George M. Bridgeforth and Mark Nolden
A 21-year-old man falls 30 ft down an elevator shaft without losing consciousness. he reports some problems with sensation and motor function below the waist.

CLINICAL POINTS
- Burst fractures are caused by axial loads (downward forces).
- Neurological impairment may occur as a result of burst fractures.
- Cervical axial load injuries may be associated with traumatic brain injuries.
- Thoracolumbar injuries may be associated with abdominal trauma.
- Numbness and weakness occurs at and below the level of the spinal cord injury.
- Bladder, bowel, and sexual impairment may result.
Clinical Presentation
Burst fractures are traumatic spinal injuries that involve vertebral breakage. They may occur as a result of cervical injuries from diving accidents or from rollover accidents in which the driver was not wearing a seat belt. The mechanism of injury involves an axial load impact against a rock or a shallow river or against the roof of a vehicle as it rolls over. Cervical burst fractures may also be seen in contact sports injuries—in football, from an illegal technique called “spearing,” in which the top of the helmet is used as a weapon during a flying block or a tackle.
As expected, impact injuries to the cervical spine may be associated with traumatic brain injuries. Therefore, the neurological examination should document any associated head trauma. Computed tomography (CT) scans of the cervical region and the head are indicated. Patients with severe neurological damage from cervical may present obtunded and in spinal shock. Severe cervical injuries may result in permanent tetraplegia (quadriplegia) once the patient recovers from spinal shock within 48 to 72 hours. A Jefferson fracture is a burst fracture of the first cervical ring (vertebrae). These fractures are usually fatal.
Burst fractures caused from falls in which the heels or buttocks strike the ground first may cause damage to the lower thoracic to upper lumbar vertebrae. Usually these occur between T10 and L2, but burst fractures as low as L5 have been reported. Patients with cervical or thoracolumbar burst fractures may fall into any one of the five American Spinal Injury Association (ASIA) spinal injury groups (see Chapter 4). Signs of an unstable burst fracture include acute neurological impairment, kyphosis (forward angulation of the spinal column greater than 20 degrees), acute subluxation (dislocation of the spinal column), and a 50% or greater encroachment of the spinal canal. A complete neurological examination, initial radiographs, and a CT scan are used to assess stability. The comprehensive neurological assessment should be conducted while the patient has been immobilized on a spine board with a hard cervical collar. It is important to examine the patient for other traumatic injuries to the major organs as well.
Severe thoracolumbar injuries may present acutely with loss of motor and sensory function below the umbilicus (T10 level). Severe thoracolumbar injuries may result in permanent paraplegia. Falls during which the patient lands feet first are associated with unilateral or bilateral heel fractures (10% of heel fractures are bilateral). Complete paraplegics with acute spinal cord injuries lose lower extremity sensation, so the presence of any bruising or swelling of the heels warrants radiographic analysis of the affected foot or feet. However, patients with normal neurological function manifest heel pain unless they are obtunded from a traumatic brain injury, drug, or alcohol intoxication. Ten percent of calcaneal fractures from falls are bilateral.
PATIENT ASSESSMENT 
- Check for neurological impairment.
- Always check for bilateral calcaneal injuries from falls.
- Always assume spinal instability until proven otherwise. Patients with severe trauma should be immobilized in a hard cervical collar and on a spine board.
- Always check neurovascular status carefully.
Radiographic Evaluation
Tests to order, depending on the type and severity of the trauma, include the following:
- Acute cervical trauma (minor): anteroposterior (AP), lateral (must be able to see the C7-T-1 interspace vertebrae), and oblique radiographs. A swimmer view is used to visualize the C7 vertebrae if it is not identified on the lateral projection. An odontoid view (open mouth view), used to evaluate fractures of the odontoid process, is also necessary. Flexion/extension views should be read only by experienced spinal care providers. Flexion and extension radiographs are never taken until the initial radiographs have been evaluated first (Fig. 5.1).
- Acute thoracolumbar trauma (minor): AP, lateral, and oblique radiographs (two oblique views). Flexion and extension radiographs should be taken only if necessary.
- Acute cervical and thoracolumbar trauma (severe): CT scan “stat”
Burst fractures are comminuted dispersion fractures of the vertebral body; they are caused by an axial load. Unlike wedge compression fractures, which are limited to the anterior column of Denis, burst fractures are characterized by a comminuted fracture involving the anterior and the middle columns of Denis. The comminuted fractures may be identified on an AP view as compressed vertebrae. In addition to the decreased vertebral height, there is an outward dispersion of the vertebral fragments. This dispersion is characterized by an increase in the interpedicular space (a horizontal measurement taken from pedicle to pedicle in a single vertebra).
On the lateral view, the examiner can identify a comminuted fracture of the entire vertebral body. Unlike wedge compression fractures, which affect mainly the anterior column of Denis, the examiner should look for flattening and dispersion of the entire vertebral body with retropulsion posteriorly of the middle column (Fig. 5.2). This retropulsion is one of the hallmarks of a burst fracture. In contrast, a wedge compression fracture involves the anterior half to two-thirds of the vertebral body, and there is no evidence of retropulsion of the bony fragments seen on the lateral view. However, if there is anterior and middle column involvement characterized by a dispersed comminuted fracture, one must suspect a burst fracture. The lateral projection shows a comminuted fracture of the entire vertebral body. Associated findings include a decreased vertebral height associated with an increased distance from the anterior to the posterior vertebral body.
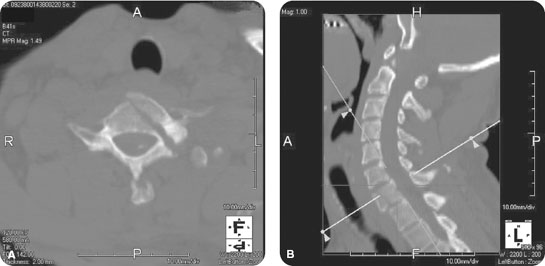
FIGURE 5.1 While tubing in the Atlantic Ocean, a 48-year-old man is swept into the sand by a wave. (A) Sagittal reformatted image of the cervical spine. (B) Maximum intensity projection image through the C7 vertebral body, demonstrating an acute burst fracture.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








