Fig. 14.1
A forward-planned intensity-modulated radiation therapy (IMRT) plan (left) vs. a conventional wedge plan (right)

Fig. 14.2
A 107 % isodose cloud (blue) visible on a digitally reconstructed radiograph (DRR)

Fig. 14.3
A 105 % isodose cloud (green) visible on a digitally reconstructed radiograph (DRR)
Limitations of forward-planned IMRT are the constraints associated with using just two gantry positions with medial and lateral tangentially oriented fields. Comprehensive irradiation of the regional lymphatics of the internal mammary, axillary, and supraclavicular regions is often not possible with this technique, and it is ideally suited for treatment that includes only the breast.
14.3 Inverse-Planned IMRT
Over the past decade, the general term IMRT has been used to refer to inverse planning of radiation therapy involving the use of either multiple, non-coplanar fixed gantry positions or, more recently, a continuous photon arc. Such techniques can result in far more complex and homogenous dose distributions than forward-planned IMRT, which offers some advantages when treating lymphatics in the internal mammary, axillary, and supraclavicular regions owing to the non-coplanar orientation of the beams or arcs used. A disadvantage of inverse-planned IMRT is that the multiple-beam geometry results in higher doses to both superficial and deep tissues outside the target volume, such as the lung and contralateral breast. The clinical implications of these high-dose exposures are unclear, but scattered dose to the uninvolved breast during radiation therapy could result in the development of breast cancer [1, 10] or lung cancer [19, 31] in smokers. As a result, the benefits of the improved conformality and homogeneity of inverse-planned IMRT should be balanced against the risk of additional scattered radiation to normal structures when inverse-planned IMRT is used. Inverse-planned IMRT is best reserved for specific cases where more conventional techniques such as forward-planned IMRT are unable to cover regions at risk and should probably not be used routinely, especially in cases where only the breast is being treated.
14.3.1 Avoiding the Heart
Inverse-planned IMRT can result in treatment plans that can avoid the heart in patients with left-sided breast cancer (Fig. 14.4). A deep inspiratory breath-hold technique [23] should be used to minimize target motion during therapy, in addition to pulling the chest wall away from the heart as much as possible. The dose to the heart should be thoroughly minimized. Although the optimal dose-volume histogram parameters have not been clearly defined, a reasonable guideline would be a mean dose to the entire muscular heart of <5 Gy [6].


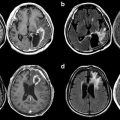
Fig. 14.4
An inverse-planned IMRT plan for a patient with a reconstructed breast that avoids the heart while treating the internal mammary chain of lymphatics
14.3.2 Treatment of Regional Lymphatics
The lymphatic regions at risk in patients with breast cancer include the axillary, infraclavicular, supraclavicular, and internal mammary chains. Evidence is evolving that comprehensive treatment of the lymphatics may be of benefit for patients with high-risk disease [28]. Traditionally the lymphatics of the breast were treated with multiple abutting photon or electron fields (Fig. 14.5), usually matched on the skin. These techniques often resulted in underdosing at the field junctions. IMRT can eliminate underdosing at these regions (Figs. 14.6 and 14.7), at the expense of higher doses to the lung and contralateral breast in some cases. Several detailed contouring atlases have been published [20, 29], and some general principles of nodal contouring are described below.




Fig. 14.5
Abutting photon and electron fields used to treat a patient after mastectomy

Fig. 14.6
An underdosed region in the internal mammary chain

Fig. 14.7
Elimination of the underdosed region in the internal mammary chain with IMRT
14.3.2.1 Internal Mammary Lymphatics
The internal mammary artery and vein should be contoured within the first three ipsilateral rib interspaces, starting at the superior aspect of the ipsilateral, medial first rib and extending to the cranial aspect of the ipsilateral, medial, fourth rib (Fig. 14.8).


Fig. 14.8
The location of the internal mammary lymphatics
14.3.2.2 Level I of the Axilla
Level I of the axilla should be contoured starting at the level where the axillary vessels cross the lateral edge of the pectoralis minor muscle superiorly and extending inferiorly to the insertion of the pectoralis minor muscle on the ribs. The medial and lateral borders extend between the medial border of the latissimus dorsi muscle and the lateral border of the pectoralis minor muscle, respectively. The anterior border is the anterior surface of the pectoralis major muscle, and the posterior border should be the anterior surface of the subscapularis muscle (Fig. 14.9).


Fig. 14.9
Axillary contours. Red, level II; orange, level I
14.3.2.3 Level II of the Axilla
Level II of the axilla should be contoured at the level where the axillary vessels cross the medial edge of the pectoralis minor muscle superiorly, extending inferiorly to the cranial edge of level I of the axilla (where the axillary vessels cross the lateral edge of the pectoralis minor muscle). The medial and lateral borders extend between the medial border of the pectoralis minor muscle and the lateral border of the latissimus dorsi muscle, respectively. The anterior border is the anterior surface of the pectoralis minor muscle and the posterior borders are the ribs and intercostal muscles (Fig. 14.10).


Fig. 14.10
Axillary contours. Blue, level III; red, level II; orange, level I
14.3.2.4 Level III of the Axilla
Level III of the axilla should be contoured at the level of the insertion of the pectoralis minor muscle on the coronoid process superiorly, extending inferiorly to the cranial edge of level II of the axilla (where the axillary vessels cross the medial edge of the pectoralis minor muscle). The medial and lateral borders extend from the thoracic inlet to the medial border of the pectoralis minor muscle, respectively. The anterior border is the posterior surface of the pectoralis major muscle, and the posterior borders are the ribs and intercostal muscles (Fig. 14.11).


Fig. 14.11
Axillary contours. Blue, level III; red, level II
14.3.2.5 Supraclavicular Lymphatics
The lymphatics of the supraclavicular region should be contoured at the inferior border of the cricoid cartilage superiorly, extending inferiorly to the caudal edge of the clavicular head. The medial and lateral borders should be the edge of the thyroid gland and trachea and the lateral edge of the sternocleidomastoid muscle, respectively. The anterior border is the posterior surface of the sternocleidomastoid muscle, and the posterior border is the anterior surface of the scalene muscles (Fig. 14.12).


Fig. 14.12
Contours of the supraclavicular region
14.3.3 Treatment of the Breast and Tumor Bed
Treating the intact breast with inverse-planned IMRT involves contouring the entire breast mound on CT images. Breast mounds vary considerably between patients depending on body habitus and positioning; common sense should be used when contouring this structure, but some general guidelines are as follows: The breast mound often extends from the region between the clavicular head and second rib insertion superiorly and extends inferiorly to a variable degree. The medial border is typically at the junction of the sternum and the ribs, and the lateral junction should be determined clinically. In patients with early-stage disease who have not received neoadjuvant therapy and who have tumors that do not approximate the pectoralis muscles, the posterior border should be at the anterior border of the pectoralis major muscle. Otherwise, the posterior border should be at the pleural surface and include the ribs and pectoralis muscles. The skin surface should constitute the anterior border. The tumor cavity should comprise the entire visible postoperative seroma seen on CT and should be included in its entirety within the breast contours. The placement of surgical clips at the time of lumpectomy can assist in delineating the tumor cavity if the seroma is not visible on CT and constitutes best practice when using IMRT to treat the breast. Use of an integrated boost [24, 26] can shorten treatment time through the administration of a higher dose per fraction to the tumor bed concurrently with treatment of the breast, with acceptable cosmetic results [18].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree