Fig. 1
Lateral view of a barium swallow shows a metallic bolt in the trachea of a 2-year-old boy
Food particles and organic materials constitute the vast majority of aspirated objects (Blazer et al. 1980; Keith et al. 1980; Svensson 1985; Mantel and Butenandt 1986; Piepsz 1988; Mu et al. 1990; Linegar et al. 1992; Black et al. 1994; Baharloo et al. 1999; Metrangelo et al. 1999; Diaz et al. 2000; Siddiqui et al. 2000; Brkic et al. 2001; Lima and Fischer 2002; Ayed et al. 2003; Roda et al. 2008; Ugrinovic et al. 2009; Chik et al. 2009; de Sousa et al. 2009; Albirmawy and Elsheikh 2011; Huankang et al. 2012). The nature of the aspirated material varies according to geographic and sociologic circumstances. Peanuts are the most common aspirated particles in North America, Europe, India, and South Africa (Teixidor de Otto et al. 1980; Mantel and Butenandt 1986; Mu et al. 1990; Linegar et al. 1992; Diaz et al. 2000; Sehgal et al. 2002; Shivakumar et al. 2003), whereas earthnuts, grains, sunflower seeds, and watermelon seeds are more common in the South America, Middle East, and eastern Asia (Farkash et al. 1982; Elhassani 1988; Oguz et al. 2000; Pasaoglu et al. 1991; Cataneo et al. 2008; Zhijun et al. 2008; Chik et al. 2009; Saki et al. 2009; Oncel et al. 2012; Gang et al. 2012; Pan et al. 2012). Due to their high protein concentration, most organic foreign bodies absorb water from bronchial secretions and tend to increase in size. Candies have been reported to have a similar effect due to their high sugar concentration (Mearns et al. 1975). Oil, salt, and vegetable proteins in cooked food irritate the mucosa, causing edema and formation of granulation tissue with resultant narrowing of the bronchial lumen. Hence, an organic foreign body can grow to be larger than the original diameter of the bronchus, and what was initially a partial obstruction can progress to become a complete obstruction (Fig. 2a) (Aytac et al. 1977; Cataneo et al. 1997).
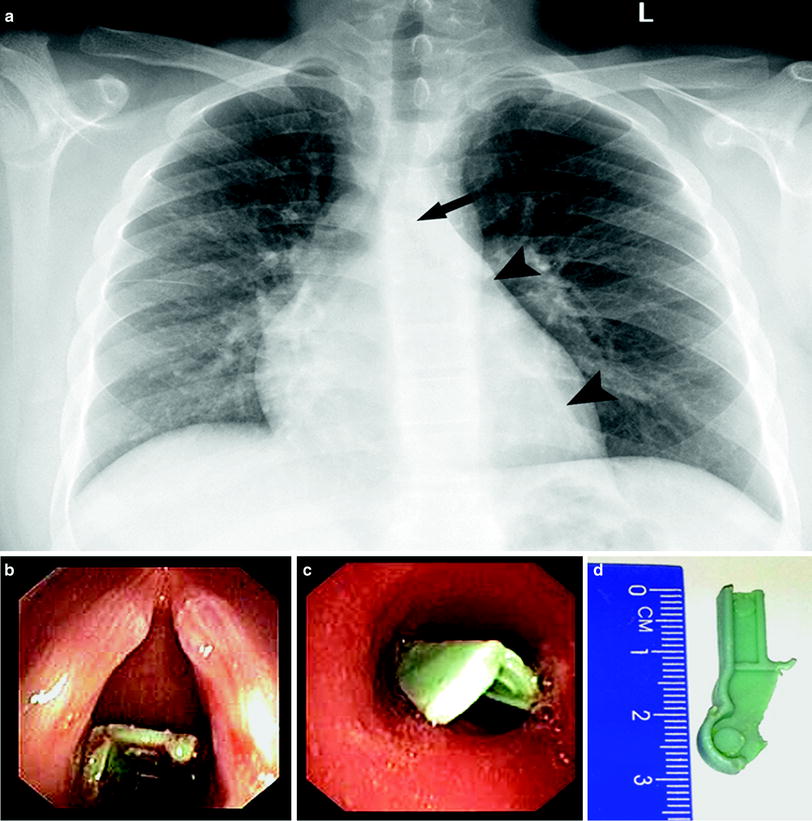
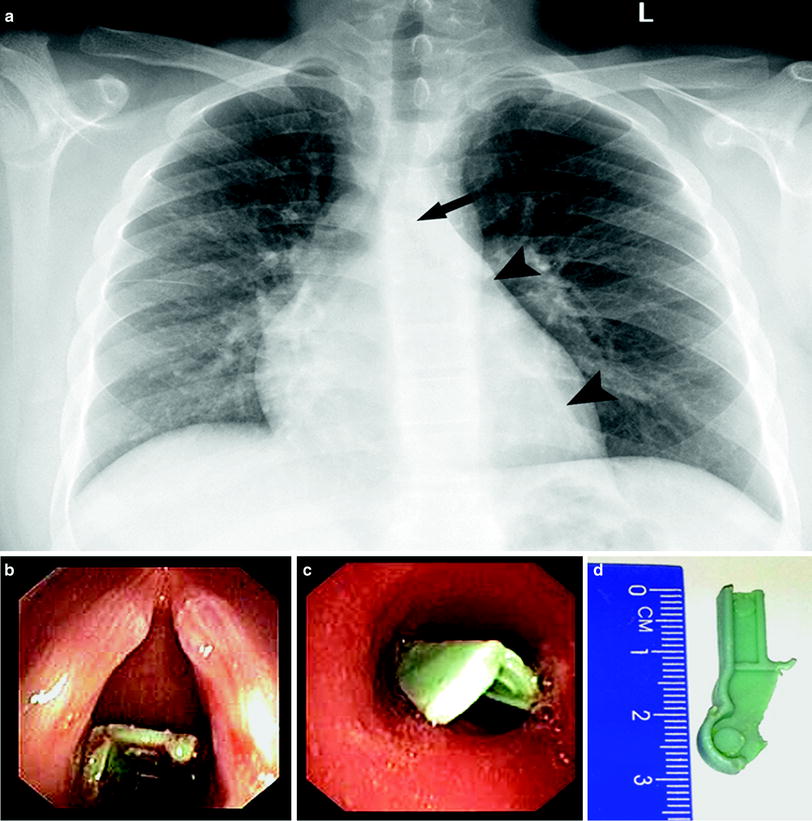
Fig. 2
Posteroanterior chest radiograph demonstrating “absance” of the left main bronchus (“interrupted bronchus” sign, arrow, (a)) in a 13-year-old boy who held a plastic piece of a toy between his lips while playing a computer game. Note resultant left lower lobe atelectasis (arrowheads) as well as left upper lobe hyperinflation. At bronchoscopy, the plastic was initialy seen under the vocal cords (b), then migrated to the orifice of the left lower bronchus (c). Note the size of the extracted piece (d)
Grass inhalation is not uncommon and has some unique characteristics. The literature contains reports describing aspiration of several types of grass heads, all with the same structure of side spurs along the main stem. When inhaled stump-first, the spikes carry the grass heads distally into the bronchial tree and lung parenchyma. Being resistant to organic decay, they can remain in the chest for a long time and can cause unusual infections, as well as other complications (Spencer et al. 1981; Maayan et al. 1993; Dindar et al. 1994; Basok et al. 1997; Newson et al. 1998; Ammari et al. 2000).
Nonorganic objects comprise 5–20 % of the foreign bodies aspirated by children (Farkash et al. 1982; Mortellaro et al. 2013). Of these, coins are the most common (Reilly and Walter 1992), followed by plastic toy pieces and sharp objects such as pencils and pull-tabs from aluminum cans (Rogers and Igini 1975; Burrington 1976; Blazer et al. 1980; Strickland et al. 1987; Applegate et al. 2001). Inert foreign bodies have little effect on the bronchial mucosa and, unless they cause an obstruction by virtue of their size, can remain undiagnosed for long periods of time (Adegboye et al. 2003). Aspiration of pacifiers is not uncommon among toddlers (Jain et al. 1986; Barrett and Debelle 1995). Partially inflated balloons and Nylon bags are particularly hazardous (Abdel-Rahman 2000; Anas and Perkin 1983).
A tooth can be aspirated by a sleeping child at the age of permanent tooth eruption. This happened to a 10-year-old girl who had a loose deciduous tooth when she fell asleep at night. When she woke up the next morning the tooth had disappeared from her mouth. The episode was forgotten; 10 days later she developed symptoms of left lower lobe pneumonia, with no response to antibiotic therapy over several months. When she was admitted to the hospital, the missing tooth was evident in the left lower lobe bronchus on a chest radiograph, with atelectasis of most of the basal segments (Fig. 3). The tooth was removed by bronchoscopy; 2 months later residual bronchiectatic changes could still be seen in the left lower lobe.
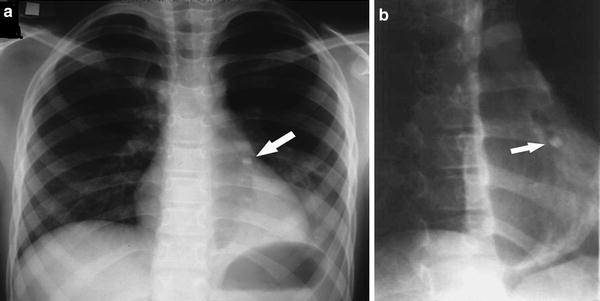
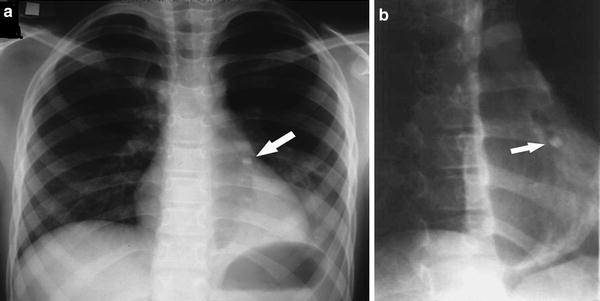
Fig. 3
Posteroanterior chest radiograph (a) of a 10-year-old girl and an oblique view (b) (obtained at fluoroscopy): a deciduous tooth (arrow) is present in the left lower lobe bronchus obstructing some of the basal segments and causing volume loss. Bronchiectasis, evident in the left lower lobe, is better demonstrated by the oblique projection
Aspiration of tooth, dental fillings, crowns, or dental treatment equipment can also occur during dental treatment (Steelman et al. 1997), following minor trauma (Holan and Ram 2000), during anesthesia, and intubation or resuscitation procedures, especially in victims of road traffic accidents, and following tracheostomy canula replacement in debilitated patients.
Aspiration of gravel, dirt, or sand can happen during a traffic accident, in a cave-in or accidental burial, in a near-drowning event, or while playing in sand (Bergeson et al. 1978; Wales et al. 1983; Avital et al. 1989; Choy and Idowu 1996; Glinjongol et al. 2004; Arun Babu and Ananthakrishnan 2013). Airway obstruction has also been reported as a result of nonaccidental trauma, when forcible introduction of a foreign body caused tracheal obstruction, with a resultant death reported in one case (Barrett and Debelle 1995; Nolte 1993). Aspiration of headscarf needles (Turban pins) has been reported in young girls and adolescents in Islamic populations (Ucan et al. 1996; Kaptanoglu et al. 1999; Murthy et al. 2001; Kaptanoglu et al. 2007; Al-Sarraf et al. 2009; Hamad et al. 2010; Albirmawy and Elsheikh 2011; Ilan et al. 2012). Aspiration of other sharp metallic objects occurs more commonly among adolescents (Ludemann and Riding 2007; Walz et al. 2013). Such an aspirated pin, an office thumbtack, or a sewing needle can get stuck in the bronchial wall in one or both ends, a condition in which simple bronchoscopic extraction is not possible. In such cases, the use of additional, advanced endoscopic techniques is necessary in order to enable a successful bronchoscopic extraction and obviate the need for possible thoracotomy (Jabbardarjani et al. 2010).
3 Mechanisms of Airway Obstruction
A foreign body in the respiratory tract does not necessarily cause an obstruction, i.e., air can be inhaled and exhaled freely around the foreign body. This is known as a “two-way valve mechanism,” and occurs when the foreign body, which is usually located in the trachea, is small in relation to the airway. A foreign body can cause complete obstruction when air entry is blocked during inspiration and the air cannot be exhaled during expiration. This is called a “no-way valve mechanism.” A foreign body can allow air entry during inspiration but prevent the exit of air during expiration in a “one-way valve mechanism.” This mechanism is explained by the larger diameter of the airway during inspiration due to higher intrathoracic negative pressure, and the smaller diameter during expiration.
Chest X-rays performed in cases of a nonobstructive tracheal or bronchial foreign body demonstrate uniform aeration bilaterally both in inspiration and expiration. In partial obstruction due to the one-way valve mechanism, the chest radiograph usually demonstrates air-trapping. Inspiratory films are often normal, and the air-trapping may become evident only in an expiratory study. In cases of complete airway obstruction (most commonly at the level of a bronchus), we often notice a combination of air-trapping in the non-dependent lobes with atelectasis of the dependent lobes. This is due to mucus plugging and the accumulation of secretions in the bronchial tree of the dependent segments (Figs. 2, 4, 5).
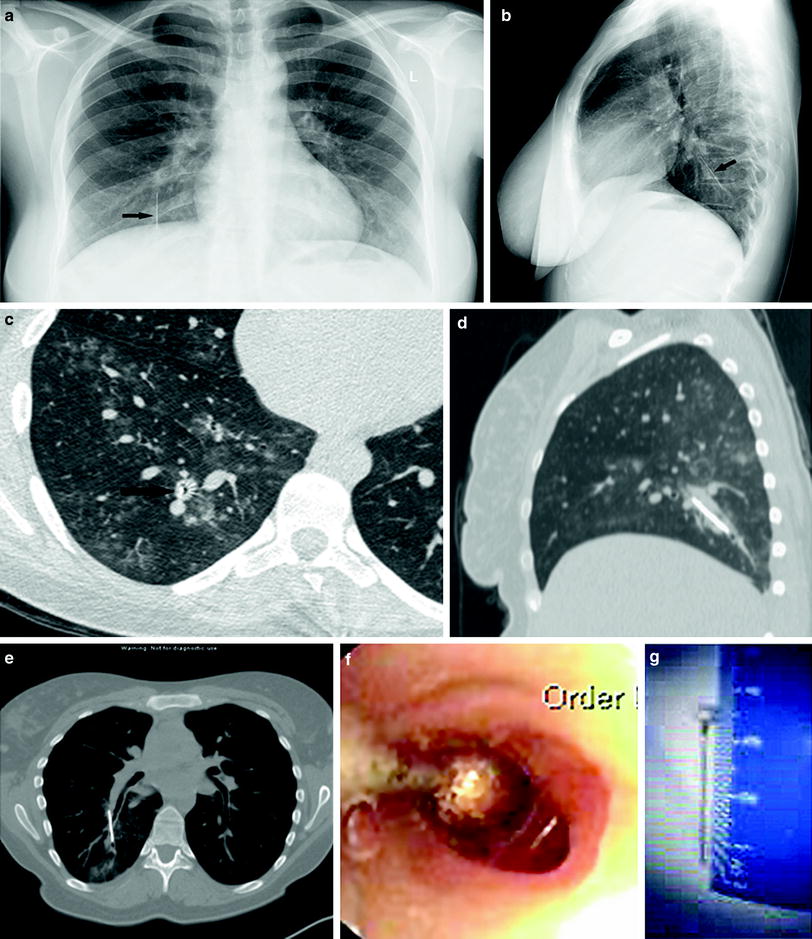
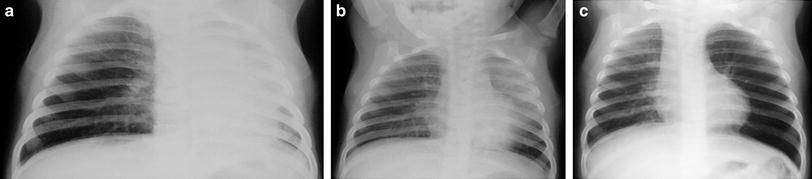
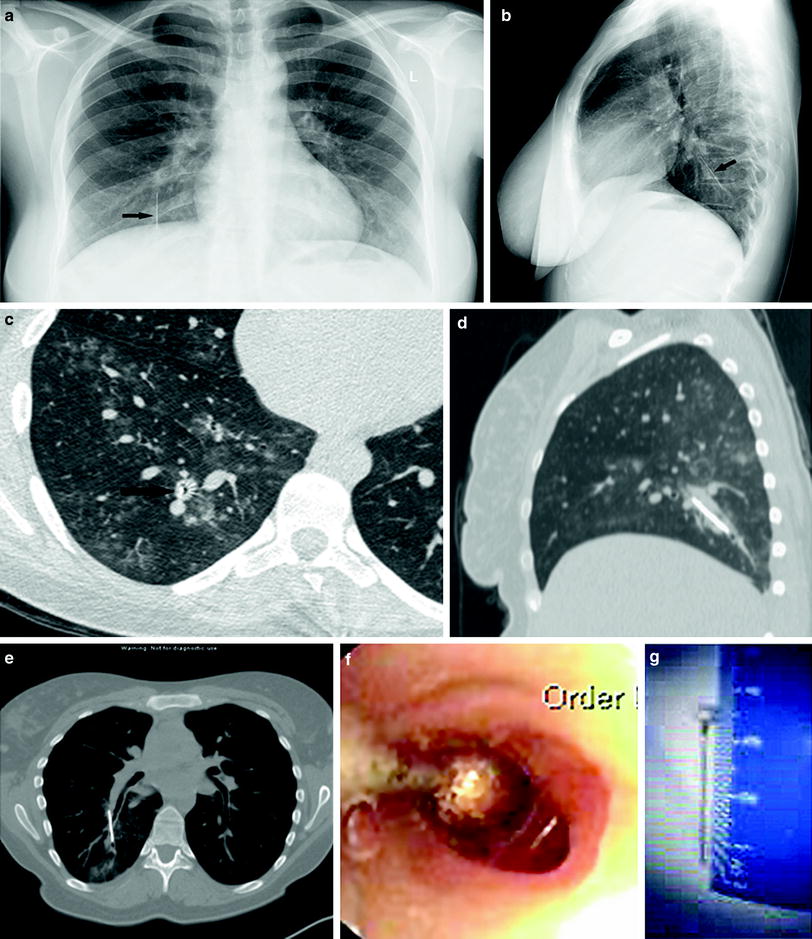
Fig. 4
Posteroanterior (a) and lateral (b) chest radiograph demonstrating a hairpin aspirated into the right lower lobe (arrow). Axial (c), semicoronal (d), and sagital (e) reformats of a CT scan demonstrated the oblique position of the pin with its end protruding through the bronchial wall, as demostrated at bronchoscopy (f). Extraction of the pin (g) was accomplished without further bronchial wall destruction only after it was heated and bent
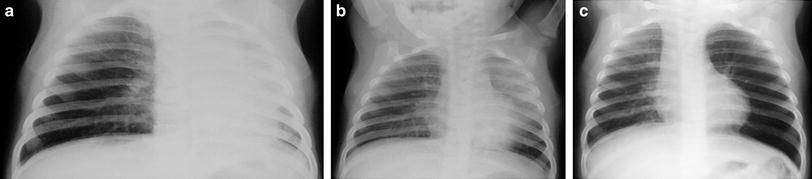
Fig. 5
A 10-month-old girl with cough, low fever, and mild tachypnea for 4 days. Initial chest radiograph was normal. Follow-up chest radiographs 24 h later, on day 5 (a), showed collapsed left lung. 24 h later, on day 6 (b), there was left upper lobe collapse; 48 h later, on day 8 (c), emphysema of the left lung was seen. Bronchoscopy found two foreign bodies: a wood splinter and a piece of plastic
The incidence of right and left bronchial foreign bodies is almost equal in infants and young children (Mu et al. 1990; Black et al. 1994; Burton et al. 1996; Cataneo et al. 1997; Senkaya et al. 1997; Metrangelo et al. 1999; Oguz et al. 2000; Van Looij et al. 2003; Ayed et al. 2003; Pinto et al. 2006; Zhijun et al. 2008; Cohen et al. 2009; Rodriguez et al. 2013), as opposed to predominance of the right bronchial tree in older children, adolescents, and adults (Baharloo et al. 1999; Fraga Ade et al. 2008; Roda et al. 2008; Kitcher 2009; de Sousa et al. 2009; Tang et al. 2009; Saki et al. 2009; Falase et al. 2013; Sidell et al. 2013). These differences can partly be explained by the almost symmetrical tracheobronchial angle in younger children (Cleveland 1979) and by the position of the carina that is more commonly seen left to the midline (Tahir et al. 2009). Migration of a small foreign body within the airways during different phases of the respiratory cycle, secondary to alterations of posture or following cough is rare, but does occur, and can change the clinical and imaging findings (Figs. 5, 6) (Metrangelo et al. 1999). The authors witnessed a case in which a foreign body that was located in the right main bronchus migrated to the right upper lobe bronchus when the father of the child turned her upside down in an attempt to expel the foreign body from the airway. Since in those days only rigid bronchoscopy was available, the foreign body could not be endoscopically removed and the patient required thoracotomy and lobectomy. Migration of a foreign body can also occur during bronchoscopy, if the foreign body detaches from the bronchoscopic forceps on its way out or if it is partially lodged into the tracheal or bronchial wall and has to be manipulated prior to its extraction.
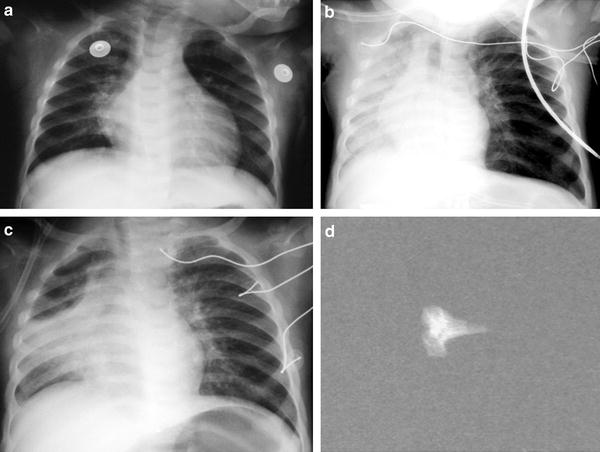
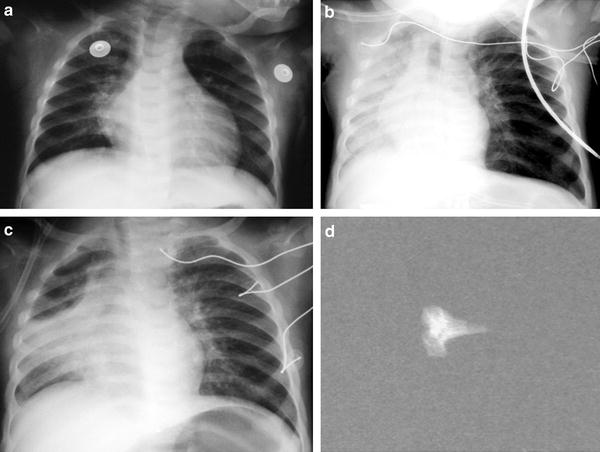
Fig. 6
A 10-month-old boy with rickets aspirated a chicken bone. Initial chest radiograph (a) was normal (the chicken bone was missed). Follow-up chest radiographs 24 h (b) and 48 h (c) later showed progressive collapse of the right lung. A chicken bone (d) was removed from the right main bronchus on bronchoscopy
4 Clinical Findings and Differential Diagnosis
The clinical manifestations of aspirated foreign bodies vary according to the location and degree of obstruction.
Laryngeal and subglottic foreign bodies make up about 5 % of foreign bodies in the airways (Mantel and Butenandt 1986; Esclamado and Richardson 1987; Cohen et al. 1993; Black et al. 1994; Baharloo et al. 1999). When large enough, their presence in the major airway causes dyspnea, and when located adjacent to the vocal cords they may induce hoarseness, sudden loss of voice, and inspiratory stridor (Blazer et al. 1980; Hanukoglu et al. 1986; Laks and Barzilay 1988). Cyanosis may occur secondary to laryngeal spasm (Halvorson et al. 1996; Baharloo et al. 1999; Ciftci et al. 2003). Similar symptoms can be induced by other processes such as a laryngeal web (Chen et al. 1998), viral or bacterial croup, epiglottitis, papilloma or hemangioma, angioneurotic edema, or hypocalcemic tetany (Grad and Taussig 1990; Ibrahimov et al. 2013). Laryngeal or tracheal hirudiniasis following leech infestation while drinking infected stream water can cause the same symptoms due to mechanical obstruction. In addition, the combination of the grasp of the mucosa by the leech cutting plates and secretion of an anticoagulant causes hemorrhage that can result in prolonged hemoptysis and anemia (Mohammad et al. 2002; Yazici et al. 2012).
Tracheal foreign bodies constitute 4–13 % of foreign bodies in the airways (Mu et al. 1990, 1991; Black et al. 1994; Burton et al. 1996; Metrangelo et al. 1999) (Figs. 1, 7). In one series, they represented 23 % of the cases with early diagnosis and 7 % of the cases with late diagnosis (Oguz et al. 2000). In most patients there is a history of choking and dyspnea, yet they tend to be diagnosed later than bronchial foreign bodies, probably because they cause less severe respiratory symptoms (Esclamado and Richardson 1987). Inspiratory or biphasic stridor and wheeze can also be caused by tracheomalacia or external compression on the trachea by a vascular structure. Vascular rings usually cause a focal narrowing, but can have a hazardous effect by blocking a small foreign body that would have otherwise be aspirated into a more distal bronchus, thus turning a partial, distal bronchial obstruction to a potentially fatal tracheal obstruction. Other causes of external compression include bronchogenic cysts, enlarged lymph nodes (secondary to viral or bacterial infection or due to tuberculosis), mediastinal tumors (e.g., lymphoma), or an esophageal foreign body (Fig. 8). A hollow foreign body located in the larynx or trachea can be almost asymptomatic and thus presents a unique diagnostic challenge (Jain et al. 2013).
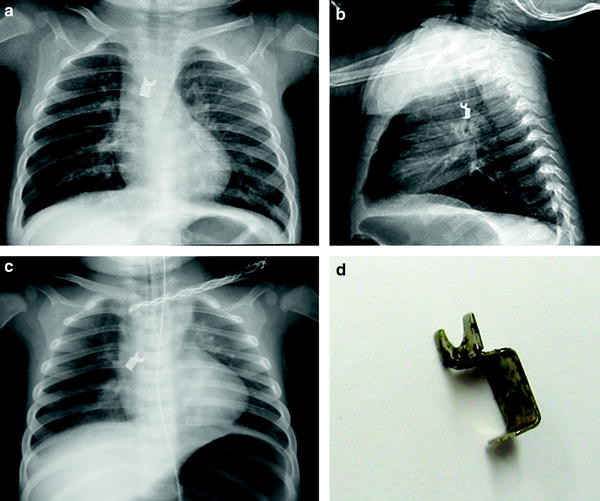
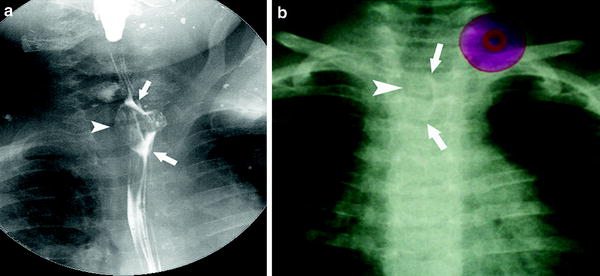
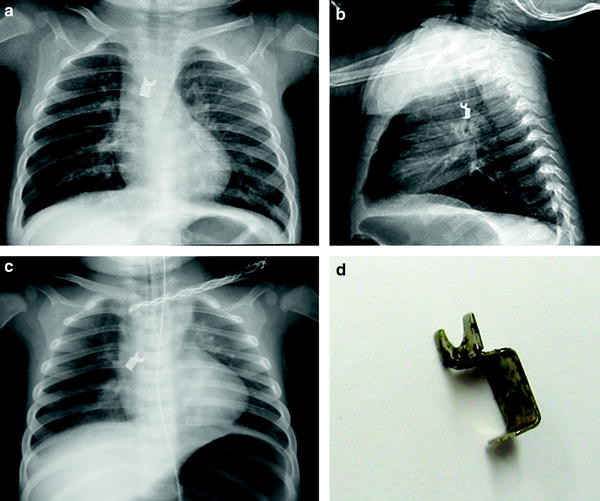
Fig. 7
A broken piece of a metal zipper partially blocking the distal trachea of a 2.5-year-old girl causing bilateral hyperinflation as seen in an AP (a) and lateral (b) chest radiograph. During rigid bronchoscopy, the foreign body got stuck between the vocal cords and the child could neither be ventilated nor intubated. Bradycardia and decrease in oxygen saturation necessitated resuscitation and emergency tracheostomy. The foreign body was pushed down to the right bronchus (c). Following completion of tracheostomy, the metal piece (d) was pulled up to the level of the cords by flexible bronchoscopy and dislodged using surgical forceps
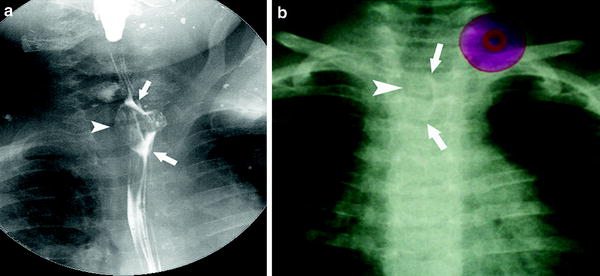
Fig. 8
A rubber-made vaccum hanger was swollen by a 2-year-old boy causing stridor and salivation. Oblique view of a barium swallow study (a) demonstrated the rubber hanger in the proximal esophagus (arrows), causing marked posterior compression and narrowing of the trachea (arrowhead). Magnified AP chest radiograph (b) demonstrated the rubber hanger in the upper esophagus, with a similar one illustrated on the top left corner of the film
Bronchial foreign bodies The majority of aspirated foreign bodies (67–85 %) are found in the main bronchi (Blazer et al. 1980; Mantel and Butenandt 1986). A history of sudden choking is the most important clue for diagnosis (Esclamado and Richardson 1987; Silva et al. 1998; Zerella et al. 1998; Metrangelo et al. 1999; Oguz et al. 2000; Ciftci et al. 2003). Such a history, however, was documented in only about one third of the cases in one series (Oguz et al. 2000). The classical triad of a choking episode, cough, and wheeze was found in over 90 % of the patients in another series (Blazer et al. 1980). Hemoptysis can be a presenting symptom (even in cases of a blunt foreign body) (Scully et al. 1983; Maayan et al. 1993; Fabian and Smitheringale 1996; Cataneo et al. 1997; Zuniga et al. 2000; Abellan Martinez et al. 2000; Mohammad et al. 2002). Physical examination will reveal unequal chest expansion during inspiration, as well as decreased breath sounds over the obstructed lung (Laks and Barzilay 1988; Oguz et al. 2000; Orji and Akpeh 2010; Roda et al. 2008; Huankang et al. 2012). Occasionally, a slapping sound of a loose foreign body can be heard (Felman 1982).
In cases of delayed diagnosis, pneumonia is a common presentation. The presence of an aspirated foreign body should be suspected in any patient with unexplained chronic pulmonary symptoms. Foreign body aspiration, however, is by no means the most common cause of recurrent pneumonia. Recurrent or persistent pneumonia can also result from bacterial infections, gastroesophageal reflux, impaired clearance of secretions from the tracheobronchial tree as in asthma, ciliary dysmotility (primary ciliary dyskinesia), cystic fibrosis, infected bronchiectasis or secondary to an immune deficiency (Kumar et al. 2009). Tumors of the tracheobronchial tree are uncommon in children, but, when present, may cause a varying degree of airway obstruction. Foreign bodies can sometimes coexist with other medical conditions that elicit similar symptoms such as allergic asthma, recurrent infections, or acute bronchiolitis (Ezer et al. 2011). Persistent symptoms and lack of improvement despite appropriate medical therapy should raise suspicion for the presence of a foreign body.
Esophageal foreign bodies can mimic foreign bodies in any location of the airway due to external compression of the larynx, trachea, or bronchi (Fig. 8). Such compression can cause laryngeal or tracheal spasm, resulting in respiratory distress, stridor, or wheeze (Smith et al. 1974). In infants operated for congenital esophageal atresia, the combination of esophageal dilatation proximal to a stenotic anastomosis and an inherent tracheomalacia can result in severe tracheal narrowing, stridor, and a respiratory arrest. A tracheoesophageal fistula may develop as a result of a decubitus ulcer caused by an esophageal foreign body of long-standing duration (Szold et al. 1991; Li et al. 2009).
Nasal foreign bodies, when present for a long time, usually cause swelling of the nostrils or nasal discharge that may be foul smelling. They can ulcerate and damage the nasal septum, dislodge into the nasopharynx, and seldom can be aspirated into the tracheobronchial tree (Cohen et al. 1993; Fini-Storchi and Ninu 1996; Qureshi et al. 2009).
5 Imaging Techniques
Chest Radiograph. The plain chest X-ray remains the initial study in the evaluation of a suspected aspirated foreign body. Abnormal findings are found in 40–88 % of chest X-rays in children with proven foreign bodies (Laks and Barzilay 1988; Mu et al. 1990; Black et al. 1994; Oguz et al. 2000; Cataneo et al. 2008; Fraga Ade et al. 2008; Sidell et al. 2013). These rates increase when using inspiratory–expiratory techniques (Black et al. 1984, 1994; Losek 1990). Opaque foreign bodies are easily identified, but most are radiolucent (Figs. 1, 2, 11).
In cases of a nonopaque foreign body, inspiratory and expiratory films can provide important information. Comparison of the two hemithoraces is mandatory. The inspiratory film is often normal or near normal, while the expiratory film shows obvious air-trapping. The obstructed lung is of larger volume and more radiolucent. The decrease in ventilation of the obstructed lobe causes an increase in pCO2. The higher pCO2 leads to arterial vasoconstriction and therefore to reduced pulmonary perfusion. Thus, the vessels in the obstructed region become narrow and sparse. This finding, characteristic of obstructive emphysema, can be seen on both plain films and Computed Tomography (CT). There is usually a mediastinal shift to the opposite side in expiration, as well as a lower ipsilateral hemi diaphragm (Figs. 9, 10).
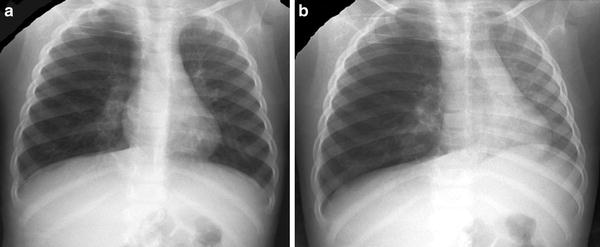

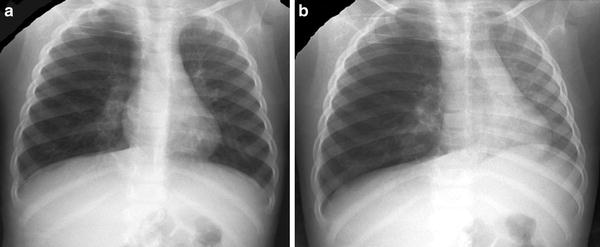
Fig. 9
Anteroposterior chest fluoroscopy at inspirium (a) and expirium (b) demonstrating minimal change in volume and lucency of the hyperinflated, obstructed right lung as opposed to volume loss and change in opacity of the deflated left lung in expiration (b). Note the arched and more superior position of the left hemidiaphragm and the mediastinal shift toward the unobstructed left lung at expiration

Fig. 10
A 20-month-old boy had a choking episode. Initial chest radiograph (a) demonstrated obstructive emphysema of the right lung; bronchoscopy failed to reveal a foreign body. Lung scan (b) showed lack of perfusion to the right lung. Chest CT demonstrated obstructive emphysema of the right lung with contralateral mediastinal shift (c), as well as a foreign body in the right main bronchus (d). Repeat bronchoscopy identified a lentil
In young children, whose cooperation is not always optimal, two lateral decubitus films, one on each side, can replace the inspiratory–expiratory films (Capitanio and Kirkpatrick 1972). An unobstructed, dependent lung shows smaller volume and crowded vessels as a result of gravitational forces on the abdominal and mediastinal organs. In cases of partial obstruction, the dependent lung does not deflate as expected. The relative hyperinflation of the dependent lung thus indicates the presence of partial bronchial obstruction.
Alternatively, expiratory films can be obtained in non-cooperative patients by applying manual pressure on the upper abdomen using a lead glove during the examination (Wesenberg and Blumhagen 1979). In infants this can also be done by inflating a blood pressure cuff, wrapped around the abdomen. Careful monitoring must be performed to ascertain that at no time the pressure in the cuff exceeds the child’s systolic blood pressure. Oblique projections enable better visualization of the trachea and main bronchi, and may demonstrate an otherwise “hidden” foreign body or discontinuation of the air column, depicted as an “absent segment” of the airway (Figs. 2, 3).
The High kilo-voltage (kV) Copper Filter Technique increases the visibility of the major airways and of nonopaque foreign bodies (Fig. 11). This technique combines the use of high kV with filters that absorb most of the low energy photons. As a result, the contrast between soft tissue and bone is reduced and the contrast between air and all other tissues is increased. Thus, the airway and its contents are sharply delineated over the background of the other tissues. Various filters have been used; however, the combination of 0.4 mm of tin, 0.5 mm of copper, and 0.75 mm of aluminum is probably the most useful. The use of this technique enables improved visualization of the major airways with reduced radiation dose (Joseph et al. 1976).


Fig. 11
High kV copper filter technique of the tracheobronchial tree of a 15-month-old girl. A nonopaque foreign body (arrows) surrounded by air is seen at the carina and in the right main bronchus. The inspiration and expiration films did not reveal air trapping or any other pulmonary pathology
The sensitivity, specificity, and accuracy of chest radiographs for the detection and diagnosis of aspirated foreign bodies have been shown to be low when compared to bronchoscopy or to clinical signs in several retrospective studies (Svedstrom et al. 1989; Hoeve and Rombout 1992; Hoeve et al. 1993; Barrios Fontoba et al. 1997; Silva et al. 1998; Zerella et al. 1998; Sehgal et al. 2002; Ayed et al. 2003; Pinto et al. 2006; Cataneo et al. 2008; Kiyan et al. 2009; Zaupa et al. 2009; Hitter et al. 2011). In some series, upto 50 % of chest X-rays obtained in children with proven foreign bodies were found to be normal when filmed in the early period (within 3 days) following aspiration; however, expiratory radiographs were not routinely obtained in these studies (Zerella et al. 1998; Oncel et al. 2012). Expiratory films have a high diagnostic value, but without clinical suspicion of foreign body aspiration, they will not be routinely performed. Therefore, it is mandatory that the clinician provide this sort of information to the radiologist in charge of the exam. Chest X-rays can also be normal in cases of a radiolucent tracheal foreign body that is not large enough to cause obstruction (Chang and Pereira 2013) and in cases of bilateral bronchial foreign bodies (Wiseman 1984; Musemeche and Kosloske 1986; Laks and Barzilay 1988).
Fluoroscopy can still raise a significant contribution to the investigation of foreign body aspiration. The proponents of this modality advocate its use because it is widely available, easy to use, and rapidly diagnostic in up to 90 % of cases of a bronchial foreign body (Blazer et al. 1980; Zerella et al. 1998). In our practice, fluoroscopy is seldom used. Nevertheless, the radiologist can optimally visualize the airways and detect obstruction or the presence of an opaque foreign body with fluoroscopy (Fig. 3b), especially if a copper filter is used adjacent to the X-ray tube or close to the patient (W.E. Berdon, personal communication). Mediastinal shift toward the obstructed side during inspiration and towards the contralateral side during expiration is easily recognized (Fig. 9) (Theander 1970; Laks and Barzilay 1988; Mu et al. 1990). Unequal descent or ascent of the hemidiaphragms on inspiration and expiration can be seen and is more easily noticed in crying babies and in older children when requested to sniff rapidly. Diminished excursions of the diaphragmatic leaflets are invariably seen on the affected side, either with hyperinflation (in partial obstruction) or with volume loss (in complete obstruction) (Theander 1970). Use of any technique for assisted expiration, as described earlier, can facilitate demonstration of air-trapping. Digital subtraction fluoroscopy has been described as a sensitive method for the demonstration of tracheal and bronchial narrowing secondary to the presence of a radiolucent aspirated foreign body (Ikeda et al. 2001). The use of “last image hold” and “last fluoroscopy hold” applications currently installed in most modern fluoroscopy machines enables quick exclusion or confirmation of suspected bronchial obstruction with minimal radiation exposure.
Computed tomography (CT), due to its high contrast resolution, enables demonstration of foreign bodies that are frequently not visible on the chest X-ray. CT is usually utilized as a part of work-up for unclear cases of persistent, nonresolving respiratory symptoms, for which foreign body aspiration can be one of the reasons. When initial imaging studies or bronchoscopy are negative, CT may reveal the presence and location of a previously undiagnosed foreign body (Berger et al. 1980; Bertolani et al. 1999). CT is a very sensitive modality for demonstrating small dense objects, such as thin fish or chicken bones, that may not be detected on plain films (Braverman et al. 1993; Mignon et al. 1997; Bai et al. 2011; Hitter et al. 2011; Sattar et al. 2011; Manach et al. 2013).
CT is also an efficient tool for the demonstration of small plastic toy particles such as LEGO pieces (Applegate et al. 2001) or rubber products. The presence and location of an intraluminal lesion can easily be detected and multiple intrabronchial findings can at times be identified (Figs. 4, 10, 12, 13), as well as the “interrupted bronchus” sign. Intravenous contrast administration can enhance discrimination between an intraluminal foreign body and other endobronchial, bronchial wall, or extrinsic findings, such as a hemangioma or lymph nodes. By varying window width and level, one can see not only the foreign body, but also the reaction of the tissue around and distal to it. One can also assess the presence and extent of complications such as air-trapping, atelectasis, pneumonia, alveolar hemorrhage, empyema, bronchiectasis, or chest wall involvement (Figs. 4, 10, 12, 14) (Haliloglu et al. 2003; Kosucu et al. 2004; Adaletli et al. 2007). Air-trapping is well demonstrated by decubitus scans (Fig. 15) (Garcia-Pena et al. 1999; Lucaya et al. 2000; Choi et al. 2002). Scanning in the semicoronal plane had been used to demonstrate accurate localization of the obstructing foreign body (Figs. 12, 13) (Bar-Ziv and Solomon 1990). However, with current helical, multidetector scanners using volumetric acquisition of data, a high pitch and a short scanning time, accurate multiplanar reconstructions can be obtained, thereby replacing the semicoronal scans.
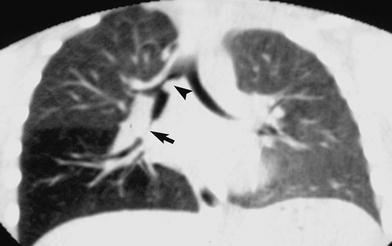
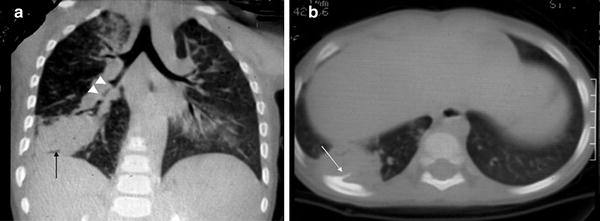
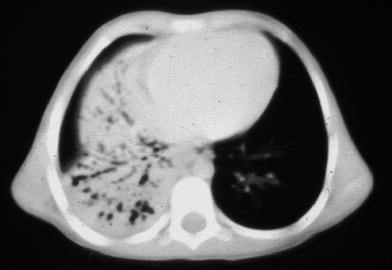

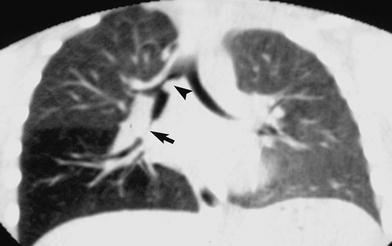
Fig. 12
A semicoronal chest CT (lung settings) of a 2-year-old boy, obtained in expiration. Soft tissue density is demonstrated in the bronchus intermedius causing a partial obstruction (arrow). This is the equivalent of the “absent segment” sign that results from the presence of an obstructing foreign body and inflammatory changes in the adjacent bronchial wall. Note also the obvious air trapping in the right lower lobe as compared to the normal-sized right upper lobe and left lung. Another partially obstructing foreign body is seen adjacent to the medial wall of the right main bronchus (arrowhead)
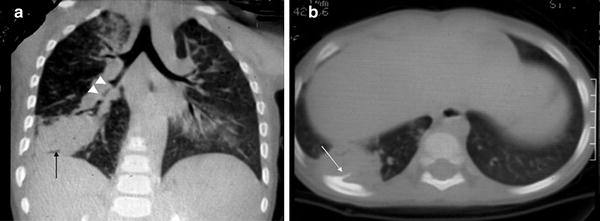
Fig. 13
A 3-year-old boy aspirated a branch of Timothy grass. Semicoronal (a) and axial (b) chest CT demonstrate narrowing and irregularity of the bronchus intermedius (arrowheads), distal atelectasis, and abscess formation (arrow). Also note sclerosis of the adjacent rib representing osteomyelitis (white arrow in (b))
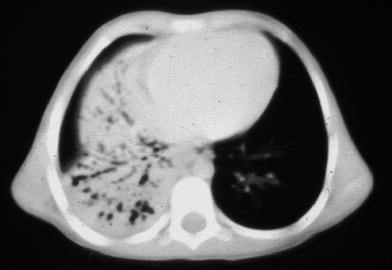
Fig. 14
Axial CT of the lower chest in a case of chronic foreign body aspiration into the right intermediate bronchus, causing collapse and bronchiectasis in the right middle lobe and right lower lobe

Fig. 15
Right lateral decubitus chest CT demonstrates air-trapping in the right (dependent) lung, following aspiration of a piece of an eraser
We routinely use a helical technique with 3-mm collimation, 3-mm reconstructions for adolescents and children, with the smallest possible field of view. For infants and toddlers we may use 2-mm collimation with 1-mm reconstructions. Tube current can be reduced to as low as 25–30 mA for such studies, and kV can be reduced to as low as 80–90, depending on child age and weight. Multiplanar reconstructions are helpful in detecting airway foreign bodies (Kosucu et al. 2004; Kocaoglu et al. 2006; Adaletli et al. 2007; Bai et al. 2011). Virtual bronchoscopy can further contribute to the diagnosis and location of a presumed aspirated foreign body when a chest radiograph is not informative (Konen et al. 1998; Haliloglu et al. 2003; Kosucu et al. 2004; Kocaoglu et al. 2006; Adaletli et al. 2007; Cevizci et al. 2008). Virtual bronchoscopy has the advantage of demonstrating smaller airways than possible to view with conventional bronchoscopy, as well as the airways beyond an obstructed bronchus (Haliloglu et al. 2003; Kosucu et al. 2004; Adaletli et al. 2007; Cevizci et al. 2008; Bhat et al. 2010). However, reconstructions are time consuming and have not been shown to contribute additional information over multiplanar reconstructions (Kosucu et al. 2004; Kocaoglu et al. 2006). The major disadvantage of CT examinations is the inherent radiation exposure of the young patient, despite improved technology and increasing awareness of both manufacturers and radiologists to minimize radiation dose. Therefore, it is imperative to weight the potential benefit of the additional data yielded as a result of each study against the potential risk, especially in cases when conventional bronchoscopy, that might be both diagnostic and therapeutic, is to be carried out as well (McHugh 2005; Manach et al. 2013).
Nuclear medicine is not recommended for the diagnosis of a bronchial foreign body. When used, however, the lung scan can be helpful in defining regional decrease in ventilation and perfusion (Fig. 10b), as well as air-trapping, and can thus guide endoscopy to the area of suspected obstruction (Holland and Trumbull 1979; Lull et al. 1980; Balink et al. 2012).
Magnetic resonance imaging (MRI) studies are also rarely used for investigating suspected foreign body aspiration, especially because at present the use of sedation is mandatory. Nevertheless, several reports have described the utility of MRI in the management of foreign body aspiration. Due to the multiplanar nature of this modality, MRI can accurately locate the foreign body prior to bronchoscopy, and can also reveal foreign bodies in multiple sites during the same study (Imaizumi et al. 1994; Morijiri et al. 1994). The high fat content of aspirated peanuts, as well as the high water content of most organic foreign bodies enable clear delineation of their size and site (O’Uchi et al. 1992; Tashita et al. 1998).
Ultrasound (US) can be of value in defining the presence, nature, and extent of complications of foreign bodies, such as consolidation with an air bronchogram, pleural effusion or empyema, loculated pockets of fluid, chest wall abscess, or rib osteomyelitis (Seibert et al. 1986; Giudicelli et al. 1996). Ultrasound can presumably demonstrate the foreign body within the collapsed lung; however, the authors do not have experience in this.
6 Imaging Findings
Imaging findings in cases of foreign body aspiration are determined by the presence and the degree of airway obstruction, the site of the foreign body, its type, and the time that has elapsed between aspiration and the performance of imaging studies.
A foreign body can be present in the airway without causing obstruction. This situation almost always involves an oblong foreign body in the trachea, small enough to have been aspirated yet not large enough to block the (relatively) larger airway. In such a case the chest radiograph and fluoroscopy will usually be negative, although pneumonia might be present (Esclamado and Richardson 1987; Mu et al. 1990; Cataneo et al. 1997). Fluoroscopy or a high kV soft tissue technique with a copper filter may reveal the foreign body (Fig. 11). CT (Gupta and Berry 1991; Malis and Hayes 1995; Bertolani et al. 1999) and MR imaging (O’Uchi et al. 1992; Imaizumi et al. 1994; Morijiri et al. 1994; Tashita et al. 1998) can demonstrate the presence and often the nature of such a foreign body when the initial imaging is negative.
Obstruction of the airway can vary in severity and occur at different levels of the tracheobronchial tree. Laryngeal or subglottic foreign bodies tend to be thinner and are often arranged in an anteroposterior direction (sagittal plane) in the region of the vocal cords, as opposed to esophageal foreign bodies, which lie in a transverse direction (coronal plane). If the foreign body is a thin, rounded object (e.g., a coin or an egg shell), it will be seen as a thin line on the anteroposterior chest radiograph when located between the vocal cords, and as a rounded shadow when located in the esophagus. Tracheal foreign bodies usually cause no obstruction or incomplete obstruction. The imaging findings, when present, are often bilateral: either bilateral volume loss or bilateral hyperinflation (Fig. 7). In the latter case, the diaphragms are flattened and in a low position. When small enough, the foreign body may move in the tracheobronchial tree during the different phases of the respiratory cycle, as a result of coughing or following treatment with inhaled bronchodilators, with consequent changes in the clinical and imaging findings (Figs. 5, 6) (Metrangelo et al. 1999).
About three quarters of airway foreign bodies are found in the main bronchi (Blazer et al. 1980; Mantel and Butenandt 1986; Zhijun et al. 2008; Kitcher 2009; Saki et al. 2009), where they cause partial or complete obstruction. Plain films and fluoroscopy seldom demonstrate a nonopaque foreign body. An oblique projection obtained with these modalities, placing the upper airway over the mediastinal soft tissues, creates better contrast and enhances demonstration of the foreign body (Fig. 3). This technique may also indirectly reveal the presence of a foreign body by virtue of focal absence of the air column in the obstructed bronchus, the so-called “absent segment” or the “interrupted bronchus” sign (Fig. 2) (Grunebaum et al. 1979; Lim-Dunham and Yousefzadeh 1999). Partial obstruction results in localized air-trapping distal to the site of the foreign body, with resultant widening of the intercostal spaces, and flattening of the ribs and diaphragms, and blunting of the costophrenic angles (Laks and Barzilay 1988; Mu et al. 1990; Ernst and Mahmud 1994; Black et al. 1994; Oguz et al. 2000). Segmental or lobar emphysema due to air trapping has been reported to be present in ~40 % of children with proven foreign body aspiration (Bai et al. 2011; Sattar et al. 2011; Boufersaoui et al. 2013; Mortellaro et al. 2013); in some studies, this is indicated as the most specific finding in the chest radiograph (Hitter et al. 2011; Sattar et al. 2011; Boufersaoui et al. 2013). Pulmonary hyperexpansion with sparse vascularity or displacement of the mediastinum to the contralateral side on expiration indicates the presence of obstructive emphysema (Figs. 2, 5, 6, 9, 10) (Mu et al. 1990). Complete obstruction also causes segmental or lobar atelectasis (Figs. 2, 3, 5, 6), or even total collapse of the ipsilateral lung (Figs. 5, 6). The collapsed area may initially be homogeneously opaque, due to the absence of air in the alveoli and bronchi. Collateral diffusion of air to the bronchioles distal to the obstructing foreign body may result in a faint air bronchogram. In cases with lobar atelectasis, compensatory emphysema of the ipsilateral respected lobes and of the contralateral lung is often present (Theander 1970). In contrast to obstructive emphysema, pulmonary vessels are prominent in compensatory emphysema.
The presence of lobar collapse with localized pneumothorax should suggest the diagnosis of acute bronchial obstruction of any etiology (Berdon et al. 1984; Nimkin et al. 1995) (Fig. 16). The combination of increased pressure and the presence of a sharp object in the bronchi can result in a bronchopleural fistula. This complication, as well as pneumonia secondary to focal obstruction, may give rise to pleural effusion or empyema (Dogan et al. 1999). Pleural effusion as the only imaging sign of foreign body aspiration has also been reported (Auerback 1990). In prolonged cases, localized or multifocal bronchiectasis may develop and be evident on the plain radiograph (Fig. 3) or on CT (Fig. 14); these are best evaluated by high-resolution CT with thin section collimation (Kuhn 1993). Subacute or chronic infection and inflammatory response may form a parenchymal abscess adjacent or distal to the foreign body, or a chest wall abscess and rib osteomyelitis (Fig. 13).


Fig. 16
Collapsed right lower lobe with localized pneumothorax due to acute foreign body aspiration
7 Complications
Complications of foreign body aspiration can be immediate or long term. A foreign body can cause fatal asphyxia and death when there is complete obstruction of the major airways (Buntain et al. 1979; Black et al. 1984, 1994; Byard 1994; Bhana et al. 2000; Ciftci et al. 2003). This occurrence is rare, although it was described in 5–7.5 % of foreign body aspiration cases in one report (Menendez et al. 1991; Foltran et al. 2013). This high incidence has not been observed in the author’s experience and is not corroborated in most other reports. Complete obstruction can develops abruptly when a relatively small foreign body is aspirated into a trachea with a pre-existing (sometimes unknown) focal narrowing caused by a vascular ring, tracheomalacia or external compression. Complete obstruction can also occur during bronchoscopy for extraction of a foreign body (Fig. 7).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree