0.5-mm intervals) allow coronal and sagittal reformatting and three-dimensional reconstructions.
Magnetic resonance (MR) techniques are useful for detection of early bone and soft tissue changes. Specific techniques have gained popularity for evaluating synovium and articular cartilage.
Synovial inflammation:
T2-weighted spin-echo or fast spin-echo sequences in coronal and axial planes
Intravenous gadolinium (0.1 to 0.2 mmol/kg body weight) followed by fat-suppressed T1-weighted images 15 to 60 minutes after injection. Early synovial inflammation is more easily appreciated. Bolus injections with dynamic fast scan techniques are useful for evaluating active synovitis and remissions.
Articular cartilage can be evaluated on contrast-enhanced images or by using double-echo steady state or fat-suppressed fast spin-echo proton density sequences.
Suggested Reading
Eustace S, DiMasi M, Adams J, et al. In vitro and in vivo spin-echo diffusion imaging characteristics of synovial fluid: Potential noninvasive differentiation of inflammatory and degenerative arthritis. Skel Radiol 2000;29:320–323.
Goupille P, Roulot B, Akoka S, et al. Magnetic resonance imaging: A valuable method for detection of synovial inflammation in rheumatoid arthritis. J Rheumatol 2001;28:35–40.
Lin J, Fessell DP, Jacobson JA, et al. An illustrated tutorial of musculoskeletal ultrasound: Part 1, introduction and general principles. AJR Am J Roentgenol 2000;175:637–645.
Rose PM, Demlow TA, Szumowski J, et al. Chondromalacia patella: Fat suppressed MR imaging. Radiology 1994;193:437–440.
Rheumatoid Arthritis
Key Facts
Clinical: Rheumatoid arthritis (RA) affects 1% to 2% of the general population with permanent deformity and disability in 10% to 20%. Characteristically, RA is a symmetric polyarthropathy. Diagnostic criteria of the American Rheumatism Association are as follows:
Morning stiffness lasting 1 hour before improvement
Soft tissue swelling of three or more joint areas noted on physical examination
Swelling of wrists, metacarpophalangeal joints, and proximal interphalangeal (PIP) joints
Symmetric swelling
Rheumatoid nodules
Positive rheumatoid factor
Radiographic erosions with or without juxta-articular osteopenic in hand, wrist, or both
Criteria 1 to 4 must be present for 6 weeks. If four or more criteria are present, the criteria are 91% to 94% sensitive and 89% specific for RA.
Age: 25 to 55 years
Sex: Females outnumber males 3:1.
Distribution: PIP joint, metacarpophalangeal joint, wrist, metatarsophalangeal (MTP) joint, ankles, knees, shoulders, and, to a lesser extent, hips, and spine
Laboratory findings: positive rheumatoid factor, elevated erythrocyte sedimentation rate
Radiographic features:
Early
Soft tissue swelling around involved joints
Juxta-articular osteopenia
Subtle marginal bone erosions
Late
Osteopenia (diffuse)
Joint space narrowing
Obvious erosions
Joint subluxations
Soft tissue atrophy
Rheumatoid nodules
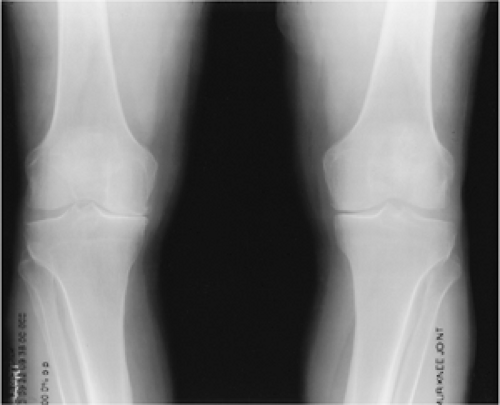
 FIGURE 13-1 Early RA. (A,B) Bilateral posteroanterior views of the hands showing subtle swelling (arrows) and juxta-articular osteopenia. |
 FIGURE 13-2 Coronal contrast-enhanced fat-suppressed T1-weighted image demonstrates early changes of RA with erosions (arrowheads) and synovial enhancement. |
Suggested Reading
Brower AC. Arthritis in black and white, 2nd ed. Philadelphia: WB Saunders; 1997:195–224.
Huh YM, Suh JS, Jeong EK, et al. Role of inflamed synovial volume of the wrist in redefining remission of rheumatoid arthritis with gadolinium enhanced 3D-SPGR MR imaging. J Magn Reson Imaging 1999;10:202–208.
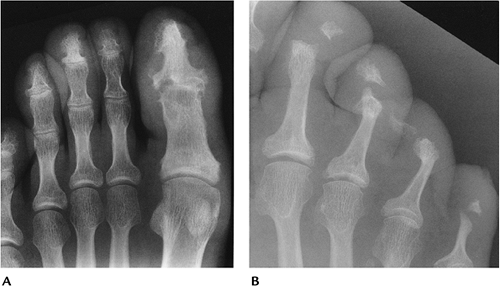
Psoriatic Arthritis
Key Facts
Clinical:
Psoriatic arthritis occurs in 2% to 6% of patients with psoriasis. Psoriatic arthritis comprises approximately 5% of patients with polyarthropathy. Arthritis may precede or coincide with skin manifestations.
Age: 25 to 55 years
Sex: no sex predilection
Distribution: hands, feet, sacroiliac joints (50%), and spine, in order of decreasing frequency
Laboratory findings: negative rheumatoid factor, elevated erythrocyte sedimentation rate, human leukocyte antigen (HLA)-B27 antigen often positive.
Imaging features:
Bilateral, but asymmetric involvement
Fusiform (entire digit) soft tissue swelling
Normal bone density (no osteopenia)
Marked joint space narrowing
“Pencil in cup” erosions
Bone proliferation
Distal joints (distal interphalangeal [DIP] and PIP) of hands and feet (compared with proximal) are more commonly involved in RA.
 FIGURE 13-5 Psoriatic arthritis both hands. Erosive changes in the interphalangeal and DIP joints. Subluxations are not usually a prominent feature of psoriatic arthritis. |
Suggested Reading
Resnick D, Kransdorf MJ. Psoriatic arthritis. In: Resnick D, Kransdorf MJ, eds. Bone and joint imaging, 3rd ed. Philadelphia: Elsevier-Saunders; 2005:288–297.
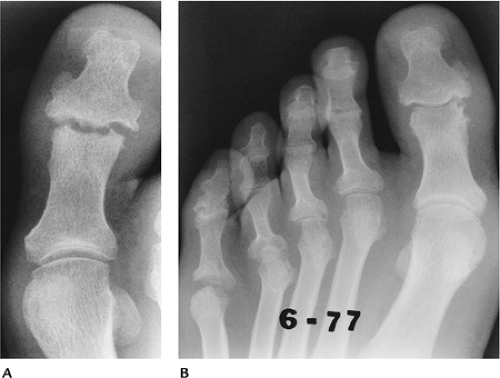
Reiter Syndrome
Key Facts
Clinical:
Reiter arthropathy typically is associated with conjunctivitis and urethritis. Patients also may have fever and weight loss. This triad is sexually transmitted. In females, the arthropathy is associated with dysentery.
Age: 15 to 35 years
Sex: most common in males
Distribution: feet, ankles, knees, sacroiliac joints. Upper extremity involvement uncommon.
Laboratory findings: HLA-B27 antigen positive in 75%
Imaging features:
Bilateral asymmetric joint involvement
Fusiform (entire digit) soft tissue swelling
Joint space narrowing
Bone proliferation
Ill-defined erosions
Normal mineralization
 FIGURE 13-7 Reiter involvement of the plantar aspect of the calcaneus with irregular bone proliferation. |
Suggested Reading
Weldon WW, Scaletter R. Roentgen changes in Reiter syndrome. AJR Am J Roentgenol 1961;86:344–350.
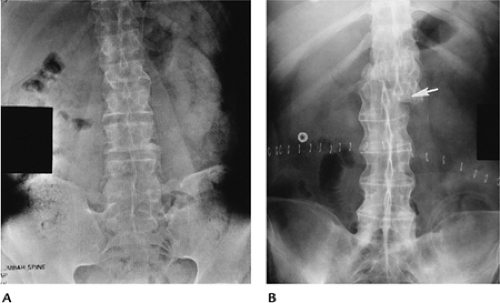
Ankylosing Spondylitis
Key Facts
Clinical:
Ankylosing spondylitis is an inflammatory condition that affects primarily the axial skeleton. Patients typically are young males who present with low-back pain. Patients also may have weight loss and low-grade fever.
Age: 15 to 35 years
Sex: Males outnumber females 4:1 to 10:1.
Distribution: sacroiliac joints, spine (lumbar to cervical), hips, knees, shoulders. Peripheral joints of hands and feet less common (10% with long-standing disease).
Laboratory findings: HLA-B27 antigen frequently positive, elevated erythrocyte sedimentation rate
Imaging features:
Bony ankylosis of involved joints
Bilateral symmetric involvement of sacroiliac joints
Bone mineral normal early; osteopenic after ankylosis
Minimal erosive changes
Suggested Reading
Brower AC. Arthritis in black and white, 2nd ed. Philadelphia: WB Saunders; 1997:257–272.
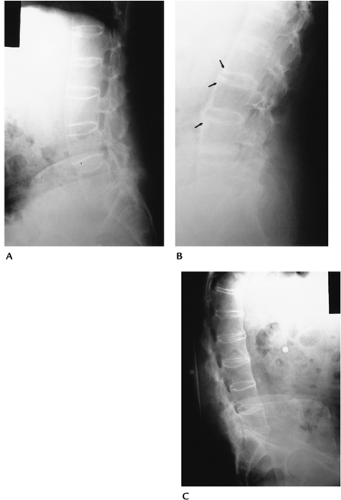
Osteoarthritis
Key Facts
Clinical:
Osteoarthritis is the most common arthropathy and increases in incidence with age. Osteoarthritis may occur after other arthropathies (secondary osteoarthritis). Degenerative joint disease may be genetic, or the result of age, occupation, or multiple factors. Patients present with pain and swelling in the involved joints.
Age: more than 50 years
Sex: no sex predilection
Distribution: hands (DIP and PIP joints), feet, knees, and hips. Elbows and shoulders less commonly involved.
Laboratory findings: none
Imaging features:
Asymmetric joint space narrowing
Subchondral sclerosis
Subchondral cysts
Osteophyte formation
Subluxations (less dramatic than RA)
Unilateral or bilateral involvement, but asymmetric
 FIGURE 13-13 AP radiograph of the pelvis demonstrating advanced degenerative arthritis in the right hip with osteophytes and bone sclerosis.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|