George M. Bridgeforth and Mark Nolden
A 42-year-old restrained female passenger presents with back and chest pain after a motor vehicle collision, which took the life of her 4-year-old child.

CLINICAL POINTS
- This compression injury is caused by violent forward flexion.
- Once known as the “seat belt injury,” this fracture is now less common.
- Survivors usually have paraplegia, with lower motor neuron damage to the bowel and bladder.
- Other serious injuries to the abdominal organs (ruptured liver, spleen, aorta, kidneys) may occur.
Clinical Presentation
Chance fractures are uncommon injuries, and they have become even less likely since the introduction of combination shoulder strap-lap seat belts. In older vehicles, where the seat belt does not include a shoulder strap, and in an accident, the patient can be thrown forward against the seat belt, which functions like a restraining fulcrum. As the patient
is thrown forward and upward, there is a disruption of the spinal column through all three columns of Denis. The mechanism of injury is flexion distraction. The majority of injuries affect the lower thoracic to upper lumbar vertebrae. Ligamentous injuries may be seen, especially if there is an associated rotational component to the injury. Surprisingly, neurological injuries are uncommon and occur in approximately 15% of cases. Usually, these injuries are characterized by a paraplegia below T10 level (the umbilicus) or a cauda equina injury.
Individuals with complete T10 paraplegia (American Spinal Injury Association [ASIA] class A) present with a total loss of neurological function below the umbilicus (navel). This includes a complete loss of motor function, total sensory loss, and loss of sexual, bowel, and bladder function.
Individuals with an incomplete spinal cord injury (T10 paraplegia [ASIA class B]) have a loss of motor function but intact sensory function, which includes the sacral segments. This would be a very unusual level but sensation of the legs and perianal sensation would be intact. Impaired sexual function and bowel and bladder incontinence are still present.
Individuals with an incomplete spinal cord injury (T10 paraplegia [ASIA class C]) have motor weakness of the lower extremities (with less than 50% of the key muscles having a grade less than 3/5). Once again, there is accompanying impaired sexual, bowel, and bladder function.
Individuals with an incomplete spinal cord injury (T10 [ASIA class D]) would exhibit functional motor strength in the lower extremities (at least 50% of the muscles or more would exhibit grade 3/5 or stronger motor function). However, these injuries may still be accompanied by impaired sexual, bowel, and bladder function.*
PATIENT ASSESSMENT 
- Assess carefully for neurovascular compromise (loss of pulses, cold cyanotic limbs).
- Assess for other abdominal organ injuries (aortic tears, as well as liver, kidney, and spleen damage).
- Look for bruising of the abdomen and the chest wall.
Individuals with acute cauda equina injuries present with mixed picture of upper motor neuron (injury to the central nervous system) and lower motor neuron (injury to nerve roots and peripheral nerves). There may be acute traumatic low back pain with an asymmetrical motor and sensory impairment of the lower extremities. There is an acute loss of voluntary bowel tone on a rectal examination (i.e., patients cannot generate a forceful tone when they bear down). In addition, there is perianal saddle anesthesia, which is characterized by a loss of sensation to pinprick in the gluteal region surrounding the anus. In addition, there is a loss of the anal wink reflex (i.e., a contraction of the anal sphincter that occurs when the anal rim is stroked with a cotton swab). Acute spinal core injuries to the lower thoracic and lumbar regions (or acute cervical injuries with spinal shock) are initially characterized by similar findings (saddle anesthesia, loss of voluntary bowel tone, loss of the anal wink reflexes); however, an asymmetrical motor sensory impairment of the lower extremities leads the examiner more toward a cauda equina injury.
As expected, the rate of associated abdominal injuries is high—reported to be 50% or more. There may be associated damage to the aorta, liver, spleen, uterus, thoracic ribs, diaphragm, or kidneys. Therefore, a surgical consultation and a computed tomography (CT) of the abdomen (or possibly the head) are indicated.
Radiographic Evaluation
It is necessary to obtain the following tests:
- Lateral and anteroposterior radiographs of the spine
- CT scans for acute thoracolumbar trauma (severe)
- Abdominal CT
- Head CT (if the patient is acutely intoxicated, has an associated injury above the clavicle, or has an impaired mental status)
- Spinal CT with sagittal reconstructions (Fig. 6.1).
- Abdominal CT
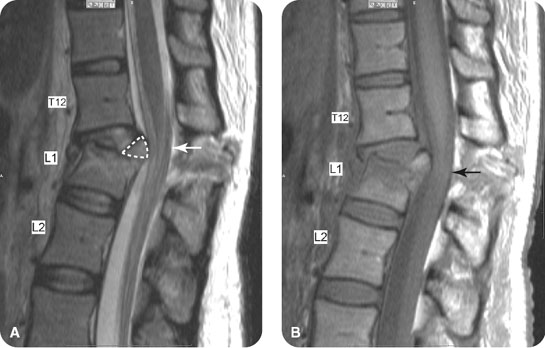
FIGURE 6.1 (A) Sagittal T1-weighted and (B) T2-weighted magnetic resonance images of a 51-year-old man involved in a serious motor vehicle accident, demonstrating the Chance fracture at L1 and the superior retropulsion causing posterior displacement of the cauda equina.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








