Case presentation
A 4-year-old male arrives via air ambulance after being involved in an all-terrain vehicle (ATV) accident. The child was riding with his older sister (he was in the front, riding on his sister’s lap) when the ATV turned over at a high rate of speed, causing the vehicle to flip onto the child. The ATV was pushed over by his father and several other witnesses to the accident and emergency medical services were called. The child was complaining of severe abdominal pain and had a Glasgow Coma Scale score (GCS) of 12. The accident occurred 1 to 2 hours by car from the nearest pediatric trauma center, so the decision was made to transport the child by air.
On arrival, he is alert and crying but consoles and tells you he has “tummy pain.” His vital signs are significant for a heart rate of 114 beats per minute, respiratory rate of 22 breaths per minute, and blood pressure of 95/65 mm Hg. He has diffuse abdominal tenderness with guarding and there is mild bruising to the right upper quadrant. His liver function tests are elevated: AST (aspartate aminotransferase) of 1721 U/L and ALT (alanine transaminase) of 1083 U/L.
Imaging considerations
Imaging is routinely employed in the evaluation of blunt abdominal trauma and its use is fairly routine in adult trauma victims. The role of imaging during the evaluation of abdominal trauma in the pediatric population, however, is somewhat controversial. Indeed, not all pediatric patients who sustain abdominal trauma require imaging. Several clinical decision tools have been devised to assist the clinician in determining which patients might have an intraabdominal injury , and benefit from imaging and which patients can forego computed tomography (CT) imaging safely, employing historical, clinical examination, and laboratory findings to render an imaging decision. Such decision rules do appear to reduce imaging use (specifically CT), reduce cost of care, and potentially reduce the risk of future cancer cases. , An example of one such decision rule is given below, devised by Streck et al., which takes into account five variables in patients with blunt abdominal trauma:
- 1.
AST >200 U/L.
- 2.
Abdominal wall trauma, tenderness, or distention.
- 3.
Abnormal chest x-ray.
- 4.
Complaint of abdominal pain.
- 5.
Abnormal pancreatic enzymes.
This study included almost 2200 children with a mean age of 8 years. Patients who were negative for all five variables had a 0.6% risk of intraabdominal injury and 0.0% risk of intraabdominal injury requiring intervention. Thus, this clinical prediction model had a negative predictive value of 99.4% for intraabdominal injury and 100.0% for intraabdominal injury requiring acute intervention in patients with none of the prediction rule variables present.
Plain radiography
This modality can be used to detect free abdominal air and associated pelvic fractures. However, plain radiography is not useful to visualize intraabdominal solid organ injury.
Ultrasound (US)
The use of US in the Focused Assessment with Sonography for Trauma (FAST) technique for routine adult abdominal trauma evaluation has been well documented and well supported, proving to be efficacious in detecting abdominal organ injury and useful in guiding management, including further imaging and operative repair. The advantages of sonography for the pediatric patient include a rapid examination time, general availability, and eliminating ionizing radiation exposure.
However, studies have shown FAST US to be less reliable in pediatric patients. A large meta-analysis of approximately 4000 patients that included both prospective and retrospective studies found a sensitivity of 66% and a specificity of 95% for FAST in the detection of intraabdominal solid organ injury in adult patients. , Other studies have found similar results. , In a recent multicenter study of children 16 years of age and less, FAST was shown to have a sensitivity for intraabdominal injury of 27% and a specificity of 91%; CT utilization rate among FAST and non-FAST groups was approximately the same; centers that performed FAST at a higher frequency did not have improved accuracy; and all patients who required intervention had abnormal physical examinations, including 15 children with negative FAST examinations. In another study, in hemodynamically stable children, the routine use of FAST compared to standard trauma care was not supported, as the rate of abdominal CT scans, time in the Emergency Department, hospital charges, or missed intraabdominal injuries was not improved in patients randomized to FAST versus those randomized to standard trauma care. Studies have sought to improve the low sensitivity associated with pediatric FAST examinations by utilizing liver function tests along with FAST. One study of approximately 3000 patients found that FAST alone produced low sensitivity (50%), but when combined with liver function testing, sensitivity improved to 88%. ,
An intriguing development is the use of intravenous contrast–enhanced US (IV CEUS). The use of IV CEUS greatly improves sensitivity in detecting intraabdominal solid organ injury, as compared to standard sonography. IV CEUS is operator dependent and not yet available in most centers in the United States. Currently, application appears most promising for hemodynamically stable children, with suspicion for solid organ injury from low-energy blunt abdominal trauma, or for follow-up imaging of known injuries. More investigation is needed with this imaging technique before this technique gains a wider application, but preliminary investigations seem promising.
The place of US in the evaluation of pediatric trauma is evolving. Notably, the American Academy of Pediatrics has released a guideline supporting the use of US as a diagnostic and procedural adjunct, promulgating effective training programs/curricula, credentialing, and quality control measures. , , For many pediatric emergency medicine fellowships, point of care US has become part of the training curricula, although implementation does vary. , Currently, though, use of abdominal ultrasonography as a sole imaging modality to reliably exclude intraabdominal injury is not supported.
Computed tomography
The American College of Surgery Advanced Trauma Life Support manual states that CT should be used in hemodynamically stable children only when necessary, but there is a lack of specific guidelines in this regard. CT exposes children to ionizing radiation that has the potential to cause adverse effects later on in life. This modality is excellent at identifying intraabdominal injury. The clinician should keep the following in mind:
- 1.
Utilize CT only when necessary (i.e., study results will impact management decisions).
- 2.
Practice gentle imaging (i.e., As Low As Reasonably Achievable [ALARA] principles).
- 3.
Avoid “pan-scanning” in pediatric patients. While this technique is utilized frequently in adult trauma patients, it exposes pediatric patients to unnecessary radiation with little impact on clinical management or outcomes.
A significant percentage of pediatric patients have required repeat imaging of the same body part at a pediatric trauma center after initial imaging at a referring hospital, increasing radiation dose to the patient. If CT is utilized prior to transfer to a pediatric trauma center, the study should be done with intravenous (IV) contrast and using proper technique to avoid the need to repeat a poor study.
Magnetic resonance imaging (MRI)
This modality is currently not considered a first-line test for pediatric abdominal trauma. There is scant literature describing the role of MRI in pediatric patients with blunt abdominal trauma. There are case reports of MRI use in adult patients with abdominal trauma. , An initial study demonstrated that noncontrast MRI offered no advantage to contrast-enhanced CT imaging in the diagnosis of solid organ injury, and another study reported IV contrast–enhanced MRI was comparable to CT for evaluating blunt abdominal trauma.
However, there are instances where MRI may prove useful. Patients with a previously documented severe reaction to iodinated IV contrast, patients with decreased renal function, pregnant patients, or patients in whom CT or other imaging modality results are indeterminant may be candidates for MRI. What role MRI can or will play in the evaluation of blunt pediatric trauma remains undetermined at this time.
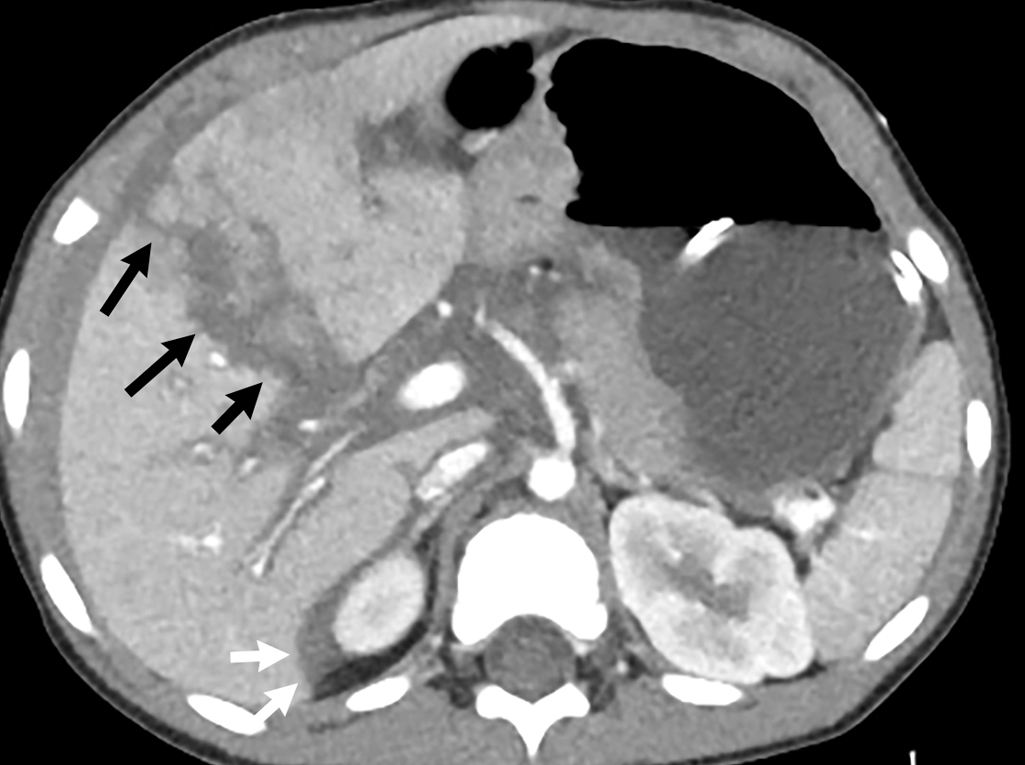
Imaging findings
Given the history and physical examination, IV contrast–enhanced CT of the abdomen and pelvis was performed. Thoracic and lumbar spine image reconstructions were also obtained. CT demonstrates a hepatic laceration extending from the anterolateral liver margin to the liver hilum, with perihepatic hemorrhage ( Fig. 41.1 ). The degree of injury is consistent with a grade IV liver laceration. On the early phase images, there is a 2-cm lobulated high attenuation area at the site of injury, which increases in size on delayed phase imaging, consistent with active contrast extravasation due to active bleeding ( Figs. 41.2 and 41.3 ).