Fig. 38.1
Classification of breast imaging artifacts
38.2.1 Artifacts in Analog and Digital Mammography
The artifacts appear as either lighter (minus) or darker (plus) lines, specks or blotches.
38.2.1.1 Film-Related Artifacts
Analog mammography involves the use of hard-copy films and is associated with related artifacts due to technical errors in processing, film handling, and storage (Minigh 2009). Roller marks cause plus-density parallel lines that lie perpendicular to the film travel. Guide shoe marks appear as plus- or minus-density lines parallel to the direction of film travel. Delay streaks appear as plus-density deposits of developer. Wet pressure produces plus-density blotched artifacts. Too dark or too light films are caused by improper developer, improper fixer, or faulty film batch.
Dust causes artifacts that resemble calcifications. Fingerprints produce artifacts that may mimic calcifications. Foreign bodies on the screen (e.g., pencil marks, fingernail polish, cleaning tissues) mimic linear or mass-like artifacts. Stains and blotches may mimic a mass. Scratches appear as sharp linear artifacts. Static electricity artifacts appear as jagged or star like plus densities. Improper film storage or loading, a cracked cassette, or damaged safelight filters can result in film fogging, light leaks, and upside-down film artifacts.
38.2.1.2 Equipment-Related Artifacts
These refer to mammography machine-related artifacts. These artifacts may be due to incorrect collimation, incomplete grid motion, Bucky failure, and compression system failure (Ikeda 2004).
The equipment-related artifacts that occur in analog mammography can also occur in digital mammography with additional laser printer artifacts and image-display monitor artifacts (Ikeda 2004; Rotenberg et al. 2004; Lewin et al. 2004; Bloomquist et al. 2006; Yaffe et al. 2006). Detector miscalibration artifacts are the most common artifacts in digital mammography. Remedies for prevention of these artifacts include mandatory regular quality control tests of the equipment.
38.2.1.3 Patient-Related Artifacts
Various materials in or on patients may cause artifacts: deodorants, talcum powder, clothing, tattoos, pacemaker, or foreign bodies (charm needles). Motion artifacts are caused by patient breathing and pulling. Positioning artifacts such as belly fold (Fig. 38.2), pectoral muscle fold (Fig. 38.3), hand artifact (Fig. 38.4), chin artifact (Fig. 38.5), and skinfold artifact (Fig. 38.6a–c) are more common phenomenon in the geriatric age group. Motion artifacts are caused by breathing or movement during acquisition (Fig. 38.7). Foreign material artifacts may be due to deodorant/talcum powder (Fig. 38.8).
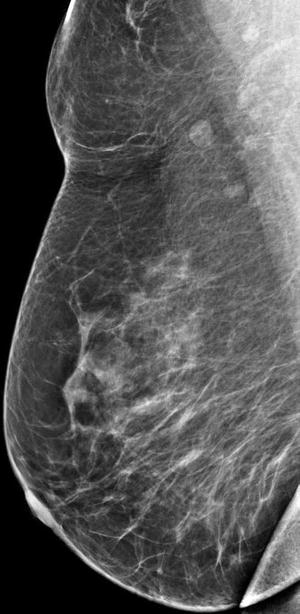
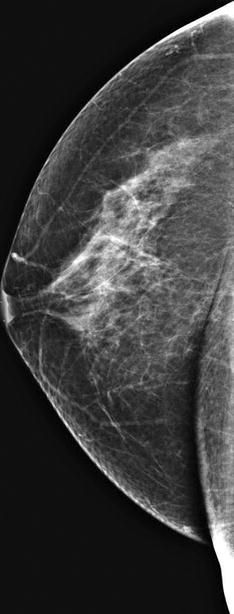
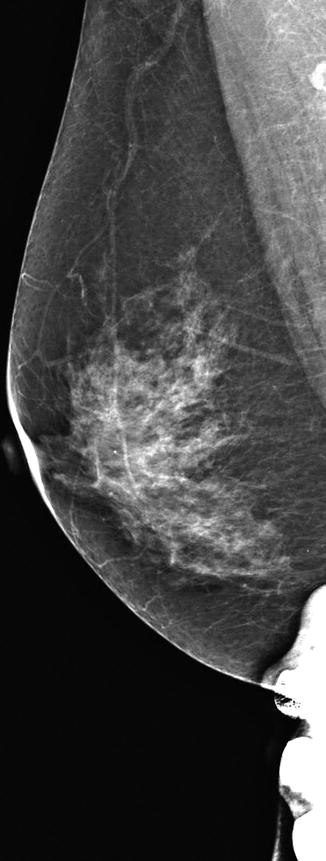
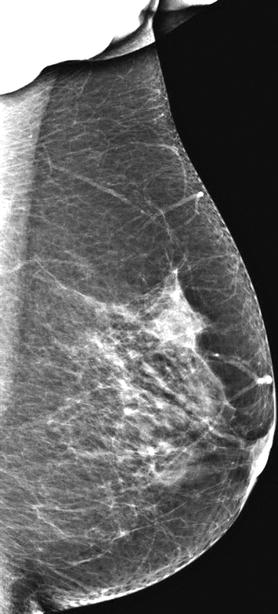
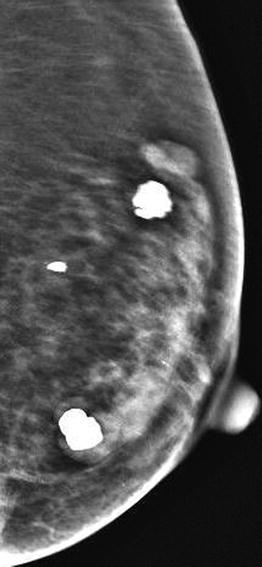
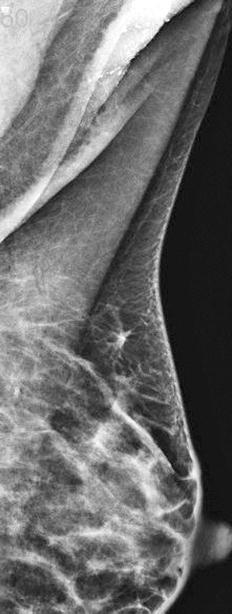
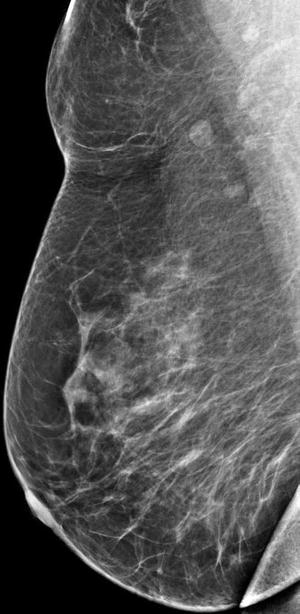
Fig. 38.2
Mammogram (MLO view) shows a belly fold at the inferior aspect of the breast
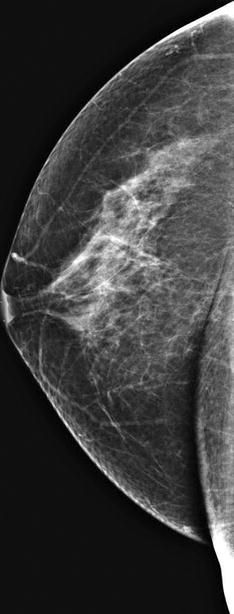
Fig. 38.3
Mammogram (CC view) shows a pectoral muscle fold
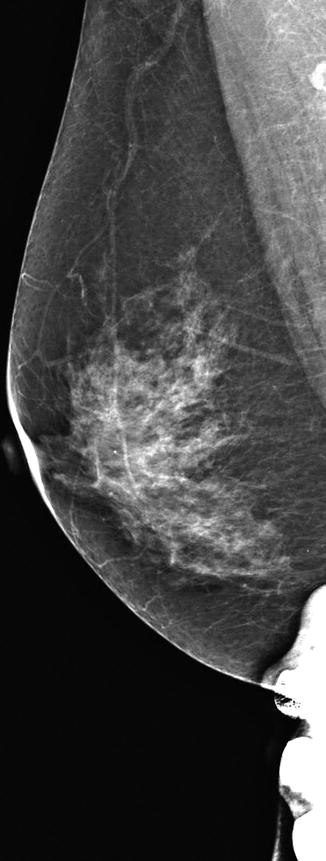
Fig. 38.4
Mammogram (MLO view) shows a hand artifact at the inferior aspect of the breast
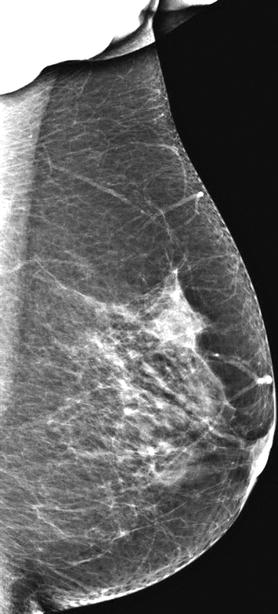
Fig. 38.5
Mammogram (MLO view) shows a chin artifact at the superior aspect of the breast
Fig. 38.6
(a) Mammogram (CC view) shows a chest wall skinfold. (b) Mammogram (CC view) shows a chest wall artifact at the medial aspect of the breast. (c) Mammogram (CC view) shows a chest wall artifact at the lateral aspect of the breast. (d) Mammogram (MLO view) shows an axillary skinfold
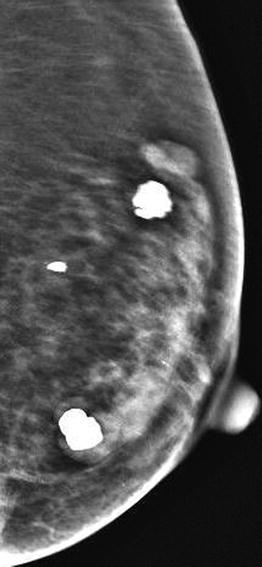
Fig. 38.7
Mammogram (MLO view) shows motion artifacts
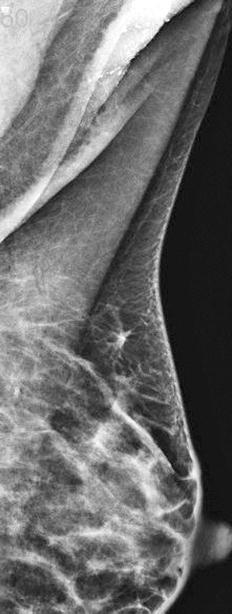
Fig. 38.8
Mammogram (MLO view) shows deodorant/talcum powder artifact mimicking microcalcifications in the axilla
Achieving an optimal mammographic image requires full patient cooperation. Patient-related artifacts, positioning as well as motion artifacts, occur more frequently in the geriatric age group. The aged loose skin is easily trapped in the compression paddle, causing a skinfold artifact. A poorly or noncooperative patient who has difficulty in understanding is often unable to follow instructions that are required to attain appropriate position.
Poorly mobile or wheelchair-bound patients, often old, are not able to achieve and maintain adequate position which leads to positioning artifacts and artifacts caused by breast motion, uncontrollable breathing, and insufficient compression. Remedies for patient-related artifacts include reduction of patient motion by optimizing patient’s comfort and careful explanation which helps alleviate the anxiety of examination and may improve cooperation.
38.2.1.4 Mammogram Interpretation Pitfalls
There is the risk of false positives. Abnormalities that are visible on both views may not be the same lesion. The distance of the lesion from the nipple should be checked. An additional true lateral view may help if confirmation needed. Finding the lesion in the breast should not stop one from a complete systematic survey of the mammograms; if not, other abnormalities, such as a smaller second lesion, clusters of microcalcifications, an axillary abnormality, or a lesion in the other breast, may be missed.
The area of interest may not be included in mammogram if it is too peripheral, too posterior, too high in the axillary tail or hidden in a large breast. Additional extended views, spot compression views, or 3D digital tomosynthesis, if available, can be used for evaluation. Problematic asymmetric density may be evaluated by spot view, true lateral view, or 3D digital tomosynthesis, if available. An apparent cluster of microcalcifications or intramammary mass on standard views may be actually dermal.
38.2.2 Artifacts in Breast Ultrasound
Artifacts may arise from any physical, electronic, or technical phenomenon which can cause abnormal echogenicity or acoustic shadowing on ultrasound.
38.2.2.1 Grayscale Ultrasound Artifacts
Crystal dropout causes a focal image defect extending from the skin downwards. Inappropriate dynamic range – the optimal value is 55–60 dB for breast – may reduce image details. Improper gain setting influences the image, making cysts appear solid or solid masses appear cystic. Reverberation artifacts are series of bright echoes paralleling an interface, commonly seen reflecting from needles, from the anterior wall of the cyst (Fig. 38.9) or from silicone implants. “Ring-down” artifacts are the echogenic bands perpendicular to the transducer, typically from air collection. Specular reflection artifacts occur as bright linear echoes when sound bounces back to the transducer from the edge of the structure. Volume averaging artifact is due to superimposition of adjacent structure and can make the biopsy needle appear to be within the lesion when it is only near it.
Fig. 38.9
Ultrasound image of the breast shows reverberation artifact at the anterior wall of the cyst.
38.2.2.2 Color Doppler Ultrasound Artifacts
Any movement will be mapped as an area of color. Respiratory motion, often uncontrollable in the elderly, may cause great difficulty in the use of color Doppler ultrasonography. Close cooperation of the patient is needed to use vocal fremitus (talking, humming singing) for distinguishing a tissue mass. This is difficult or impossible to achieve with older patients.
38.2.2.3 Silicone Implant-Related Artifacts
Snowstorm artifacts are caused by extracapsular silicone or by free silicone injection (Fig. 38.10a, b). Artificial increase of thickness and heights of implant are caused by the sound waves traveling slower in silicone. Echogenic noise is produced in the silicone implants due to reverberation artifacts of the invaginated fold of redundant implant shell. New automatic ultrasound machines with improved software offer excellent clarification of the imaging and a reduction of equipment-related artifacts (Rosen and Soo 2001). The biggest sources of ultrasound image artifacts these days are patient related, especially in the elderly.
Fig. 38.10
(a) Ultrasound image of the breast shows snowstorm artifact, caused by extracapsular silicon. (b) Ultrasound image of the breast shows snowstorm artifact caused by free silicone injection
38.2.2.4 Breast Ultrasound Interpretation Pitfalls
Posterior enhancement (increased transmission) is most pronounced in cysts. Malignancies such as invasive ductal carcinoma, ductal carcinoma in situ, metastatic nodule, or lymphoma can also exhibit posterior enhancement. Posterior shadowing (decreased transmission), considered a pronounced sign of malignancy, may also occur in benign lesions such as hyalinized fibroadenoma or focal stromal fibrosis.
Calcifications and the nipple may cause posterior shadowing which can be recognized by correlation with the mammogram and by changing the angle of insonation, respectively. Refractive edge shadowing around the curved edge of the mass can cause apparent mass at the interface of the fat lobule (Fig. 38.11a). Increased pressure and/or change of angle as well as use of color Doppler may resolve the problem (Fig. 38.11b)
Fig. 38.11
(a) Ultrasound image of the breast shows refractive edge shadowing that can make a fat lobule look like a mass. (b) Repeat ultrasound image of the breast shows that changed angle and increased pressure have resolved the problem
38.2.3 Artifacts and Pitfalls in Breast MRI
MRI has come to the forefront as an ancillary tool in breast imaging to improve the detection and characterization of primary and recurrent breast cancers (Ojeda-Fournier et al. 2007). There are a number of artifacts and pitfalls that can potentially limit interpretation of the breast MRI by masking or simulating disease (Morris 2002; Arena et al. 1995).
38.2.3.1 Patient-Related MRI Artifacts
Motion Artifacts
Motion artifacts can be due to physiologic causes (cardiac, respiratory, or pulsation of blood vessels) or to nonphysiologic motion. MRI motion artifacts are a significant problem often seen while imaging elderly patients. Artifacts from blood flow as well as cardiac (Fig. 38.12), respiratory, and patient motion all propagate in the phase-encoding direction, regardless of the direction of the motion. Motion results in blurring of moving tissues and also causes a structured noise pattern known as “ghosting” of brighter moving tissues in the phase-encoding direction (Rausch and Hendrick 2006; Pusey et al. 1986).
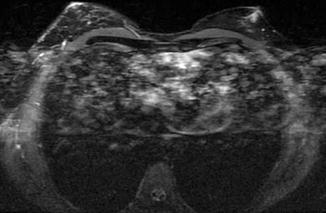
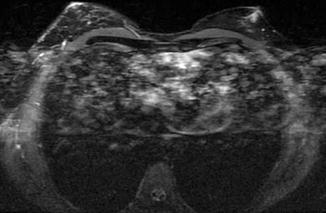
Fig. 38.12
MRI of the breast shows motion artifacts due to cardiac pulsation (Courtesy of Dr. Eugene Ong, National University Hospital)
Ghosting is a form of phase-encoding artifact (Morris 2002; Harvey et al. 2007). To eliminate ghosting, a saturation band can be placed over the moving structure using a standard sequence. Reducing the repetition time may help reduce ghosting so that it is not propagated throughout the entire image, but doing so is often impractical in breast MRI.
Nonphysiologic motion is due to patient movement during the scan and can lead to unsatisfactory images affecting the entire series (Coulthard and Potterton 2000). Claustrophobia and patient anxiety remain the major causes of this artifact, which are more common in the elderly. Patient motion can be reduced by optimizing patient comfort: explain the study to the patient, reassure the patient before the examination, provide appropriate positioning with comfortable arm and head rests, optimize examination time, provide sedatives, use physical restraints only if absolutely necessary, provide earplugs and blankets, and maintain constant communication with the patient throughout the procedure (Rausch and Hendrick 2006).
Metallic Artifacts
Ferromagnetic metals (such as iron, nickel, cobalt) cause severe inhomogeneity in the magnetic field. Metallic objects, including surgical biopsy clips (Fig. 38.13a–c), jewelry, fasteners on clothing, or imaging equipment on or near the patient can disturb the main magnetic field, resulting in a local signal intensity void in the vicinity of the metal, often with a surrounding area of high signal intensity and image distortion (Ojeda-Fournier et al. 2007). If extensive, the artifact could hinder or preclude diagnosis of local recurrence at the lumpectomy site. On the other hand, the signal intensity void from percutaneous biopsy clips may help confirm the biopsy location (Haigh et al. 2000a; Genson et al. 2007; Finder et al. 1998) (Fig. 38.14a–d). A complete history of previous breast interventions, removal of all metallic objects from the patient and the immediate environment, and using titanium metallic markers are some remedial measures to minimize distortion.
Fig. 38.13
(a) Axial T1-weighted MRI of the breast shows metallic artifacts due to surgical clips as an area of signal void. (b, c) Corresponding mammograms (MLO views) show metallic artifacts due to surgical clips (Courtesy of Dr. Eugene Ong, National University Hospital)
Fig. 38.14
(a) Axial and (b) sagittal MRI of the breast show marker clip metallic artifact seen as area of susceptibility. (c, d) Corresponding mammograms (CC and MLO views) show metallic clip artifacts (Courtesy of Dr. Eugene Ong, National University Hospital)
Positioning
Breast MRI can be compromised by breast tissue outside the coil. Breast tissue excluded from the coil may become folded and compressed, resulting in loss of symmetry. Poor visualization of axillary and retroglandular tissue can result from inadequate positioning of the breast in the coil; generally, this happens in the elderly due to sagging skin and glandular involution. Maintenance of bilateral symmetry is ensured by proper positioning of both breasts in the breast coil (Friedman et al. 2006).
At our institution, we often perform MRI for geriatric patients. Artifacts related to improper positioning tend to occur more frequently with elderly women, and hence, we recommend training mammographic technologists in proper positioning of patients and how to manipulate and position the breast within the compression paddles. Do not allow the patient to position herself in the coil. A radiology nurse or patient care assistant can also be trained to properly perform this task. A female staff member should be present during positioning.
Each breast should be centered from superior to inferior within the aperture of the dedicated breast coil. Areas of high signal intensity will result where breast tissue is adjacent to coil elements. The breasts should be pulled away from the chest wall into the two holes in the bilateral breast coil. As little breast tissue as possible should remain above the coil apertures. Improper positioning can result in compression of breast tissue between the chest wall and the center partition of the breast coil (Rausch and Hendrick 2006). Ideally, breast coils of various sizes will be available so that breast size can be matched to coil size. This option improves both patient comfort and image signal-to-noise ratios (Zhuo and Gullapalli 2006).
38.2.3.2 Sequence-Related MRI Artifacts
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree