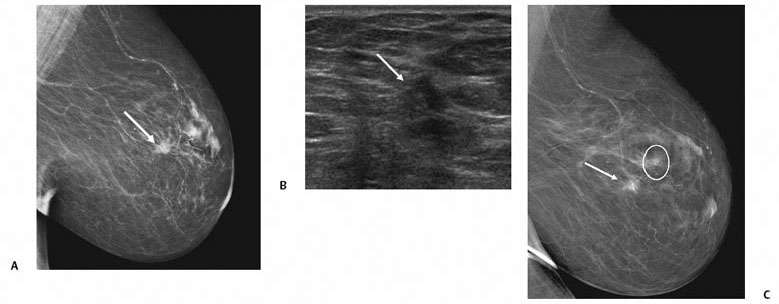
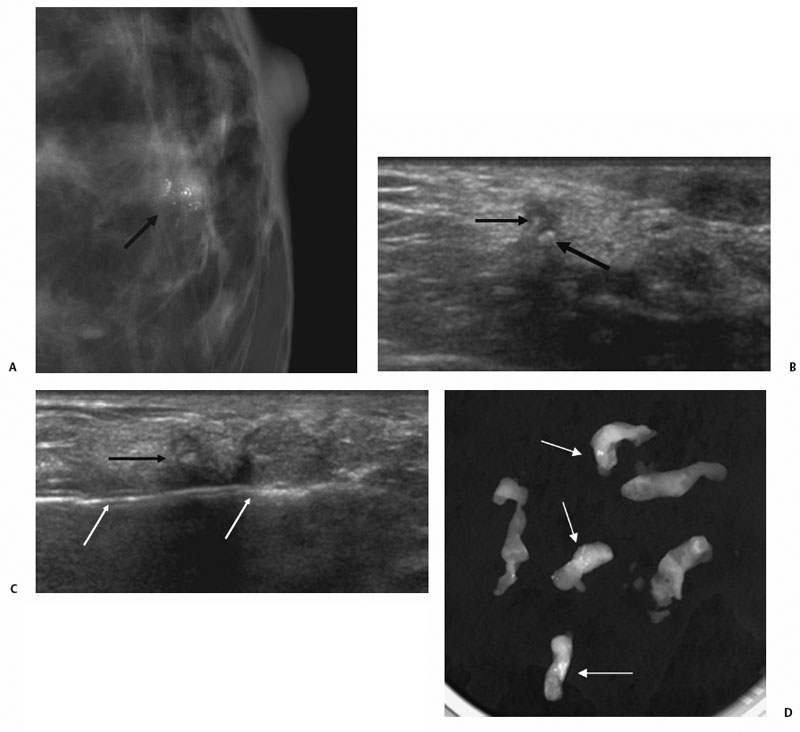
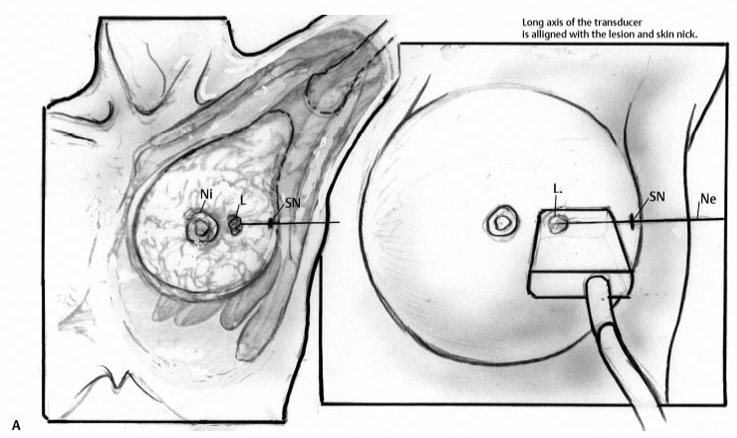
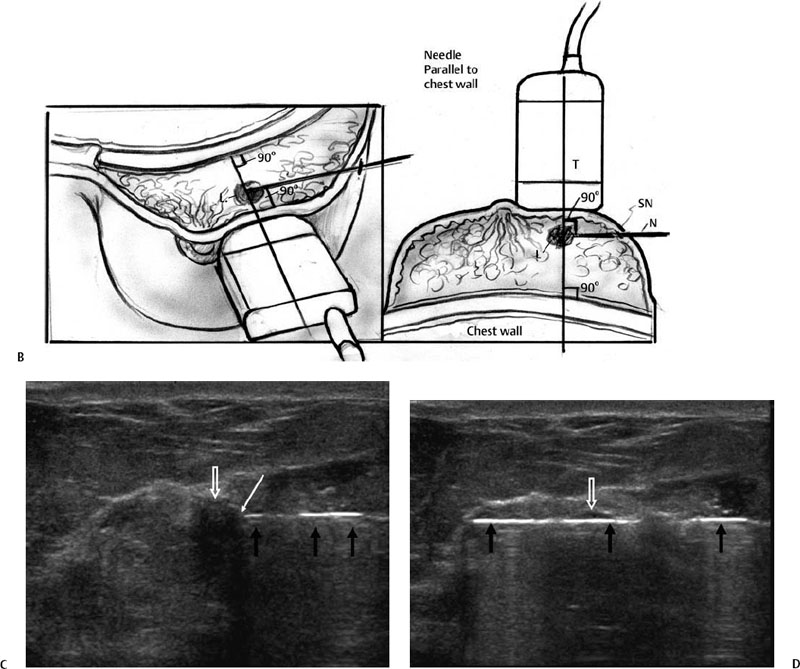
5 Breast Biopsy Percutaneous image-guided breast biopsy is less invasive, less expensive, and more efficient than diagnostic surgical biopsy. American College of Radiology (ACR) Practice Guidelines for performance of ultrasound-guided breast biopsy recommends that radiologists who are beginning to perform these procedures meet practice guidelines for performing breast ultrasound and obtain Advantages of image-guided preoperative diagnosis of breast cancer over diagnostic surgical biopsy: Other advantages of ultrasound guidance for breast CNB over stereotactic guidance include Percutaneous image-guided biopsy has largely replaced diagnostic surgical biopsy in the evaluation of breast lesions in many practices. Most breast lesions that are visible on ultrasound that are suspicious (Breast Imaging Reporting and Data System [BI-RADS] assessment category 4) or malignant (BI-RADS 5) are amenable to ultrasoundguided core needle biopsy. Image-guided biopsy is not typically performed for Some lesions will not be amenable to percutaneous biopsy. Of 630 breast cancers diagnosed over a 3-year period at Yale University, 17% were not diagnosed by percutaneous biopsy. The most commonly cited reasons were Although most masses identified on mammography can be identified on ultrasound for biopsy, lesions presenting as architectural distortion or calcifications on mammography may be more difficult to identify on ultrasound. If a lesion is much better visualized on mammography than ultrasound, then stereotactic-guidance may be the better choice to improve confidence that the correct area was sampled (Fig. 5.1). Fig. 5.1 A 67-year-old woman with abnormal right mammogram. (A) Right mediolateral (ML) view shows an 8-mm mass with spiculated margins (arrow). (B) Ultrasound shows a corresponding subtle hypoechoic solid mass in the right breast at 10 o’clock (arrow). (C) Postprocedure ML view shows that the clip (circle) is located ~2 cm from the lesion (arrow). Core biopsy was immediately repeated using stereotactic guidance. Histology from ultrasoundguided core needle biopsy (CNB) showed only stromal fibrosis, whereas the stereotactic-guided CNB showed ductal carcinoma in situ. In retrospect, stereotactic-guided CNB would likely have been a better choice initially because the finding was subtle on ultrasound. Should typically undergo sampling using stereotactic guidance, but can be identified and undergo biopsy using ultrasound in some cases. In a prospective study, Soo et al identified 23% of 111 lesions on ultrasound that presented as microcalcifications without a mass on mammography, and subsequently performed successful CNB using ultrasound. When calcifications were identified on ultrasound, lesions were more likely to be larger, malignant (69% versus 21%), and invasive when malignancy was diagnosed (72% versus 28%) than lesions not identified on ultrasound. Ultrasound-guidance can be a useful option when percutaneous biopsy using stereotactic guidance is not feasible (Fig. 5.2). Fig. 5.2 A 68-year-old woman with suspicious microcalcifications on mammography who underwent diagnostic ultrasound-guided core needle biopsy. Stereotactic-guided biopsy could not be performed due to small compressed breast thickness. (A) Craniocaudal magnification view of the left breast shows grouped heterogeneous calcifications (arrow). (B) The calcifications were visualized on ultrasound (arrows). (C) Ultrasound-guided vacuum-assisted biopsy was performed by placing the needle (white arrows) posterior to the calcifications (black arrow). (D) Specimen radiograph contains numerous calcifications (arrows). Histology revealed invasive ductal carcinoma and ductal carcinoma in situ. Contraindications to ultrasound-guided breast biopsy: Women who are not good candidates for stereotactic biopsy due to stroke or small breast size can usually undergo ultrasound-guided breast biopsy if the lesion is identified. The presence of a breast implant can increase the complexity of the approach, but is not necessarily a contraindication. Either automated throw needle (CNB) or vacuum-assisted (VAB) biopsy devices may be used for ultrasound-guided breast biopsy. VAB can be useful for selective cases: FNAB can be very useful in Prior to beginning the procedure, diagnostic breast imaging including any mammograms, ultrasound, and MR images should be reviewed. Fig. 5.3 Positioning of the transducer and biopsy needle. (A) The skin nick is made at the side of the breast in the same plane as the transducer. (B)
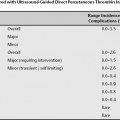
Classification
Initial Training
Indications
Microcalcifications
Ultrasound-Guided Biopsy of Abnormal Axillary Lymph Nodes
Axillary Adenopathy of Unknown Cause
Contraindications
Preprocedural Evaluation
Equipment
High-Frequency Linear Array Transducers
Needle Selection (Core versus Vacuum)
Core Needle Biopsy
Vacuum-assisted Biopsy
Fine-Needle Aspiration Biopsy
Room Setup
Preparation for Procedure
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree