He-3
Xe-129
Essentially insoluble in biological tissue
Weakly soluble in biological tissue
Cannot provide gas exchange information
Provides gas exchange information
No known side effects
CNS (euphoric and anesthetic) side effects
Low molecular weight
High molecular weight
Large diffusion coefficient
Small diffusion coefficient
Higher percentage of atomic polarizationa
Lower percentage of atomic polarizationa
Shortage of supply
Readily available
>$500/L
<$200/L
He-3 is relatively insoluble in biological tissue and, therefore, is not taken up by the body through the alveolar-capillary interface. Xe-129 is weakly soluble in biological tissues and demonstrates a relatively large chemical shift between Xe-129 in the gas phase and Xe-129 dissolved in tissue or blood. By exploiting this property, regional information about pulmonary gas exchange can be obtained. The biological solubility of Xe-129 also results in side effects. At the doses used in medical imaging, some patients experience transient CNS effects including euphoria, altered sensations, and drowsiness. At doses higher than typically used in imaging, xenon has anesthetic effects. He-3 has few, if any, side effects. Historically, higher polarizations could be achieved with He-3 than Xe-129. Thus, much of the initial human research with HG-MRI was done with He-3. However, recent technical advances have greatly increased the polarizations achievable with Xe-129 (Hersman et al. 2008). He-3, as a low molecular weight atom, has a much larger diffusion coefficient than Xe-129 which has implications for diffusion imaging. A current shortage of He-3 has resulted in increased costs, making Xe-129 more attractive as a contrast agent for MRI (Shea and Morgan 2010).
2.2 MR Sequences
Five basic MRI techniques using hyperpolarized gas contrast imaging have been developed. The first four techniques below can be performed with either He-3 or Xe-129, but the fifth, Dissolved Phase Imaging, is limited to Xe-129.
1.
Static Spin Density (Ventilation Imaging)—used to assess pulmonary ventilation.
2.
Dynamic Spin Density Imaging—used to assess the temporal kinetics of gas flow in the lung.
3.
Diffusion Imaging—used to assess lung microstructure by measuring the restriction to diffusion of the He-3 or Xe-129 atoms.
4.
Oxygen Sensitive Imaging—used to quantify the alveolar partial pressure of oxygen.
5.
Dissolved Phase Imaging—used to measure the movement of Xe-129 atoms from the lung airspace into the tissue and blood, that is, gas exchange.
2.2.1 Static Spin Density Imaging
With static spin density imaging, the patient inhales the hyperpolarized gas and spin density imaging is performed during a short breath hold. Assuming a homogenous B1 field, the signal received from any area of the lung is proportional to the number of polarized gas atoms within that area. Assuming that the rate of depolarization of the gas is similar throughout the lung over the course of the breath hold, the signal is approximately proportional to the ventilation in that region of the lung. Well-ventilated regions will contain a large number of polarized gas atoms and thus produce a strong signal (appearing white on the images). Areas of the lung that are poorly ventilated will contain fewer polarized gas atoms and appear grey or black on the ventilation images, so-called ventilation defects. Ventilation defects have been found in patients with obstructive lung diseases including asthma, cystic fibrosis (CF), COPD, and bronchiolitis obliterans (Altes et al. 2001; Donnelly et al. 1999; Kauczor et al. 1996; McAdams et al. 1999, 2000).
2.2.2 Dynamic Spin Density Imaging
2.2.3 Diffusion Imaging
Similar to proton-based diffusion imaging, hyperpolarized gas diffusion imaging assesses the degree to which the hyperpolarized gas atoms are restricted in movement. A typically derived measure of the degree of restriction is the apparent diffusion coefficient (ADC). Within the lungs, the gas atom movement is restricted by the airway and alveolar walls. Thus, the ADC reflects the size and connectedness of the lung airspaces. In patients with COPD, the hyperpolarized gas ADC is elevated relative to age-matched healthy subjects, a finding which is thought to reflect the known alveolar enlargement in this disease (Kirby et al. 2012; Saam et al. 2000; Salerno et al. 2002). Histology studies in animal models of emphysema and in explanted human lungs have confirmed the correlation between ADC and alveolar size (Chen et al. 2000; Mata et al. 2007; Woods et al. 2006).
2.2.4 Oxygen Sensitive Imaging
The rate of decay of the polarization of both He-3 and Xe-129 depends upon the local environment and is hastened by molecular oxygen. Thus, by measuring the T1 of the He-3 or Xe-129 gas in the lungs, it is possible to estimate the partial pressure of oxygen regionally within the lungs (Deninger et al. 1999; Fischer et al. 2004; Kadlecek et al. 2013). Little work has been done with oxygen sensitive imaging in children so this technique will not be discussed further here.
2.2.5 Dissolved Phase Imaging
Because Xe-129 is weakly soluble in biological tissues and there is a relatively large chemical shift between gas phase and dissolved phase Xe-129, it is possible to image the regional gas transfer within the lung (Kaushik et al. 2013; Qing et al. 2013; Ruppert et al. 2000). This technique in concert with ventilation imaging permits a comprehensive evaluation of lung physiology and the relative contribution of airway and vascular processes to lung disease. For example, ventilation imaging shows the airway component of asthma, but there may be a vascular component that could be elucidated with dissolved phase imaging. Little work has been done with dissolved phase imaging to date in the pediatric population.
3 Applications in Pediatric Lung Disease
3.1 Healthy
The lung in disease-free children and young adults characteristically demonstrates a homogenous, high signal on hyperpolarized gas MR spin density (ventilation) imaging (Fig. 1) (Altes et al. 2001; Lee et al. 2009). Small peripheral ventilation defects occur in healthy individuals, with increased prevalence in older adults (Parraga et al. 2007). It is possible that ventilation defects occur with normal aging, but these defects could be related to prior environmental or infectious insults.
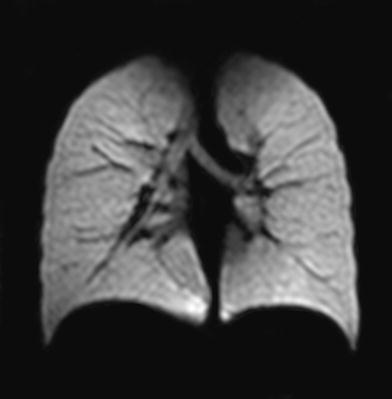
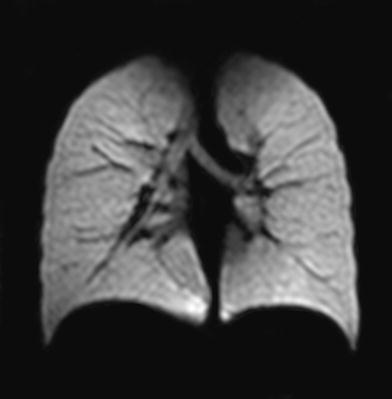
Fig. 1
Coronal He-3 MR ventilation image of the lungs of a healthy subject. Uniformly high signal is obtained from the lung airspaces and there are no ventilation defects
Enlargement of alveoli during childhood can be detected using diffusion-weighted He-3 MRI (Fig. 2) (Altes et al. 2006b). Prior to He-3 MRI, it was thought that alveolar development ceased in early childhood (age 2–5 years) and that further lung growth was simply due to expansion in size of the existing lung structures. A recent study found that the He-3 MR ADC in the lungs increased with increasing age during childhood, but the rate of increase was less than expected if lung growth occurred only by expansion of the preexisting alveoli. This finding suggests that there is both enlargement of the individual alveoli and growth of new alveoli (neoalveolarization) occurring simultaneously throughout childhood and adolescence (Narayanan et al. 2012). Diffusion-weighted HG-MRI provides the opportunity to noninvasively assess alveolar development in childhood, both in healthy children and in children with disorders that perturb alveolar development such as bronchopulmonary dysplasia (BPD) and congenital diaphragmatic hernia.
Fig. 2
Coronal He-3 ADC maps of two healthy subjects age 8.8 and 27.6 years. Very high ADC values are present in the trachea and main bronchi where the diffusion of the gas is less restricted. The ADC values in the young adult are much higher than in the child, indicating less restriction of diffusion of He-3 atoms within the airspaces of the lungs. This is thought to relate to the known enlargement of alveoli from lung growth in childhood. Reprinted with permission from Altes et al. (2006b)
3.2 Asthma
Asthma is the most common chronic disease of childhood, affecting as many as 20 % of children at some time during childhood. The disease predominantly involves the small and medium-sized airways with symptoms usually associated with variable airflow obstruction, caused by bronchoconstriction, airway wall edema, mucous plug formation, and airway remodeling (Campana et al. 2009; Hogg 2002). There is a growing concept that the severity of the disease in adulthood may be significantly reduced through early childhood diagnosis and control. The majority of HG-MRI studies in asthmatics have been performed in young adults, with a few studies conducted on children. The majority of the studies in asthma employed ventilation imaging.
In patients with asthma, ventilation defects are common and increase with disease severity as assessed by spirometry and symptomatology, Fig. 3 (Altes et al. 2001; de Lange et al. 2006). Ventilation defects in asthmatics could be caused by focal airway narrowing, mucus plugging, and/or airway closure. Ventilation defects are found in asthmatics with normal spirometry, indicating that hyperpolarized gas MRI detects ventilation abnormalities in the lungs with greater sensitivity than does spirometry.
Fig. 3
Axial He-3 MR ventilation images in three patients with asthma. There are increasing numbers of ventilation defects (arrows denoting black and grey areas) with increasing asthma severity and decreasing FEV1 % predicted
Hyperpolarized gas MR is capable of detecting regional patterns of airway closure. HG-MRI can be repeated to assess changes in the regional patterns of airway closure in response to treatment or over time without the risk of ionizing radiation exposure to the patient. de Lange et al. (2009) found that ventilation defects in individual asthmatics tend to persist or recur in the same locations in the lung over time periods of weeks to months (Fig. 4). This suggests that asthma may not affect all regions of the lung equally but may instead have a regional predisposition in individual patients, analogous to the regional heterogeneity of other autoimmune diseases such as Crohn disease.
Fig. 4




Axial He-3 MR ventilation images from a single subject imaged on three different days. The three ventilation defects present on Day 1 resolve on Day 55 but recur on Day 93. There is striking similarity in the appearance of the defects on Day 1 and Day 93. Modified and reprinted with permission from de Lange et al. (2009)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree