Fig. 4.1
Anatomy of the mammary gland. Anterior view. Displayed is the areola-nipple complex, in which the lactiferous ducts of the lobes (15–20), as components of the gland, converge. Csl Cooper’s suspensory ligaments, eom external oblique muscle, gl gland lobules, ld lactiferous ducts, pmm pectoralis major muscle, sam serratus anterior muscle
The mammary gland has both a parenchymal and a stromal component. It consists of 15–20 segments or lobes, each one of them with a main lactiferous duct opening on the nipple. The ducts converge beneath the nipple, with about 5–10 major ducts draining into the nipple. Each lobe is subdivided into many smaller lobules (20–40), ending in acinar structures, consisting of cylindrical and cubic cells, located around the lumen, in which the secretion flows during breastfeeding. Therefore, the breast is considered a compound tubuloacinar gland (Fig. 4.2).
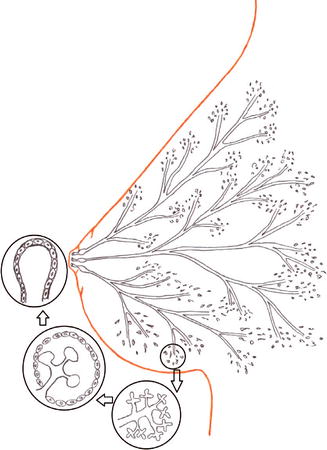
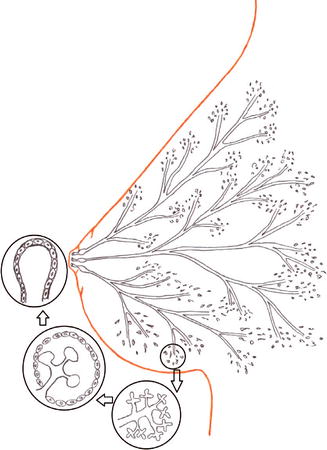
Fig. 4.2
Structure of the mammary gland. Model. The glandular body consists of many lobes, divided in numerous lobules ending in axinar formations, which consist of cylindrical or cubic cells located around a lumen
The mammary stroma consists of adipose tissue, the Cooper’s ligaments, vessels, and nerves. The adipose tissue is mostly located in the peripheral portions of the mammary gland, but it is also situated among the lobes and the glandular lobules; however, the retro-areolar region is devoid of adipose tissues (Fig. 4.3). The mammary stromal composition may change in a woman, as a consequence of a weight change or with advancing age. The Cooper’s ligaments are fibroelastic structures, stretched from the posterior side of the mammary gland to its anterior dermis. These ligaments allow the breast motion and represent the only suspensory apparatus of the mammary gland. The mammary gland sags when the Cooper’s ligaments become weaker (as a consequence of weight change or pregnancy); reinforcing exercises for the pectoral muscles will not suffice, and breast lift surgery is the only option. The space behind the breast is covered with the Chassaignac’s bursa. In very young women there are fibrous connections between the Chassaignac’s bursa and the aponeurosis of the chest-wall muscles; with advancing age such connections break forming a virtual space behind called Chassignac’s space. Mammary prostheses are placed in this area; they are therefore called retroglandular prostheses; retromuscular implants are placed behind the pectoralis major. The breast mainly lies on this muscle, which consists of a number of insertions located on the humerus, on the medial surface of the clavicle, on the lateral surface of the sternum, and on the anterior arches of the ribs, from the fifth to seventh rib; it contributes to the processes of inter-rotation, abduction, and flexion of the arm, but it does not have any function of support of the mammary gland. The pectoralis minor is located under the pectoralis major, and it does not directly touch the breast; it originates from the coracoid, and it inserts on the anterior arches of the ribs, from the third to sixth one. Other muscles that indirectly touch the breast are the external oblique muscle, which originates from the anterior ribs arches, from the seventh to tenth one, extending inferiorly and medially from the linea alba to the pubis; the serratus anterior muscle, which originates from the arches of the first ten anterior ribs, is inserted through three fascicles on the superior, medial, and inferior margins of the scapula.
Fig. 4.3
Anatomy of the mammary gland. Lateral view. The breast is supported by the pectoral muscle, with the Chassaignac’s bursa in the middle. The adipose tissue covers the periphery glandular tissue. Cb Chassaignac’s bursa, gl gland lobules, ld lactiferous ducts, pmm pectoralis major muscle
The vascular supply to the breasts is derived from the following arteries: the lateral thoracic (or external mammary) artery, a branch of the axillary artery, which supplies the superolateral portion of the gland and the nipple-areolar region; the internal mammary artery, which is a branch of the subclavian artery, passes along the intercostal spaces and sends perforating branches to the superomedial part of the mammary gland; and in conclusion, the branches of the posterior intercostal arteries, perforating branches that supply the inferior and posterior glandular part (Fig. 4.4). Such vessels, through multiple anastomoses, form three plexuses: the subdermal, pre-glandular, and retro-glandular plexuses. The veins also originate three plexuses, from which the blood laterally flows into the thoracoepigastric vein and then drains into the axillary artery; it flows medially into the internal mammary vein, which drains into the subclavian vein, but also into the veins of the neck and of the abdominal wall.
Fig. 4.4
Vascular supply of the mammary gland. Anatomy. The external mammary branch of the axillary and internal mammary arteries, which originate from the subclavian artery, provide the main blood supply to the mammary gland. aa axillary artery, ema external mammary artery, ima internal mammary artery, sa subclavian artery, lcb lateral cutaneous branches of the intercostal posterior arteries
The lymphatic system is very complex, since the subdermal and the parenchymal plexus overlap, and it is still not clear yet, whether or not they both flow into a single drainage system. Approximately 90 % of the entire lymph fluid drains into the axillary lymph nodes and the remaining part into those located outside the axilla, such as the internal mammary chain lymph nodes; we find intramammary lymph nodes iwn 20 % of cases (Fig. 4.5). The clinical practice divides the axillary lymph nodes into apical (or subclavicular) lymph nodes, medial to the pectoral muscle; external mammary nodes, located into the lateral part of the pectoralis major muscle; subscapular lymph nodes, extending along the course of the subscapular vessels; central lymph nodes, located in the center of the axilla (these lymph nodes are further divided in three levels, according to the theoric lymphatic flow direction). Rotter’s lymph node consists of 3–4 lymph nodes located between the pectoralis major and the pectoralis minor muscles. The subclavicular, the cervical, and the contralateral internal mammary lymph nodes are the subsequent lymphatic stations.
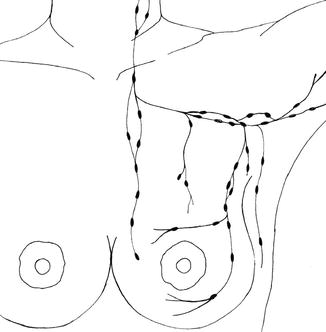
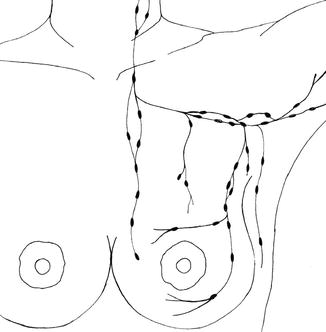
Fig. 4.5
Lymphatic drainage of the mammary gland. Model. Representation of the principal ways of the lymphatic flow
The mammary gland is very sensitive and highly innervated; the nerve system mostly consists of the supraclavicular nerves, located along the cervical plexus (between C3 and C4), which innervate the superior portion of the gland. The medial and lateral branches, which come from the thoracic nerves, innervate the remaining part of the breast (among the T2–T7). The 4th lateral branch of the thoracic nerve is responsible for the innervation of the nipple-areolar complex, and it is therefore important to pay special attention there during surgery.
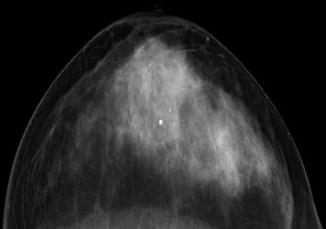
4.2 Normal Imaging Anatomy
4.2.1 Mammography
Mammography is currently the primary examination for a broad and complete study of the breast. The three main projections are the craniocaudal (CC) (Fig. 4.6), the mediolateral oblique (MLO) (Fig. 4.7), and the lateral view; they must include the four mammary quadrants, the areolar region, the axillary mammary extension, the inframammary fold, and the pectoral muscle.