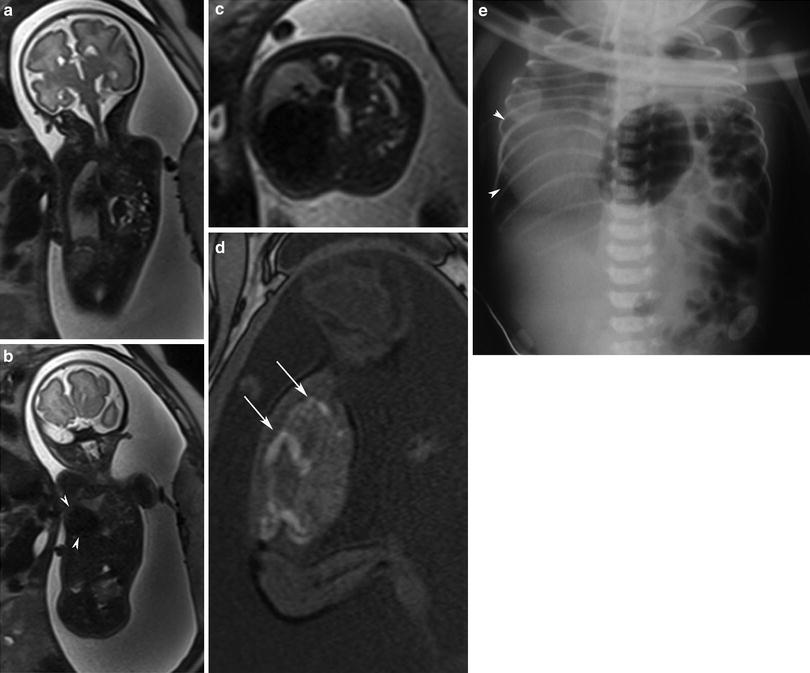
Fig. 1
Normal lung. a Coronal T2-weighted image (33 weeks) showing great vessels and lungs with normal volume and signal intensity. b Axial T2-weighted image showing the normal high signal intensity suggestive of habitual pulmonary development. Note the normal thymus (arrowheads). c Sagittal T2-weighted showing the high signal intensity of the lungs due to the presence of amniotic fluid within the parenchyma. Note the thymus anteriorly to the heart (arrowheads)
At the moment, there are no known biological effects of MR imaging on the fetus. The current recommendations by the Safety Committee of the Society of Magnetic Resonance Imaging regarding MR imaging safety during pregnancy suggest using this technique only in patients with inconclusive US. However, several imaging centers avoid acquiring MR imaging during the first trimester of the pregnancy, because there are no benefits in fetal diagnosis. Gadolinium-based contrast media are not recommended because they cross the placenta and penetrate the fetal circulation within seconds after intravenous administration (Shellock and Kanal 1991; Guo and Luo 2006).
3 Indications for Fetal MR Imaging of the Chest
Although US remains the gold standard imaging technique for screening of fetal malformations, MR imaging has been advancing in the last two decades as a complementary method for studying fetal anatomy (Hubbard et al. 1999; Shinmoto et al. 2000; Coakley et al. 2004). One of the most important advantages of MR imaging is soft tissue contrast. In addition, in cases of severe oligohydramnios or maternal obesity, this method can provide essential information not possible with US studies.
Improvements in US resolution over the past two decades have increased the ability to diagnose fetal chest anomalies. However, recent advances in MR imaging techniques have also increased the value of MR in evaluating these malformations, especially for atypical lesions and masses (Levine et al. 2003; Kasprian et al. 2006).
There are many factors that influence normal fetal lung growth, such as adequate size and shape of the fetal thorax, fetal breathing, movements, and an adequate amount of amniotic fluid. Pulmonary hypoplasia can occur when any of these factors are abnormal, but it is most commonly seen in patients with intrathoracic space occupying lesions. The most common space occupying lesions in the fetal thorax are CDH, CPAM, BPS, and fetal hydrothorax (Hubbard et al. 1999; Levine et al. 2003; Newman 2006).
4 Pulmonary Lesions
4.1 Congenital Pulmonary Airway Malformation
The CPAM, previously known as congenital adenomatoid malformation, is the most common congenital lung malformation. It is a lesion characterized by abnormal branching of immature bronchioles that may communicate with the tracheobronchial tree. The CPAM usually has arterial blood supply originating from the normal pulmonary circulation and venous drainage into normal pulmonary veins. However in hybrid lesions, a systemic blood supply may be evidenced. These lesions are often diagnosed on prenatal US or MR imaging (Daltro et al. 2004; Bulas and Egloff 2011). Fetal MR imaging is helpful in its ability to distinguish CPAM from other entities such as CDH, BPS, bronchogenic cyst, neurenteric/enteric cyst, laryngeal or tracheal atresia, and mediastinal cystic teratomas.
For clinical management, the classification into micro- or macrocystic appearance has been used. Adzick el al. (1985) suggested classifying CPAMs into two types: macrocystic (>5 mm) and microcystic (<5 mm). However, the original classification of Stocker et al. (1977) remains more commonly used. These authors divided the lesions into three types: type I, macrocystic (>2 cm); type II, multiple small cysts; and type III, solid form (microscopic cysts). A newer classification proposed by Stocker (2002, 2009) considered also the pathologic analysis to the categorization, with the lesions that have been classified according to cyst size and histologic similarity to segments of the developing bronchial tree and airspaces. Five types were proposed by these authors: type 0 a tracheal or bronchial origin and is pathologically defined as acinar dysgenesis or dysplasia; type 1 is defined as large cystic lesions (2–10 cm) with a bronchial or bronchiolar origin; type 2 represents the small cystic lesions (0.5–2 cm) with a bronchiolar origin; type 3 has a bronchiolar–alveolar duct origin (adenomatoid type) with microscopic cysts; and type 4 with distal acinar origin and usually localized to one lobe and demonstrated large cysts with mediastinal shift. Given the controversial and occasionally confusing terminology and the paucity of literature correlating pathology, it is best to carefully describe the anatomy of the malformation and associated changes related to large lesions to guide any surgery or management (Epelman et al. 2010). Depending on the type of the CPAM, the US and MR imaging may vary. The cystic components will present as an anechoic mass by US and will be bright on T2-weighted MR images (Figs. 2 and 3). On the other hand, solid components of CPAM will present as a homogeneous echogenic mass by US and hyperintense lesions on T2-weighted MR images.
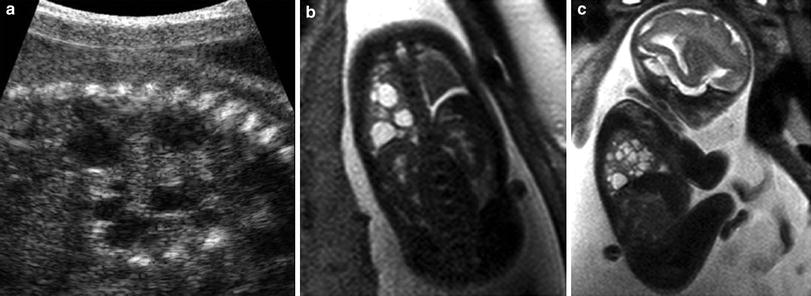
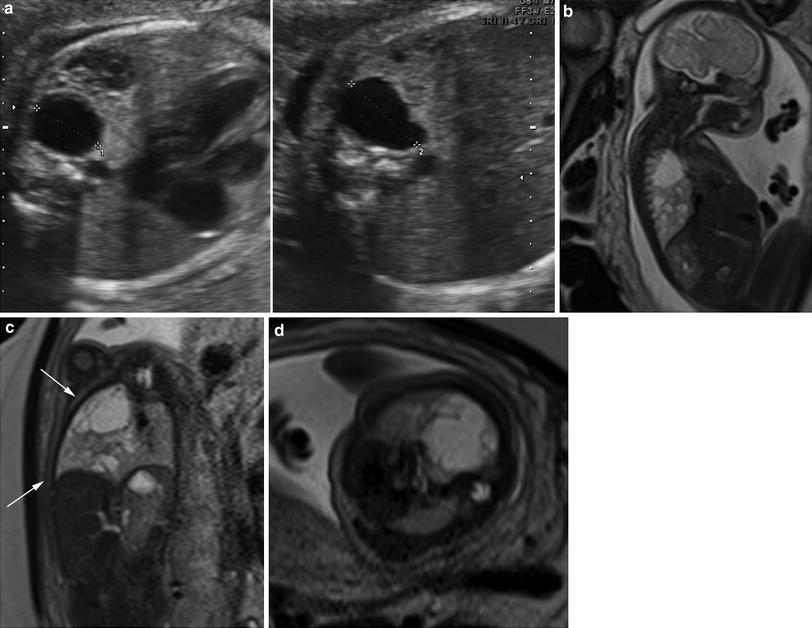
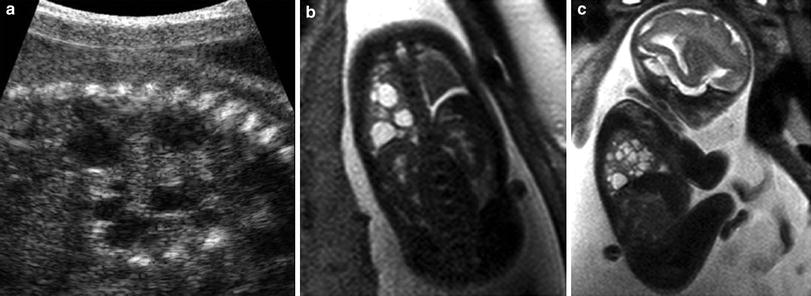
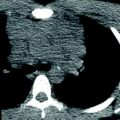
Fig. 2
Cystic lung lesion. a Ultrasound view of multiple cysts of different sizes in the right lung. b, c Coronal and sagittal T2-weighted view shows cysts in the right lung. Note the low intensity signal in the left lung and small left hymithorax
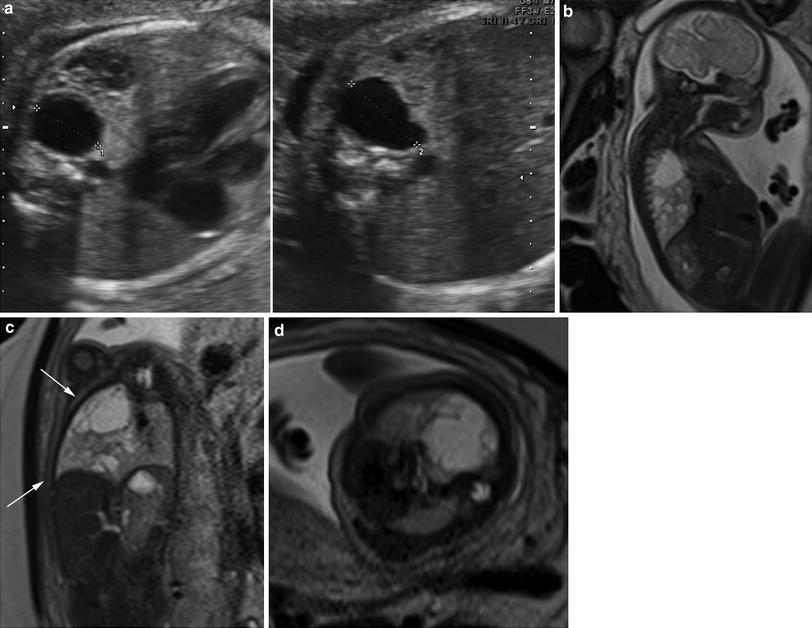
Fig. 3
Cystic lung lesion with mass effect. a Ultrasound view of multiple cysts of different sizes in the right lung. b–d Sagittal, coronal, and axial T2-weighted images demonstrate multiple cysts in the right lung (white arrow). Note the mass effect of the lesion, displacing the mediastinum and compressing the left lung parenchyma
The natural history and prognosis of CPAM are variable. Maximum growth of a CPAM lesion typically occurs between 20 and 26 weeks of gestation. In the late second trimester, the mass often decreases in size (Bulas and Egloff 2011). The prognosis associated with this lesion is dependent on the size, rather than the histologic type of the lesion. Larger lesions are associated with higher frequency of mediastinal shift, pulmonary hypoplasia, vascular compromise, hydrops, and also hydramnios (Hubbard et al. 1999; Witlox et al. 2011; Schrey et al. 2012; Biyyam et al. 2010).
4.2 Bronchopulmonary Sequestration
Bronchopulmonary sequestration is a mass of pulmonary tissue that does not communicate with the central airway through a normal bronchial connection, and that receives its blood supply through an anomalous systemic artery, resulting in a nonfunctioning lung tissue. The arterial supply may arise from the descending thoracic or abdominal aorta, or from one of its branches (Daltro et al. 2010). Bronchopulmonary sequestration may be extralobar or intralobar, although most often the BPS present as hybrid lesions with components of both sequestration and CPAM. The hybrid cases are described as a cystic lesion with a feeding systemic vessel (Fig. 4). The extralobar form is most commonly diagnosed in the prenatal and neonatal periods, whereas the intralobar form, although nowadays could be seen in the prenatal period, is more commonly seen in childhood. Some of the BPS lesions may regress in utero (Daltro et al. 2004; Epelman et al. 2010).
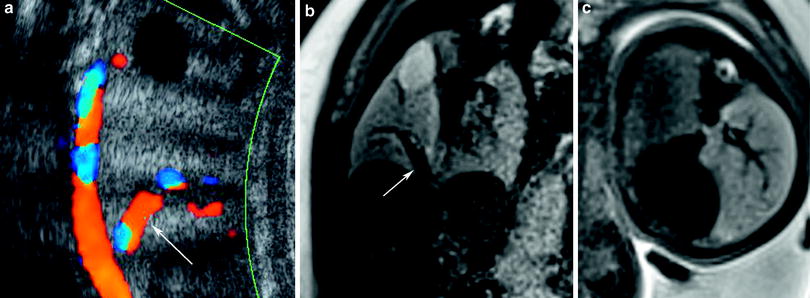
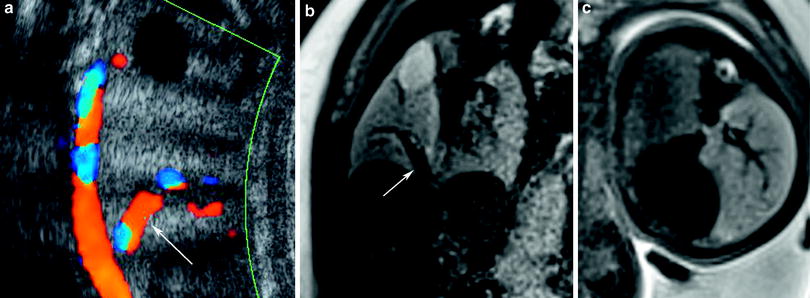
Fig. 4
Hybrid lung lesion. a Ultrasound image of a hybrid lesion composed of an intralobar sequestration and a CPAM lesion. Note the hyperechoic lesion with arterial supply from the aorta (white arrow). b, c. Coronal and axial T2-weighted images showing a hyperintense mass in the lung, with arterial supply from the aorta (white arrow) associated with a cystic lesion in the upper lobe
Prenatal US demonstrates bronchopulmonary sequestration as a homogeneously hyperechogenic mass in the lower lobes of the lung. On MR imaging, sequestered lung tissue has markedly high signal on T2- and low signal on T1-weighted images. The characterization of the anomalous vessels is possible by US but very difficult by MR imaging (Fig. 5).
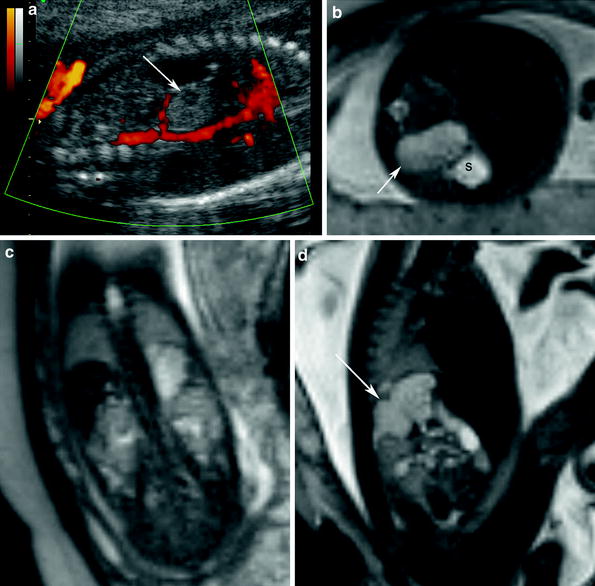
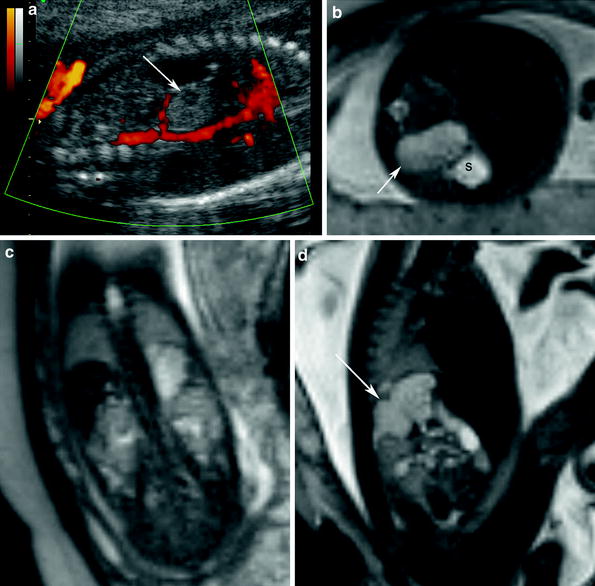
Fig. 5
Pulmonary sequestration. a Prenatal ultrasound (27 weeks) reveals hyperechoic image with arterial supply from the aorta (white arrow). b–d Axial, coronal and sagittal T2-weighted images showing hyperintense signal mass in the base of the left lung. Axial view shows the lesion close to the stomach
The differential diagnosis of pulmonary sequestration may include neuroblastoma and adrenal hemorrhage to the infradiaphragmatic lesions. Pulmonary sequestration is more commonly seen as a solid lesion located on the left side, and can be seen with US during the second trimester. On the other hand, neuroblastoma usually contains cystic areas, which occurs more frequently on the right side and is more commonly diagnosed in the third trimester (Kays et al. 2006; Biyyam et al. 2010).
4.3 Bronchogenic Cyst
The bronchogenic cyst is the most common cystic lesion of the mediastinum. It is classified as an anomaly of the ventral bud of the primitive gut that occurs between the 26th and 40th days of embryonic development. The walls of bronchogenic cysts are thin, covered by respiratory epithelium and contain mucinous material. Most of the cysts are seen in the mediastinum or near the carina (Fig. 6). Less commonly, the cysts may occur within the lung parenchyma, pleura, or diaphragm. When the cysts are seen in the lung parenchyma, they are usually located in the inferior lobes. Bronchogenic cysts are sometimes found in association with other congenital pulmonary malformations such as sequestration or lobar overinflation (Daltro et al. 2004; Stocker 2009).


Fig. 6
Bronchogenic cyst. Coronal T2-weighted image shows cystic lesion in the base of the left lung
4.4 Neurenteric Cyst
The neurenteric cyst is the main lesion included in the differential diagnosis of bronchogenic cysts. The walls of neurenteric cysts have nervous and gastrointestinal elements, with intestinal epithelium that may be ciliated. They are usually seen in the posterior mediastinum, and may communicate with the esophagus, stomach, or duodenum. Neuroenteric cysts are frequently associated with anomalies of vertebral segmentation, and they can be asymptomatic at birth or present minimal respiratory distress (Fig. 7) (Newman 2006).
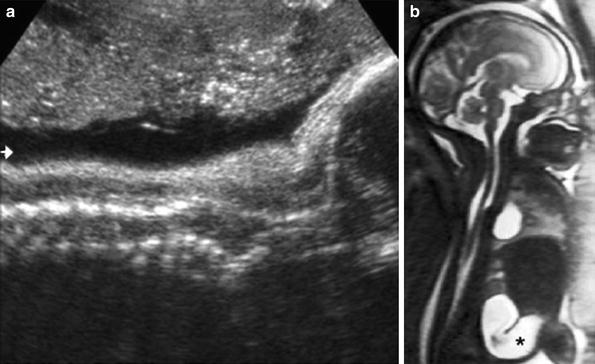
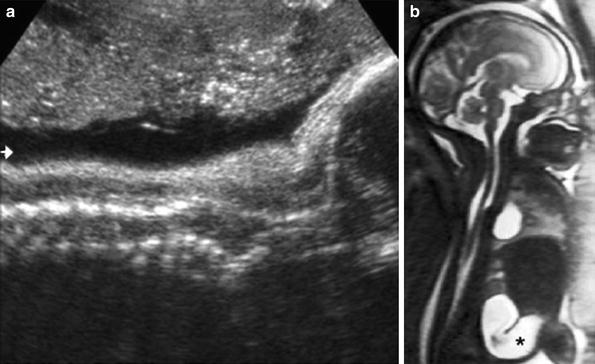
Fig. 7
Neuroenteric cyst. a Ultrasound view of the spine shows an associated segmental anomaly (arrow). b Sagittal T2-weighted image showing the cyst close to the spine. Note the dilated bowel loop (*)
4.5 Pulmonary Arteriovenous Malformations
Pulmonary arteriovenous malformations (PAVMs) result from an abnormal communication between the pulmonary arteries and veins. Most of the lesions are congenital in origin and the female: male ratio is around 2:1. Infants and children with PAVMs may be asymptomatic; however, if the lesions are large enough to cause a significant right-to-left shunt, the patient may present with cyanosis or heart failure. Between 50 and 70 % of PAVMs occur in the lower lobes and about 2/3 of the patients have multiple lesions (Hansell et al. 2005) (Fig. 8).
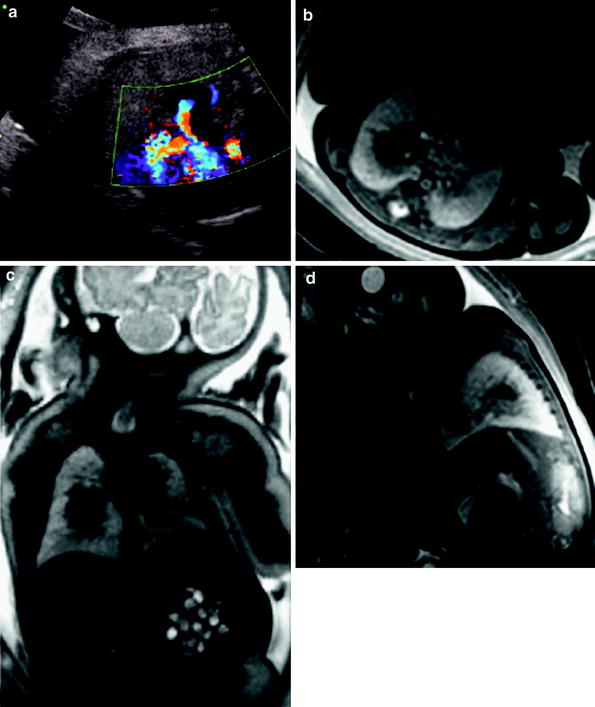
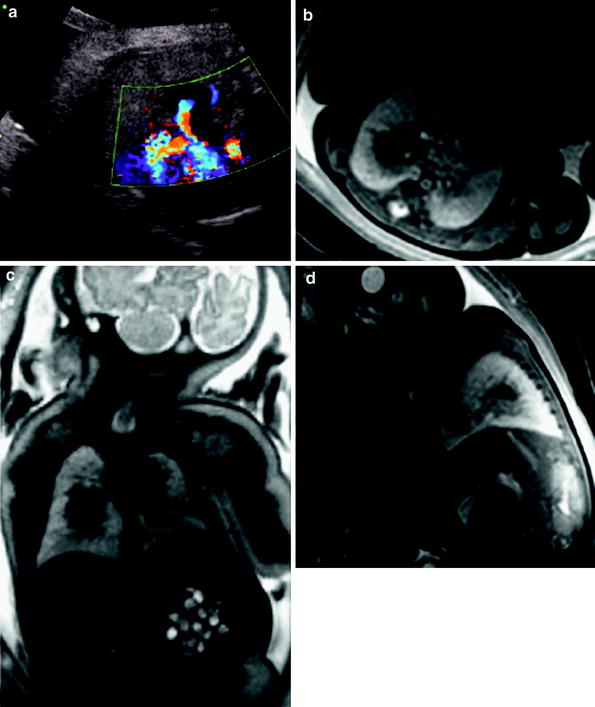
Fig. 8
a Pulmonary arteriovenous malformation. Ultrasound view shows a vascular lesion close to the heart. b–d Axial, coronal, and sagittal T2-weighted images reveal a low signal intensity lesion in the middle of the right lung
4.6 Congenital Pulmonary Lymphangiectasia
Congenital pulmonary lymphangiectasia is a generalized dilation of otherwise histopathologically normal lymphatic vessels. The condition may occur primarily, or secondary to severe pulmonary venous obstruction in cases of total anomalous pulmonary venous return or hypoplastic left heart syndrome. Congenital pulmonary lymphangiectasia is frequently associated with genetic diseases, including Noonan, Turner, Ehlers-Danlos, and Down syndromes (Faul et al. 2000) (Fig. 9).
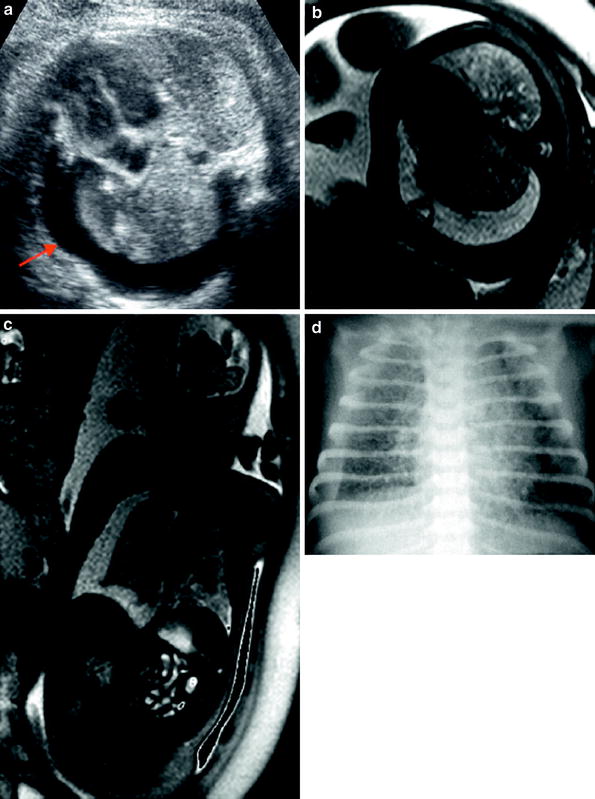
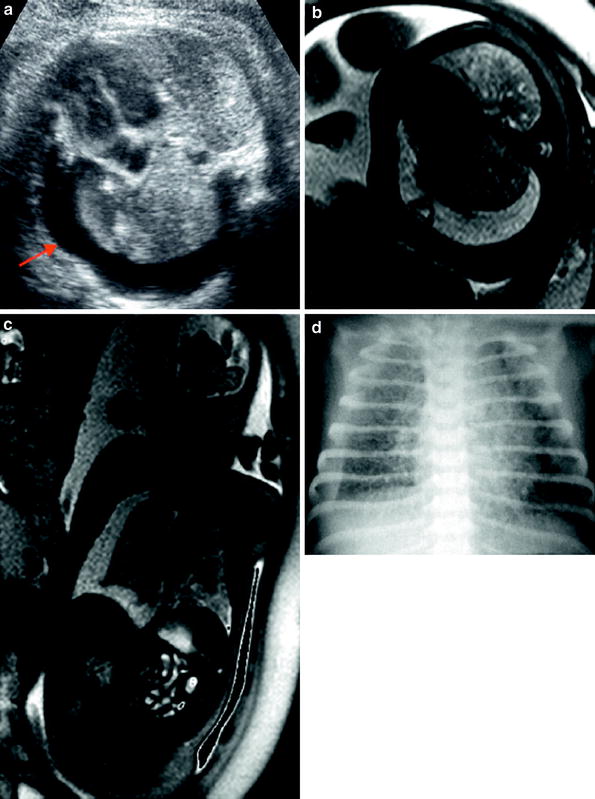
Fig. 9
Congenital pulmonary lymphangiectasia. a Ultrasound view shows right hydrothorax (arrow). b, c. Axial and coronal T2-weighted images demonstrate right hydrothorax compressing the homolateral lung. Note the low signal intensity of the both lungs. d Conventional X-ray some hours after delivery reveals diffuse reticular infiltrate and right pleural effusion
5 Hydrothorax
Hydrothorax is the accumulation of fluid in the pleural space, and can be primary or secondary in origin. Most hydrothoraces are primary, with chylothorax being the most common. The chylothorax occurs because of an abnormality in the formation of the thoracic lymphatic ducts, with resultant abnormal drainage. It is usually unilateral, occurring more frequently on the right side. In patients with secondary pleural effusions, the most common causes are chromosomal abnormalities (Down or Turner syndrome) or infectious diseases (cytomegalovirus, toxoplasmosis). Hydrothorax may also be seen in cases of fetal hydrops.
The diagnosis of hydrothorax can be made with US, which can also help to guide treatment, including drainages and shunts (Fig. 10).
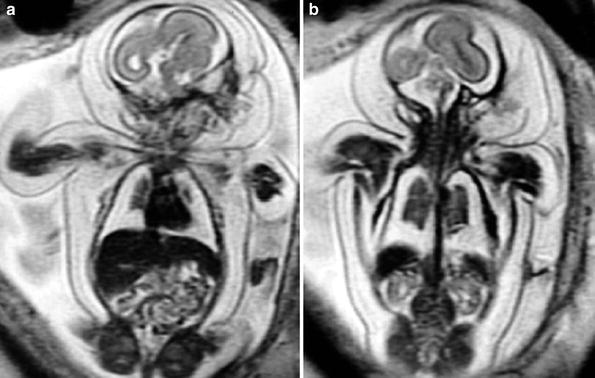
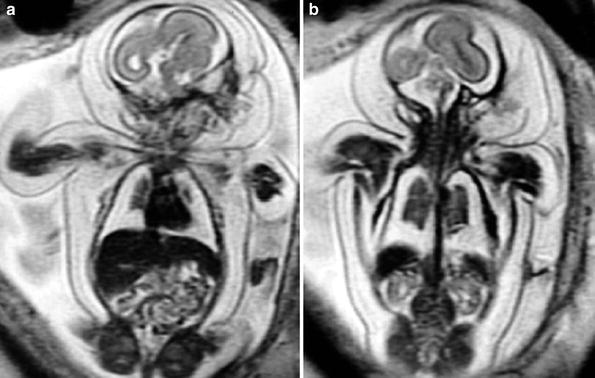
Fig. 10
Hydrothorax. a, b Coronal T2-weighted image of the fetus (26 weeks) shows a large bilateral hydrothorax. Note also the cutaneous edema and small lungs
6 Congenital Diaphragmatic Hernia
Congenital diaphragmatic hernia is defined as a partial or complete lack of development of the diaphragm, allowing the migration of abdominal structures into the thorax; these structures can compress the lungs and affect their development (Paek et al. 2001; Kays 2006). The CDH can be divided in two forms: an early form, in which the abdominal organs develop inside the thorax, and a late form, which is associated with secondary migration of the abdominal organs to the thorax. The fetal MR imaging is important in these cases allowing an anatomic evaluation and also helping to determinate the specific type of CDH and the effect of the hernia contents on adjacent structures. The fetal MR imaging may also be used to calculate lung volume and liver herniation measurements as well as to the calculation of the diameters of the pulmonary arteries and aorta (Mehollin-Ray et al. 2012; Recio Rodríguez et al. 2012).
The most common type of CDH occurs through the Bochdalek foramina, and occurs more frequently on the left side (Fig. 11). US can suggest this diagnosis between the 2nd and 3rd trimesters, demonstrating the stomach and small bowel loops in the left hemi-thorax, and the heart deviated to the right side. Around 12 % of the cases of CDH occur on the right. In most of these cases the liver is seen in the right hemi-thorax, compressing the heart in the left hemi-thorax (Fig. 12). The migration of small bowel loops into the right hemi-thorax is uncommon (Okazaki et al. 2003; Bedoyan et al. 2004; Hedrick et al. 2004). An extreme form of congenital diaphragmatic hernia is associated with the complete bilateral agenesis of the diaphragm (Fig. 13). In these cases, the lack of mediastinal shift may be evident and the lung parenchyma may be completely compressed by the abdominal content herniated (Hiasa et al. 2012; Jasnosz et al. 1994; Wang et al. 1997; Mehollin-RAY et al. 2012).