Assaying Venous Function and Anatomy from the Surgical Perspective
Duplex and color-flow ultrasound have greatly enhanced our ability to investigate and thus to correct abnormalities of the venous system. Additionally, new devices, such as air plethysmography, yield functional and quantitative data providing current and longitudinal assessment of venous function.1 Radiologic determination of reflux based on descending venography has taken on a new meaning. Because of the plethora of “new” tests (Table 43–1), it is important to ask what we really need to know to treat patients optimally.
First and foremost, we need a basic understanding of venous hemodynamics and pathophysiology. Virtually every student will be able to tell you what Homan’s sign is but will know little about how a red blood cell passes from the toes to the heart against gravity and nothing about posterior perforators and ulceration.2 Second, for intelligent management of acute deep venous thrombosis (DVT), we need to know the location of the thrombus and the degree of obstruction. Third, in the case of patients presenting with varicose veins, the varicosities emanate from perforators, from branches of the main saphenous vein, or from dilation and loss of valves throughout the entire saphenous venous system. Finally, in patients with chronic postthrombotic syndrome, we need to know the sites of obstruction, the sites of reflux, the magnitude of obstruction and reflux, and the anatomy of the valves.
 Physical Examination
Physical Examination
Given 100 patients presenting with complaints related to the venous system, 30 could be managed quite successfully without additional expensive testing. In this category are patients who have had a preceding history of iliac DVT and present with mild pain and edema without ulceration. These patients simply need treatment with elastic compression, and testing can be reserved for those who have intractable symptoms. The patient with an isolated anterior thigh or midcalf varix deserves identification by palpation with the patient in the standing position and the veins distended. The examiner determines the site of the most proximal bulging vein and marks it. The patient is placed supine, the leg elevated, and the veins emptied. The examiner now places a finger over the bulging initiation point of reflux and has the patient stand once more. If the cluster of varices remains collapsed, the leading point of valve disruption has been identified. Patients are amazed to see the veins “go away.” It is an easy transition to recommend ligation in the area that is compressed, which would serve the function of eliminating reflux and variceal distention. All other forms of venous disease should be addressed by laboratory testing. The following sections review my personal experience with certain test procedures, emphasizing the aspects most helpful to the surgeon; four cases are presented.
 Case Example 1
Case Example 1
Patient 1 was 8 months pregnant when she was involved in a motor vehicle accident. She sustained injuries to the cartilage of her right knee and to the pelvis. She was treated by rest and crutch walking. Two weeks later, she reported to her obstetrician that her right leg was becoming more swollen and painful. On examination, the leg was edematous; the edema began in the thigh and progressed into the calf and ankle. She had tenderness in the calf musculature. Ultrasound evaluation disclosed a noncompressible common femoral vein, and venous flow in the groin area was not respiratory dependent. The patient was admitted to the hospital, and heparin was administered. On the day after admission, the patient went into labor, and an important decision had to be made. The alternatives included (1) discontinuation of heparin, allowing labor to progress naturally; (2) the same as the first option with the addition of placement of a vena cava filter; or (3) cesarean section followed by heparin with or without a vena cava filter.
Test | Detects |
|---|---|
Physical examination | Varices: size, location Obstructon: edema Dermatitis: ulceration |
Duplex ultrasound | Patency Obstruction Reflux specific vein segment (von Bemmelen) |
Photoplethysmography Air plethysmography4 | Localized skin perfusion Global limb reflux Muscle pump efficiency Obstruction |
Impedance plethysmography Descending venography | Obstruction Reflux: extent Valve anatomy |
Ascending venography | Obstruction |
Discussion
It became important to evaluate the certainty of diagnosis and the extent of disease. To do this, the actual tape of the duplex ultrasonic evaluation was reviewed because duplex ultrasound is technician dependent. On the scans, marked indentation of the skin was seen when pressure was applied by the probe, and yet the underlying vein sustained a rounded contour (see Chapter 24, Fig. 24–12, 1st edition). This established the existence of thrombus in the common femoral vein without question. Additionally, flow tracings disclosed continuous flow in a patent branch of the saphenous vein in the groin area, in sharp contrast to the contralateral extremity, where flow was respiratory dependent. This finding indicated strongly that there was thrombus proximal to the site of interrogation and that blood was circulating from the leg back to the heart through collaterals; normally, flow through main lower-extremity venous channels diminishes when the diaphragm lowers.
Physical examination confirmed the findings of extensive DVT. Because of the extent of thrombus, it was quite evident that anticoagulation therapy should be continued to preserve venous function. Surgical thrombectomy and caval filter placement were contemplated. Because the swelling had been apparent for almost a week before this patient was admitted to the hospital, however, we reasoned that the clot was likely to be adherent and stable and that the time spent placing a filter would be better used by performing an expeditious cesarian section. This plan of therapy resulted in a healthy infant and an asymptomatic leg 5 days later. At the time of discharge, the common femoral vein was partially compressible, and only low-grade obstruction was found by impedance plethysmography (IPG).
Weeks later, the patient complained of increased swelling of the leg, and her prothrombin time, designed to be 2 to 2.5 times control, was found to be 1.5 times control. IPG was done again, and significantly greater obstruction was found than prior to her last discharge. A diagnosis of progression of DVT was made, and the warfarin dose was increased to sustain more adequate levels of anticoagulation. At 3-month follow-up, the leg appeared normal, but the patient had a painful, swollen knee as a consequence of the accident. IPG disclosed outflow to be within normal range, although less than on the contralateral extremity. It was elected to defer arthroscopic surgery for her torn knee cartilage for an additional month. Testing at that time disclosed further improvement, allowing discontinuation of the anticoagulation and removal of the cartilage arthroscopically. She remained asymptomatic at 1 year.
 Case Example 2
Case Example 2
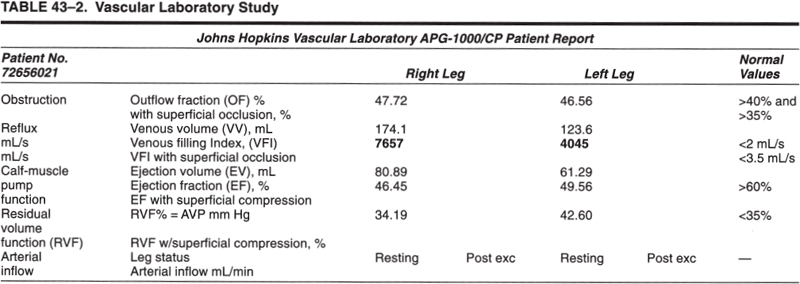
Patient 2 presented at age 46 with large varicosities that developed after pregnancy, worse in the right than the left leg. She complained not only that her veins were unsightly but also that she had achiness in her calf together with some swelling of her right ankle. The results of air plethysmographic (APG) studies are shown in Table 43–2. The patient had a great deal of reflux in the right leg, less in the left leg. In the right leg, she had a good muscle pump as the residual volume fraction, defined as the volume of blood in the calf after calf exercise divided by the volume of blood drained from the leg down to leg up position, was really quite normal.
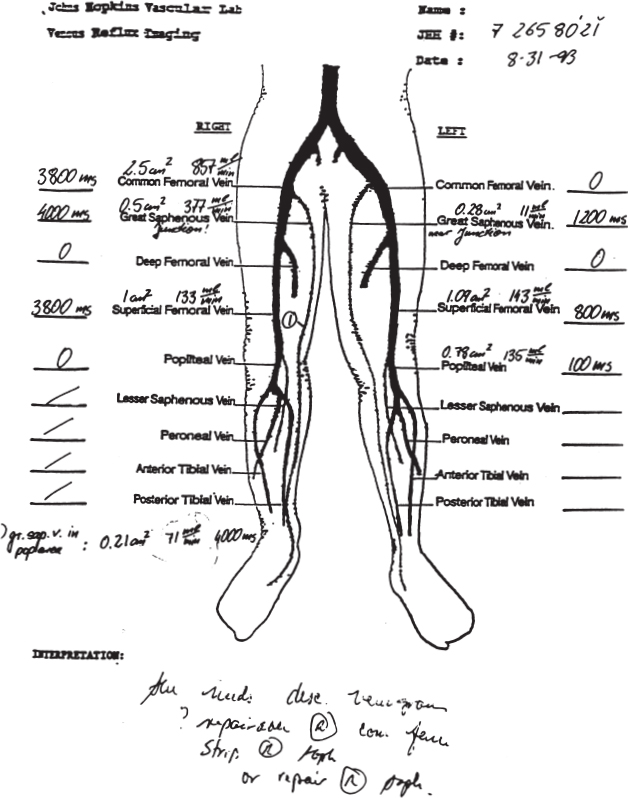
The von Bemmelen test was used to define the principal areas of reflux by duplex.3 In this test, a large blood pressure cuff capable of rapid deflation is placed around the thigh and inflated to pressures of 80. Rapid deflation then provides a standard challenge for blood to run backward promoting reflux. The results are shown in Figure 43–1 and quantitated in the diagram, which documented gross incompetency of the right common femoral and greater saphenous vein at the saphenofemoral junction.4 On the left side, the greater saphenous vein was leaky distal to the saphenofemoral junction but intact over the saphenofemoral junction.