Fig. 3.1
Relative surviving fractions of EMT6 and SCCVII cells after 8 Gy given without a break or in 5 fractions at various intervals. Cell survival after continuous 8-Gy irradiation was regarded as 1. Bars represent SD (Reproduced from Ref. [10] with permission from the publisher)
Furthermore, the effects of 2 Gy given in 5 or 10 fractions at intervals of 0.5–5 min were estimated in EMT6 cells using the cytokinesis-block micronucleus assay, which is a sensitive assay to evaluate radiation effects at low doses [13, 14]. In the 5-fraction experiment, the micronucleus frequency decreased significantly as compared to single 2-Gy irradiation when the interval was 2 min or longer (Fig. 3.2). When the interval was 5 min, 5 fractions of 0.4 Gy corresponded to a single dose of 1.72 Gy. In the 10-fraction experiment, the micronucleus frequency decreased when the interval was 1 min or longer. With an interval of 3 min each, 10 fractions of 0.2 Gy corresponded to a single dose of 1.76 Gy.


Fig. 3.2
Relative micronucleus frequency in EMT6 cells after 2 Gy given without a break or in 5 or 10 fractions at various intervals. The micronucleus frequency after continuous 2-Gy irradiation was regarded as 1. Bars represent SD (Reproduced from Ref. [10] with permission from the publisher)
To summarize this in vitro study, it was concluded that dose-modifying factors of 1.08–1.16 need to be considered when the total irradiation time is 20–30 min. However, further in vivo study is considered necessary to extrapolate this result to clinical situations.
3.2.2 Influence of the Fraction Dose and Number and Dose Rate on the Biological Effect
The next in vitro study was conducted to investigate the effects of intermittent irradiation like IMRT [15]. A total dose of 8 Gy was given to EMT6 and SCCVII cells in 2, 5, 10, 20, and 40 fractions within a fixed period of 15, 30, or 46 min, and the effects were compared with continuous 8-Gy irradiation given at a dose rate of 1.55 Gy/min or at reduced dose rates over 15, 30, or 46 min. The 20- and 40-fraction schedules would be closer to the IMRT situation than other irradiation schedules. When the total radiation time was 15 min, there were no differences in cell survival among the fractionation schedules, but when the period was 30 or 46 min, the radiation effect tended to decrease with an increase in the fraction number up to 20 fractions (Fig. 3.3). Two-fraction irradiation yielded the greatest effect among the fractionated radiation groups. Continuous low-dose-rate irradiation had a greater effect than 20- or 40-fraction irradiation. Implications regarding the clinical application of these results are complicated; nevertheless, this study showed that biological effects could differ with the fractionation schedule even when the total radiation time and dose are identical. Judging from the in vitro study, intermittent irradiation as used in IMRT seems to be less effective than continuous irradiation, and to minimize the decrease of biological effects, total irradiation time should be kept as short as possible.


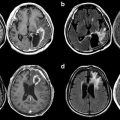
Fig. 3.3
Relative surviving fractions of EMT6 and SCCVII cells after 8 Gy given in 2–40 fractions and prolonged continuous irradiation given over 46 min. The control group received a single dose of 8 Gy over 5.3 min. Cell survival of the control group was regarded as 1. Bars represent SD (Reproduced from Ref. [10] with permission from the publisher. Regarding differences between groups, see Ref. [15])
3.2.3 Effects of Intermittent Irradiation on Murine Tumors In Vivo
The effect of prolonged radiation delivery was also studied in vivo [16]. EMT6 and SCCVII tumors were transplanted into the hind legs of Balb/c and C3H/HeN mice, respectively. When subcutaneous tumors grew to 1 cm in their longest diameter, the mice received 20 Gy in 2, 5, or 10 fractions at various intervals. Within 24 h from the first irradiation, the tumors were excised, minced, and enzymatically disaggregated into single cells. Then, cell survival was assessed using a colony assay. Figure 3.4 shows the results of a 5-fraction experiment. Contrary to the in vitro data, no decrease in radiation effects was observed; instead, by placing 2.5-, 7.5-, 10-, or 15-min intervals for EMT6 tumors and 2.5-, 5-, 7.5-, or 15-min intervals for SCCVII tumors, the effect became stronger. Similar results were obtained in 10-fraction experiments. It was speculated that SLDR in vivo might be counterbalanced or overweighed by other phenomena such as reoxygenation. Therefore, we investigated reoxygenation in SCCVII tumors during intervals of several minutes in the next study.


Fig. 3.4
Relative surviving fractions of EMT6 and SCCVII cells irradiated in vivo at 16, 18, or 20 Gy without a break or 20 Gy in 5 fractions at various intervals. Cell survival after continuous 20-Gy irradiation was regarded as 1. Bars represent SD Reproduced from Ref. [10] with permission from the publisher)
3.2.4 Reoxygenation Shortly After Irradiation and SLDR In Vivo in the Absence of Reoxygenation
Using 1-cm-diameter SCCVII tumors transplanted into C3H mice, reoxygenation at 0–15 min after a 13-Gy dose was investigated [17]; the hypoxic fraction was measured at 0, 2.5, 5, 10, and 15 min after 13 Gy using a paired survival curve assay. At given times, the irradiated mice were divided into alive and dead groups and received a second irradiation with 15 Gy. Cell survival in the two groups was compared to assess the hypoxic fraction. As shown in Fig. 3.5, the hypoxic fraction was 100 % at 0 and 2.5 min after the end of the first irradiation, but, at 5 min, it fell to 67 % (95 % confidence interval, 41–93 %). Thus, reoxygenation was observed at 5 min after irradiation. It was suggested that rapid reoxygenation could compensate for SLDR in vivo.


Fig. 3.5
Relative surviving fractions of SCCVII tumor cells after a priming dose of 13 Gy and a second dose of 15 Gy given at 0–15 min intervals to air-breathing (○) or dead (●) mice. The surviving fraction in the dead group that received the second dose immediately after the priming dose was regarded as 1. The hypoxic fraction is given by the surviving fraction of tumor cells in air-breathing mice divided by that in dead mice at respective time points. Bars represent SE (Reproduced from Ref. [10] with permission from the publisher)
To investigate the effect of intermittent irradiation under conditions of restricted reoxygenation, 1-cm-diameter SCCVII tumors in the hind legs of C3H mice were irradiated with the leg fixed using adhesive tape. This procedure was considered to increase the hypoxic fraction and restrict reoxygenation [18]. Figure 3.6 compares the growth delay of SCCVII tumors irradiated with 20 Gy, 25 Gy, or 5 fractions of 5 Gy given at 3-, 6-, or 10-min intervals. The effect of radiation decreased by imposing intervals of 3–7 min; the effect of 25 Gy given in 5 fractions was between that of 20 Gy and that of 25 Gy delivered continuously. Therefore, it was suggested that the effects of intermittent radiation in vivo decrease due to SLDR when reoxygenation is restricted.


Fig. 3.6
Relative volumes of SCCVII tumors after 20 (▲) or 25 (●) Gy given as a single dose or 5 fractions of 5 Gy given at intervals of 3 (○), 6 (■), or 10 (□) minutes. △: no irradiation. Tumor volumes before irradiation in each group were regarded as 100 %. Bars represent SE (Reproduced from Ref. [10] with permission from the publisher)
3.2.5 Other Laboratory Studies on the Biological Effects of Intermittent Irradiation
Classically, Elkind and his coworkers [3, 4] were the first to report the SLDR phenomenon. In their experiments, a significant increase in cell survival was observed when intervals of 30 min or longer were set between two radiation doses. However, they never investigated shorter intervals. With the development of radiotherapy techniques, it has become necessary to investigate the influence of radiation interruptions of shorter than 30 min.
After the 1990s, Benedict et al. [19] attempted to estimate dose correction factors for stereotactic radiosurgery using U-87MG cells in vitro. In their experiments, the effect of radiation decreased with prolongation of the treatment time, and the correction factor of 0.02–0.03 Gy/min was proposed when a total dose of 6–18 Gy was given. This indicates that when the treatment time prolongs by 30 min, 8 Gy would correspond to approximately 7.1–7.4 Gy delivered continuously, giving dose-modifying factors of 1.08–1.13. These results appear to agree with our own. Mu et al. [20] conducted an in vitro study with V79 cells using much more complicated fractionation schedules than those we employed and compared the surviving fraction ratios between the continuous and prolonged delivery of radiation with those estimated by biological models derived from the LQ model. Their conclusion was that the biological models underestimated the effect of prolonging the fraction time when a total dose of 2 Gy was fractionated. Therefore, estimation of the influence of prolonging the treatment time using biological models alone seems to be insufficient in clinical practice. More recently, Zheng et al. [21] investigated the impact of prolonged fraction delivery times simulating IMRT on two cultured nasopharyngeal carcinoma cell lines. The fraction delivery time was 15, 36, or 50 min. The dose-modifying factor for a fraction dose of 2 Gy was 1.05 when the delivery time was 15 min, but it increased to 1.11 or 1.18 when the time prolonged to 50 min. They emphasized, however, that these results do not necessarily hold in vivo. Moiseenko et al. [22] obtained results similar to those of the abovementioned studies and suggested that DNA repair underlies the increase in cell survival observed when dose delivery is prolonged, based on measurement of the retention of gammaH2AX, a measure of the lack of DNA damage repair.
Moiseenko et al. [23] investigated the correlation between the magnitude of the loss of effect brought about by prolonged radiation delivery and the α/β ratio in three cell lines. When their results were projected to a 30-fraction treatment, the dose deficit to bring cell survival to the same level was 4.1 Gy in one line, but it was as large as 24.9 and 31.1 Gy in the other two lines. The dose deficit did not relate to the α/β ratio of the three cell lines. On the other hand, Zheng et al. [24] also investigated the issue in two hepatocellular carcinoma cell lines, and a significant decrease in cell survival due to prolonged fraction delivery was observed in one line with an α/β ratio of 3.1 Gy but not in another with an α/β ratio of 7.4 Gy. Therefore, the relationship with the α/β ratio remains unclear and requires further investigation.
All these results indicate that SLDR certainly takes place when radiation delivery is prolonged or given intermittently in daily stereotactic irradiation and IMRT settings. However, it should be noted that these results were obtained using in vitro single cells. Until recently, there have been no in vivo studies except for our own ones, but other studies have been published. The results of a study by Wang et al. [25] agree with our own; when C57BL mice bearing Lewis lung cancer were irradiated under conditions of limited reoxygenation, intermittent radiation delivery led to a significant reduction in the biological effects. The study by Jiang et al. [26] also showed a similar result. However, more in vivo investigations appear to be warranted in the near future. Our study suggests that SLDR in vivo can be counterbalanced by reoxygenation. In tumors that reoxygenate rapidly, therefore, the adverse effects of prolonging the radiation delivery time may be none or negligible. However, little is known about the reoxygenation of tumors in humans, so this issue is also an important topic to be investigated in the future to elucidate the effect of intermittent or prolonged radiation delivery in clinical practice.
3.3 Applicability of the LQ Model to High-Dose-per-Fraction Radiotherapy
3.3.1 Current Controversy
To compare different fractionation schedules, the LQ formalism (![$$ {n}_2{d}_2/{n}_1{d}_1=\left(1+{d}_1/\left[\alpha /\beta \right]\right)/\left(1+{d}_2/\left[\alpha /\beta \right]\right) $$](http://radiologykey.com/wp-content/uploads/2017/06/A318890_1_En_3_Chapter_IEq1.gif) (where d 1 and d 2 are fractional doses and n 1 and n 2 are fraction numbers) and the biologically effective dose (BED) derived from the LQ model (BED = D(1 + d/[α/β]), where D is the total dose and d is the fractional dose) are often used because of their convenience and simplicity [10, 27]. While LQ formalism is useful for conversion between relatively low radiation doses as used in conventional radiotherapy, it has been suggested that it is not applicable to higher daily doses or smaller fraction numbers [9, 10]. However, many clinicians have used LQ formalism to convert hypofractionated doses to single doses in their publications [28, 29], and many have used BED to evaluate the doses of stereotactic irradiation [30, 31]. To further complicate the issue, some investigators, in contrast, claim that the LQ model is applicable to stereotactic irradiation [32, 33]. The ground for the latter group is somewhat limited in that the existing clinical data do not significantly deviate from those expected from LQ model calculations, and their data do not necessarily indicate that the LQ model fits best to the high-dose data. Since clinical data usually contain many errors, experimental evaluation of the reliability of the LQ model in single-fraction and hypofractionated radiation schedules appears to be important and desirable.
(where d 1 and d 2 are fractional doses and n 1 and n 2 are fraction numbers) and the biologically effective dose (BED) derived from the LQ model (BED = D(1 + d/[α/β]), where D is the total dose and d is the fractional dose) are often used because of their convenience and simplicity [10, 27]. While LQ formalism is useful for conversion between relatively low radiation doses as used in conventional radiotherapy, it has been suggested that it is not applicable to higher daily doses or smaller fraction numbers [9, 10]. However, many clinicians have used LQ formalism to convert hypofractionated doses to single doses in their publications [28, 29], and many have used BED to evaluate the doses of stereotactic irradiation [30, 31]. To further complicate the issue, some investigators, in contrast, claim that the LQ model is applicable to stereotactic irradiation [32, 33]. The ground for the latter group is somewhat limited in that the existing clinical data do not significantly deviate from those expected from LQ model calculations, and their data do not necessarily indicate that the LQ model fits best to the high-dose data. Since clinical data usually contain many errors, experimental evaluation of the reliability of the LQ model in single-fraction and hypofractionated radiation schedules appears to be important and desirable.
![$$ {n}_2{d}_2/{n}_1{d}_1=\left(1+{d}_1/\left[\alpha /\beta \right]\right)/\left(1+{d}_2/\left[\alpha /\beta \right]\right) $$](http://radiologykey.com/wp-content/uploads/2017/06/A318890_1_En_3_Chapter_IEq1.gif) (where d 1 and d 2 are fractional doses and n 1 and n 2 are fraction numbers) and the biologically effective dose (BED) derived from the LQ model (BED = D(1 + d/[α/β]), where D is the total dose and d is the fractional dose) are often used because of their convenience and simplicity [10, 27]. While LQ formalism is useful for conversion between relatively low radiation doses as used in conventional radiotherapy, it has been suggested that it is not applicable to higher daily doses or smaller fraction numbers [9, 10]. However, many clinicians have used LQ formalism to convert hypofractionated doses to single doses in their publications [28, 29], and many have used BED to evaluate the doses of stereotactic irradiation [30, 31]. To further complicate the issue, some investigators, in contrast, claim that the LQ model is applicable to stereotactic irradiation [32, 33]. The ground for the latter group is somewhat limited in that the existing clinical data do not significantly deviate from those expected from LQ model calculations, and their data do not necessarily indicate that the LQ model fits best to the high-dose data. Since clinical data usually contain many errors, experimental evaluation of the reliability of the LQ model in single-fraction and hypofractionated radiation schedules appears to be important and desirable.
(where d 1 and d 2 are fractional doses and n 1 and n 2 are fraction numbers) and the biologically effective dose (BED) derived from the LQ model (BED = D(1 + d/[α/β]), where D is the total dose and d is the fractional dose) are often used because of their convenience and simplicity [10, 27]. While LQ formalism is useful for conversion between relatively low radiation doses as used in conventional radiotherapy, it has been suggested that it is not applicable to higher daily doses or smaller fraction numbers [9, 10]. However, many clinicians have used LQ formalism to convert hypofractionated doses to single doses in their publications [28, 29], and many have used BED to evaluate the doses of stereotactic irradiation [30, 31]. To further complicate the issue, some investigators, in contrast, claim that the LQ model is applicable to stereotactic irradiation [32, 33]. The ground for the latter group is somewhat limited in that the existing clinical data do not significantly deviate from those expected from LQ model calculations, and their data do not necessarily indicate that the LQ model fits best to the high-dose data. Since clinical data usually contain many errors, experimental evaluation of the reliability of the LQ model in single-fraction and hypofractionated radiation schedules appears to be important and desirable.3.3.2 Cell Survival Data for the Reliability of the LQ Model at High Doses per Fraction
The theoretical basis behind the LQ model not being applicable with high doses per fraction is that dose-survival curves for cultured cells cannot be fitted well by the LQ model in high-dose ranges. This has been pointed out for a long time; in the pioneering work of Puck and Markus [34] who established the colony formation assay, the high-dose region of the dose-survival curve was apparently straight in HeLa cells. Therefore, the LQ model, with which the cell survival curve continues to bend downward at high doses, does not seem to fit the actual curves at high doses. Joiner and Bentzen [10] stated that extrapolations by the LQ model beyond 5–6 Gy per fraction are likely to lack clinically useful precision. More recently, Garcia et al. [35] investigated the compatibility of the LQ model regarding dose-survival curves of 4 cell lines in broad dose ranges. In the 4 lines, the LQ model did not fit the curves at very high dose ranges that were >7.5, 9.5, 11.5, or 13 Gy depending on the cell line. Therefore, the inadequacy of the LQ model at high doses was clearly demonstrated.
In a previous study, our group investigated the reliability of LQ formalism in converting hypofractionated doses (in 2–5 fractions) to single doses in single cells and spheroids in culture [36]. That study showed that LQ formalism is inadequate in doing so; the equivalent single doses for the hypofractionated doses calculated by LQ formalism were apparently lower than the equivalent single doses actually measured. LQ formalism underestimated the effect of fractionated irradiation. The magnitudes of errors were 6–19 % for 2- or 3-fraction schedules in cultured V79 and EMT6 single cells and 18–30 % for 2- to 5-fraction schedules in V79 spheroids. Since the reoxygenation of hypoxic tumor cells takes place in in vivo tumors between respective fractions [17, 37, 38], the compatibility of LQ formalism to single and hypofractionated radiation regimens was also investigated using murine tumors in the subsequent study.
Using EMT6 tumors, the applicability of LQ formalism for converting hypofractionated doses (in 2–5 fractions) to single doses was evaluated [39], as in the previous in vitro study. Again, the use of LQ formalism produced large errors; the equivalent single doses for the hypofractionated doses calculated from LQ formalism were much lower than the equivalent single doses actually measured. The magnitudes of errors were larger than those seen in the in vitro study; they were 21–31 % for 2- or 3-fraction schedules and 27–42 % for 4- or 5-fraction schedules. The possible larger discrepancy in in vivo tumors as compared to in vitro single cells and spheroids was considered to be largely due to the reoxygenation of hypoxic tumor cells during intervals between fractions in the hypofractionated groups. This study clearly showed that LQ formalism is inadequate for high-dose-per-fraction radiotherapy, especially in in vivo tumors.
To further evaluate the appropriateness of the BED concept in hypofractionated irradiation, we compared 2- to 5-fraction irradiation schedules simultaneously in the EMT6 tumors in Balb/mice [39]. Total doses of 18–30 Gy were given in 2–5 fractions to the tumor-bearing mice at 4-h intervals, and tumor cell survival was assessed employing an in vivo–in vitro colony assay, as in the previous experiment. Tumor cell survival was plotted against the total dose and BED3.5. In the in vitro cell survival determination conducted along with the in vivo experiment, the α/β ratio of the cell line was 3.5 Gy, so BED3.5 was adopted as a substitute for “BED10” often used clinically to represent the tumor response. Figure 3.7 shows tumor cell survival plotted against the total dose and BED3.5. Respective dose–response curves almost overlapped when cell survival was plotted against actual radiation doses. However, the curves tended to shift downward by increasing the fraction number when cell survival was plotted against BED3.5. If the BED concept is correct, the respective cell survival curves would overlap on this figure. Thus, it seems that BED is inadequate for use in this dose-per-fraction range, especially for tumors. The total dose reflected the actual effect (tumor cell survival) more accurately than BED in this experiment. The calculated BED tended to become larger than expected from the actual effects when the fraction number decreased. Thus, BED tends to overestimate the actual biologically effective dose with increasing radiation doses.