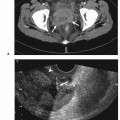
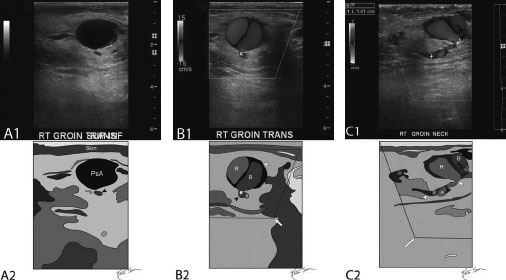
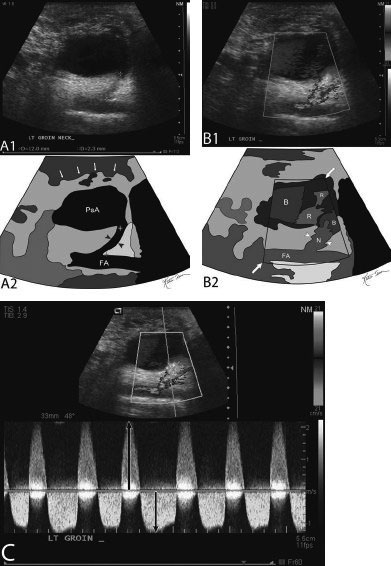
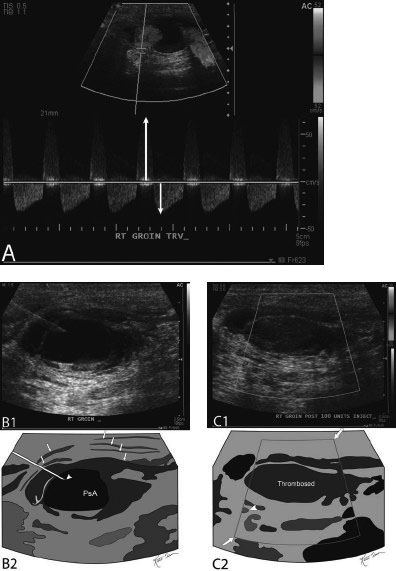
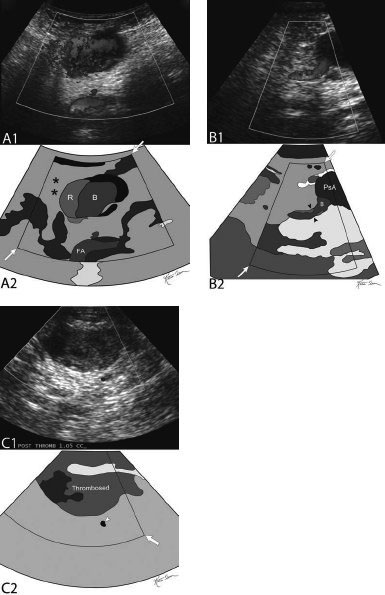
22 Management of Postcatheterization Pseudoaneurysm Arterial pseudoaneurysms are the most common complication (61%) of femoral artery catheterization and are associated with increased morbidity. The overall incidence of postcatheterization pseudoaneurysms ranges from 0.11 to 1.52%. The incidence of access of pseudoaneurysms increases with transcatheter therapeutic interventions (3.5–5.5%) compared with studies confined to diagnostic arterial catheterizations (0.1–1.1%). Due to the ongoing paradigm shift in transcatheter endoluminal interventions as opposed to traditional open surgical interventions, the incidence of postcatheterization pseudoaneurysms is on the rise with ~15,000 femoral pseudoaneurysms diagnosed in the United States annually as of the year 2000. Numerous methods, with variants within each method, for the management of postcatheterization pseudoaneurysms have been described. For the purposes of this chapter, the two most commonly described approaches (pseudoaneurysm compression and direct percutaneous thrombin injection) and their variant techniques will be discussed. Due to the high success rate and low complication rate (see below) with the risk–benefit ratio largely in favor of treatment, the indication for treatment of postcatheterization access pseudoaneurysms is broad and involves almost all patients. However, it is particularly indicated if the postcatheterization access pseudoaneurysms are The following are lists that describe the ideal features that make each patient/pseudoaneurysm ideal for either ultrasound-guided compression therapy or direct ultrasound-guided percutaneous thrombin injection. Poor candidates for compression represent ~10% of all patients and 50% of intent-to-treat technical failures. The contraindications to direct percutaneous thrombin injection therapy include Fig. 22.1 (A) Doppler ultrasound evaluation of a femoral pseudoaneurysm gray-scale ultrasound image (top) and schematic sketch (bottom) of a femoral pseudoaneurysm (PsA) demonstrating a hypoechoic spherical structure, which pulsates in real-time. The pseudoaneurysm (PsA) is superficial (under 1 cm from the overlying skin). (B) Doppler image (top) and schematic sketch (bottom; arrow pointing to Doppler box) of the same pseudoaneurysm as in Fig. 22.1A, showing the typical yin–yang appearance with half of the pseudoaneurysm coloring in red (R), and the other half in blue (B). (C) Doppler image (top) and schematic sketch (bottom; arrow pointing to Doppler box) of the same pseudoaneurysm as in Figs. 22.1A and 22.1B. The image is along the longitudinal axis of the pseudoaneurysm neck (between arrowheads). Again, the typical yin–yang appearance with half of the pseudoaneurysm coloring in red (R), and the other half in blue (B). Coloring of the pseudoaneurysm neck is also in red and blue (R and B, respectively). The pseudoaneurysm neck measures at least 1.4 cm in length. Fig. 22.2 (A) Gray-scale ultrasound image of a femoral pseudoaneurysm (PsA) (top) and schematic sketch (bottom) demonstrating a hypoechoic spherical structure, which pulsates in real-time. The image is along the longitudinal axis of the pseudoaneurysm neck (between arrowheads, and cursor crosses/calipers) and the femoral artery (FA). The pseudoaneurysm neck is also hypoechoic like the femoral artery and the pseudoaneurysm and measures 1.2 cm in length. (B) Doppler image (top) and schematic sketch (bottom; arrow pointing to Doppler box) of the same pseudoaneurysm as in Fig. 22.2A, showing the yin–yang appearance with half of the pseudoaneurysm coloring in red (R), and the other half would be colored blue (B). The image is along the longitudinal axis of the neck (N: in between arrowheads), which exhibits aliasing. Also note the injured femoral artery. (C) Doppler spectral waveform analysis sampling at the neck demonstrating bidirectional high velocity flow. In one direction (above the line), flow is in excess of 220 cm/second and in the other direction (below the line) flow is in excess of 120 cm/second. Fig. 22.3 (A) Direct percutaneous thrombin injection of a femoral pseudoaneurysm. Doppler spectral waveform analysis sampling at the neck of a pseudoaneurysm demonstrating bidirectional high-velocity flow. In one direction (above the line), flow is in excess of 60 cm/second and in the other direction (below the line) flow is in excess of 30 cm/ second. (B) Gray-scale ultrasound image (top) and schematic sketch (bottom) during needle placement into the pseudoaneurysm (PsA). The needle tip is seen in the hypoechoic pseudoaneurysm (PsA). Arrows point to the different layers of the pseudoaneurysm and the compression of surrounding tissue plains. (C) Doppler image (top) and schematic sketch (bottom; arrows pointing to Doppler box) of the same pseudoaneurysm as in Figs. 22.3A and 22.3B, demonstrating no color/flow in the pseudoaneurysm. This indicates successful treatment of the pseudoaneurysm. The arrowhead points to an adjacent vessel with color/flow within it. Fig. 22.4 (A) Doppler image (top) and schematic sketch (bottom; arrows pointing to Doppler box) showing the yin–yang appearance with half of the femoral pseudoaneurysm coloring in red (R), and the other half colored blue (B). Also note the injured femoral artery (FA). The area of mottled coloring (labeled as *) is due to motion from the pulsation and thrill/vibration of the adjacent pseudoaneurysm. (B) Doppler image (top) and schematic sketch (bottom; arrows pointing to Doppler box) of the same pseudoaneurysm (PsA) as in Fig. 22.4A. The image is along the longitudinal axis of the neck (between arrowheads), which exhibits blue coloring (B). (C) Doppler image (top) and schematic sketch (bottom; arrows pointing to Doppler box) of the same pseudoaneurysm as in Figs. 22.4A and 22.4B, demonstrating no color/flow in the pseudoaneurysm. This indicates successful treatment of the pseudoaneurysm. The arrowhead points to an adjacent vessel with color/flow within it.
Classification
Indications
Pseudoaneurysm Compression
Direct Percutaneous Thrombin Injection
Contraindications
Pseudoaneurysm Compression
Direct Percutaneous Thrombin Injection
Preprocedural Evaluation
Evaluate Prior Cross-Sectional Imaging
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree