Fig. 10.1
A 63-year-old former smoker presented with a 3.5 cm painful mass of the left lateral border of the oral tongue (photograph). Biopsy of this mass showed moderately differentiated, invasive squamous carcinoma. Contrast-enhanced diagnostic CT of the neck (with puffed-cheek technique) demonstrated the primary mass (outlined in green) and revealed a radiographically positive lymph node in left level IIa due to peripheral enhancement and central hypodensity (arrow). There were no metastases on chest X-ray. Clinical stage was T2N1M0. He underwent primary surgical resection, including left partial glossectomy, left modified radical neck dissection (levels Ia through IV), and radial forearm free flap reconstruction of the left lateral tongue defect. Final surgical pathology revealed a 3.5 cm primary tumor, closest surgical margin was 2.0 cm, and there was no perineural or lymphovascular invasion. Two of 6 and 2 of four lymph nodes were positive for carcinoma in left neck levels Ib and IIa, respectively, each with extracapsular spread. The remainder of the left neck lymph nodes (levels IIb, III, and IV) were negative for carcinoma. Final pathologic stage was T2N2b. He was treated with postoperative chemoradiation (concurrent cis-platinum) using IMRT. Representative axial, sagittal, and coronal views from planning CT are shown. The primary tumor bed, free flap, and its attachments to the native tongue and positive neck levels (I and IIa) plus ~ 1 cm were delineated as high-risk CTV (CTV 60 Gy). The remainder of the oral tongue and operative bed of the left neck were treated to 57 Gy (intermediate risk), and the contralateral neck levels I–IV were treated electively to 54 Gy (standard risk). This was accomplished in a single integrated IMRT plan in 30 fractions. Representative isodose distributions are shown in multiple axial planes.
Case 1 Key Technical Points
1.
At the time of simulation, the left neck suture line/surgical scar was marked with CT-compatible radiopaque wire, and 3 mm bolus was placed over the scar to ensure adequate surface dose to the scar. The left neck CTV contours were inclusive of the operative bed and surgical tracts and were taken out to the skin surface at the level of the scar.
2.
A customized mouth-opening and tongue-depressing/tongue-immobilizing intraoral stent was used in this case. As demonstrated in the sagittal view, this provided physical separation of the tongue from the nontarget upper lip and hard palate.
3.
In cancers of the oral tongue, in addition to targeting of the primary site tumor bed, we typically treat the remainder of the involved organ (entirety of the oral tongue) to operative bed or elective doses.
4.
As demonstrated in the sagittal and coronal views, we ensured the CTVs were carried through the adjacent floor of the mouth, root of tongue, and submental region to the level of the hyoid.
5.
The contralateral undissected (right) neck was treated electively to 54 Gy. The CTV for this unviolated/unoperated neck differed from that of the operated left neck, in that the right neck lymph node levels were delineated restricted by their anatomic boundaries (e.g., deep surface of the sternocleidomastoid and platysma), while in the left neck, the entirety of the sternocleidomastoid muscle was targeted as part of the operative bed target volume.
Case 2 (Fig. 10.2)
Fig. 10.2
A 65-year-old former smoker presented with a 4.0 cm painful expansile mass of the left lower alveolus (photograph). Biopsy of this mass showed poorly differentiated, invasive squamous carcinoma. Contrast-enhanced diagnostic CT of the neck (with puffed-cheek technique) demonstrated the primary mass interdigitated with multiple teeth and bone erosion (outlined in green). There were lymph node metastases seen on CT. There were no metastases seen on chest X-ray. Clinical stage was T4aN0M0. He underwent primary surgical resection, including left segmental mandibulectomy, left modified radical neck dissection (levels Ia through IV), and osseocutaneous fibular free flap reconstruction. Final surgical pathology revealed a 4.2 cm primary tumor with bone involvement, closest surgical margin was 1.0 cm, and there was perineural and lymphovascular invasion. One of 4 lymph nodes was positive for carcinoma in left neck level Ib, with extracapsular spread. The remainder of the left neck lymph nodes (levels IIa/b, III, and IV) were negative for carcinoma. Final pathologic stage was T4aN1. He was treated with postoperative chemoradiation (concurrent carboplatinum rather than cis-platinum due to profound baseline hypoacusis) using IMRT targeting the tumor bed, operative bed, and ipsilateral neck. A representative axial planning CT image with CTVs is shown. The primary tumor bed, free flap and its attachments, and positive neck level (Ib) plus margin were delineated as high-risk CTV (CTV 60 Gy). The remainder of the operative bed of the left neck and segment of the inferior alveolar nerve were treated to 57 Gy (intermediate risk). The left level Ib (area of ECE) was boosted to 66 Gy. This was accomplished in a single integrated IMRT plan in 30 fractions. Representative isodose distributions are shown in axial and sagittal plane.
Case 2 Key Technical Points
1.
A customized mouth-opening and tongue-deviating intraoral stent was used in this case in order to displace the tip of the oral tongue, upper lip, and upper gingiva from the high-dose region.
2.
The primary tumor bed, flap and its attachments, and bony cuts of the mandible were included in the CTV 60 Gy.
3.
Given microscopic perineural invasion, the inferior alveolar nerve was targeted; the most proximal aspect of nerve coverage was to the interspace of the medial and lateral pterygoid muscles.
4.
Given the surgical exposure associated with mandibulectomy and neck dissection, the tail of the left parotid was included in the operative bed target (CTV 57 Gy), as recurrences near a spared parotid in a pathologically involved neck have been described (10).
Case 3 (Fig. 10.3)
Fig. 10.3
A 63-year-old former smoker presented with a painful 1.7 cm mass centered in the right floor of the mouth, which was crossing midline (see photograph). Contrast-enhanced diagnostic CT of the neck demonstrated the primary mass (outlined in green) close to but not invading an adjacent mandibular torus. There were no lymph node metastases seen on CT. There were no metastases seen on chest X-ray. Clinical stage was T1N0M0. He underwent resection of the anterior floor of the mouth and bilateral neck dissection (levels II–IV) with radial forearm free flap reconstruction of the oral defect. Final pathology showed a 1.2 cm moderately differentiated tumor, 0.6 cm depth of invasion, no perineural or lymphovascular invasion, and free margins. There was a single lymph node involved in right level IB (without extracapsular extension) and a focus of metastatic carcinoma in the right submandibular gland, suspected to be direct spread down Wharton’s duct. He was treated with postoperative IMRT. Representative axial, sagittal, and coronal views from planning CT with CTVs are shown. The primary tumor bed, floor of the mouth, free flap and its attachments, and submandibular triangle plus margin were delineated as high-risk CTV (CTV 60 Gy). The remainder of the uninvolved operated bilateral neck above the junction was treated to 57 Gy (intermediate risk). Representative axial, sagittal, and coronal views from planning CT are shown with CTVs in color wash with accompanying dose distributions.
Case 3 Key Technical Points
1.
A customized mouth-opening and tongue-elevating intraoral stent was used in this case in order to displace the mobile tongue, upper lip, and upper gingiva from the floor of the mouth.
2.
For maximal, inferior constrictor muscle, larynx, and esophageal inlet sparing, a split-field IMRT technique utilizing half-beam block was used with the isocenter placed just above the arytenoids. The lower neck and supraclavicular fossae were treated using a low anterior neck field with a larynx block, which was extended to a full midline block after 40 Gy. Total dose to the bilateral midneck below the junction was 56 Gy in 28 fractions. A patched low-energy electron field was used to treat the central aspect of the neck surgical scar that fell under the larynx and full midline block.
Case 4 (Fig. 10.4)
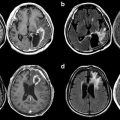
Fig. 10.4
As 58-year-old smoker presented with hoarseness of voice and globus sensation. Biopsy of an anterior glottic mass revealed invasive squamous carcinoma. Contrast-enhanced CT neck demonstrated an enhancing mass in the anterior larynx, with full-thickness cartilage erosion with invasion of the anterior neck soft tissues (outlined in green). Bilateral cervical lymphadenopathy was seen (white arrows). There were no metastases on CXR. Final clinical stage was T4aN2cM0. He underwent total laryngectomy, with total thyroidectomy, and bilateral modified radical neck dissection and bilateral paratracheal dissections. Final pathology showed cartilage destruction and anterior soft tissue invasion, and surgical margins were free. There was multilevel adenopathy in the right neck with multiple positive nodes in levels II and III and a single involved node in left level II and with extracapsular spread of all positive nodes. He was treated with postoperative IMRT with concurrent cis-platinum. The tumor bed, larynx bed, reconstructed neopharynx and anastomosis, and bilateral positive nodal levels were treated to 60 Gy in 30 fractions. The remainder of the operative bed was treated to 57 Gy. Axial and sagittal planning CT images with CTVs and corresponding dose distributions are shown.
Case 4 Key Technical Points
1.
At the time of simulation, the surgical scar was marked with CT-compatible radiopaque wire, and 3 mm bolus was placed over the scar both during simulation and treatment to ensure adequate surface dose to the scar and surgical tract.
2.
Given anterior soft tissue invasion and multilevel adenopathy with extracapsular extension, generous HR-CTV delineation was pursued and generously included the anterior neck soft tissues, the entirety of the central compartment, positive nodal levels, and suprastomal region.
3.




The tracheostoma was included in the lower-dose CTVs in this case. We consider including the stoma in the IR-CTV if there was extensive subglottic disease, narrow subglottic surgical margin, or low neck soft tissue invasion such as low neck nodes with extracapsular spread and in the HR-CTV if the location of the stoma is adjacent to preoperative disease. The risk of this location harboring disease is balanced with the risk of microstomia, which can be a severe late effect.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree