Case 1 presentation
A 14-year-old male presents with a complaint of acute right hip pain. The patient is an avid soccer player and was kicking a ball “pretty hard.” Immediately upon full extension of the right leg, he felt a “pop.” Thereafter, he began to experience pain that was radiating to the right upper thigh. He was unable to continue the game. He denies other injury and denies numbness or weakness involving the right leg.
His physical examination reveals appropriate-for-age vital signs. He weighs 59 kg (body mass index of 18.7—normal for his height of 180 cm). He has a completely unremarkable examination, with the exception of his right hip. He has mild tenderness to palpation of the anterior superior iliac spine. While he has full range of motion of the right leg at the hip joint, flexion and extension produce pain. He has no spine tenderness, deformity, or crepitus. He is able to ambulate but does so with a slight limp. There is no lower extremity tenderness, swelling, deformity, or crepitus. He is grossly neurovascularly intact.
Imaging considerations: Low-energy mechanisms
Imaging is often employed in the evaluation of children with musculoskeletal complaints, including hip issues, although not all patients require radiographic testing. A thorough history and physical examination can help identify which patients would benefit from imaging.
Plain radiography
This modality is the initial test of choice for the majority of patients in whom imaging is indicated. Previous studies have shown plain radiography to be generally effective in identifying pelvic avulsion fractures. , In a large study of 228 patients with pelvic avulsion fractures, 99% were identified by plain radiography; only two patients required advanced imaging (such as computed tomography [CT] or magnetic resonance imaging); fracture displacement and fracture size were identified in 90% and 97% of cases, respectively. , Patients with acute onset of pain or pain that is continuous, not improving, or worsening should have plain radiography performed. ,
Ultrasound (US)
The use of US to detect fractures is controversial. Studies have indicated US as an effective imaging modality for the identification of hip avulsion fractures, , but other studies have not supported these findings, especially when compared to more advanced imaging modalities. , US may show a widened physis on the injured side, compared to the nonaffected side. US can also detect nondisplaced or minimally displaced fractures, which may be difficult to see radiographically. ,
US is attractive because of the lack of ionizing radiation and general availability, but expertise is required to obtain a meaningful study and interpret the images obtained.
Computed tomography
CT is not a first-line imaging modality when there is a low-energy mechanism or an avulsion fracture is suspected. CT may be employed as a secondary imaging modality when plain radiography does not reveal a fracture but clinical suspicion for a fracture remains high.
This modality is often employed when a patient is involved in a high-energy mechanism, such as a motor vehicle accident or significant fall and is typically part of an abdomen/pelvis study for trauma (see later, “High Energy Mechanisms”).
Magnetic resonance imaging (MRI)
Persistent or worsening symptoms may warrant advanced imaging with MRI, particularly if other imaging modalities have not demonstrated any abnormal findings. As such, this modality is generally not a first-line imaging test in the emergent setting.
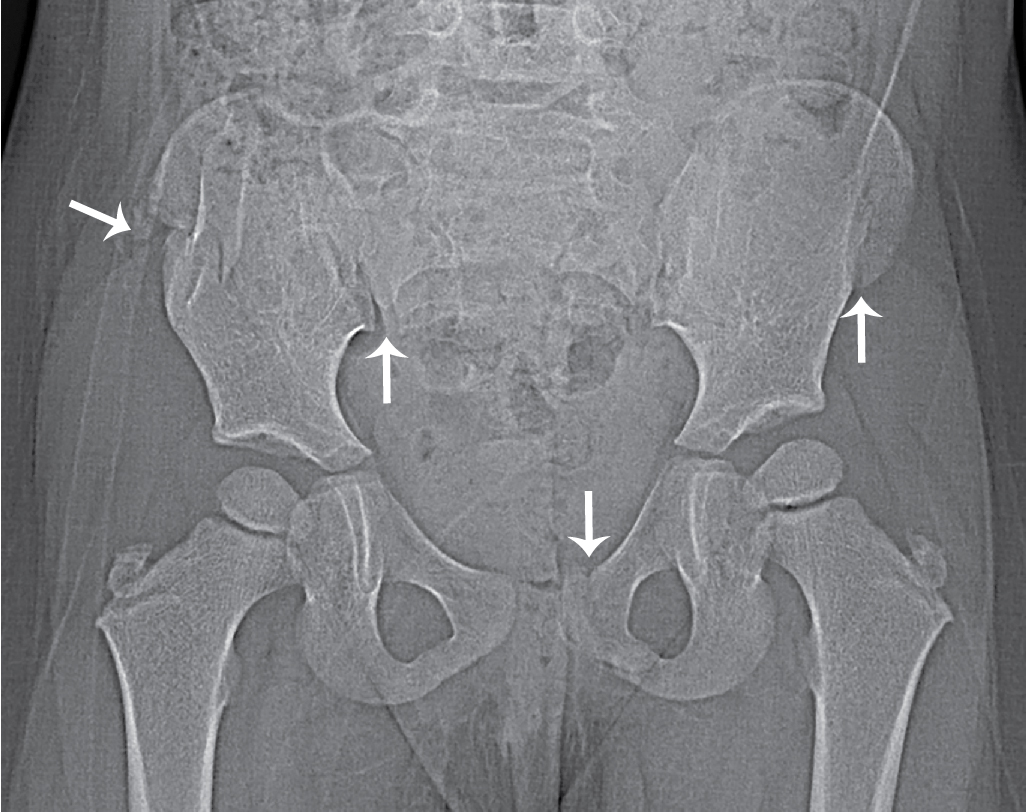
Case 1 imaging findings
Plain radiographic imaging of the pelvis was obtained, including anteroposterior and frog leg views. It is helpful to obtain a full view of the pelvis, rather than a hemipelvis view, as both right and left sides can be visualized together. An avulsion fracture is seen at the right anterior superior iliac spine. There is no dislocation and no signs of a slipped capital femoral epiphysis ( Figs. 63.1 and 63.2 ).


Case 1 conclusion
Pediatric Orthopedics was consulted and they recommended discharge with non–weight-bearing instructions, crutch use, and supportive care. Follow-up was arranged with the Pediatric Orthopedic Clinic. Operative intervention was not required.
Pediatric pelvis apophyseal avulsion fractures are commonly related to adolescent sports activity, especially soccer, football, and gymnastics and are the result of a forceful contraction through muscle-tendon unit and bone interaction, at the cartilaginous growth plate. , The most common locations for this injury include the anterior inferior iliac spine, the anterior superior iliac spine, the ischial tuberosity, and insertion of the hamstring. , , It is common for patients with this injury to report a sudden “crack” or “pop” in the hip, followed by pain, and such symptoms should raise suspicion for this injury when reported. History and physical examination are important to help distinguish an avulsion fracture from other causes of hip pain that may produce similar symptoms, as treatment differs according to the underlying etiology. The sudden onset of the pain while engaged in sports activity points to a musculoskeletal etiology; fever is suggestive of an infectious etiology; and chronic pain is suggestive of an overuse injury or apophysitis.
Plain radiography is usually diagnostic for hip avulsion fractures, showing the fracture fragment and any displacement. , This is particularly true for avulsion fractures of the ischial tuberosity, but some fractures, such as that of the anterior inferior iliac spine, may be difficult to visualize on an anterior-posterior (AP) view and may require either additional views or advanced imaging for visualization. ,
The majority of patients with pelvic avulsion fractures are treated conservatively, with nonoperative management, although which fractures require operative treatment is a matter of some controversy. , , , The site of the fracture, grade of displacement, and athlete preference can be taken into account when a treatment plan is considered, which may involve rest and nonsteroidal antiinflammatory drug use, with gradual return to weight bearing and activity, along with physical therapy exercises. , , , Some authors recommend conservative treatment for minimally displaced fractures and operative intervention for fractures with greater than 15–20 mm displacement, or patients with persistent symptoms or activity limitations. , , Whether operative intervention allows a patient to return to normal activity sooner is debated in the literature. It is appropriate to consult pediatric orthopedics for treatment recommendations and to arrange appropriate follow-up.
Complications due to hip avulsion fractures arise when these injuries are not identified. A patient with a hip avulsion fracture who undergoes stretching exercise and/or physical activity risks further displacement of the fracture fragment and nonunion. , Ischial tuberosity fractures have a higher risk and rate of nonunion. , Displacement of more than 20 mm has shown to increase the likelihood of nonunion by 26 times. Widely separated fracture fragments will heal but have been associated with persistent/chronic pain, instability and sports activity limitations, culminating in disability. ,
High-energy pediatric pelvic fractures
In contrast to pelvic avulsion fractures, high-energy pediatric pelvic fractures are not common and are usually the result of motor vehicle collision (MVC), often the result of being struck by a motor vehicle as a pedestrian; the location of impact is typically the side of the body. , These fractures themselves are typically not life-threatening but may be associated with other injuries, such as head or abdominal trauma, which may be life-threatening. Injury patterns are related to the age of the child, since initially, the pelvic ring is more cartilaginous, the periosteum is thicker, and the sacroiliac and other pelvic joints are wider and thicker, allowing the child to absorb more force compared to an adult. Over time, injury patterns become more like an adult as the child’s pelvic structures mature. Also, unlike adults, children who sustain pelvic fractures have an overall lower mortality and less significant hemorrhage. , ,
Imaging considerations: High-energy mechanisms
The decision facing the clinician when evaluating high-energy pelvic injuries is whether to employ plain radiography or CT. Additional consideration should be given to whether screening plain radiographs are effective or indicated in pediatric patients.
Plain radiography
The overall sensitivity of pelvic radiographs for detecting pelvic fractures has been found to be 54% to 78%. , Routine pelvic radiography is commonly obtained in adult trauma patients. , Routine radiography may not be indicated in all pediatric patients, however. Studies have sought to identify factors to risk stratify patients who might need radiography. One study reported a screening tool combining eight high-risk clinical findings (pelvic tenderness, laceration, ecchymosis, abrasion, Glasgow Coma Scale score <14, positive urinalysis, abdominal pain/tenderness, femur fracture) and five high-risk mechanisms of injury (unrestrained MVC, MVC with ejection, MVC rollover, auto vs. pedestrian, auto vs. bicycle) to be effective in ruling out (but not detecting) pelvic fractures in pediatric patients. Children with major trauma who did not have any of these high-risk criteria may safely forego pelvic imaging. Another study reported that pelvic contusions and abrasions, hip/pelvic pain, abdominal pain and distension, back pain, the hip held in rotation at presentation, and femur deformity/pain were independently predictive of pelvic fracture, which were helpful in determining the need for pelvic radiography. One study found that the lack of lower extremity injury, lack of an abnormal physical examination of the pelvis, and no need for abdominopelvic CT can exclude pelvic fracture and obviate the need for imaging. Some authors recommend no imaging in patients with no or low suspicion of pelvic fracture or intraabdominal injury based on mechanism and physical examination and a screening pelvic radiograph (AP) view in patients with suspicion for pelvic fracture injury but in whom CT is not indicated. , ,
Computed tomography
Although CT has been reported to be more sensitive in detecting pelvic fractures, the routine use of CT for pelvic fracture evaluation is not recommended. , Studies have reported pelvic fractures that were identified by plain radiographs and CT found no difference in classification and management of the fractures, suggesting that most pediatric pelvic fractures can be managed based on plain radiography findings. ,
CT is indicated if there is suspected instability, significant disruption, or when posterior ring disruption is suspected based on plain films. Acetabular fractures should be evaluated with CT imaging as well. If a patient requires CT to evaluate intra-abdominal injury, then the pelvis will be adequately visualized, obviating the need for plain pelvic radiography.
Magnetic resonance imaging
This modality is not a first-line imaging modality in pediatric trauma patients. MRI has been noted to be useful in the evaluation and treatment planning of fractures in which plain radiography or CT underestimate the extent of injury.
Case 2 presentation
Presented here are selected images from a 4-year-old child involved in a high-speed motor vehicle accident. The child was a backseat passenger and was not restrained. She had complaints of abdominal pain and mild tenderness throughout. An initial pelvis x-ray revealed multiple fractures ( Fig. 63.3 ). Due to the apparent complexity of the fractures noted on plain imaging, a CT scan was ordered. Interestingly, no liver, spleen, or apparent bowel injuries were identified and the child had normal AST (aspartate aminotransferase) and ALT (alanine transaminase) values. Selected imaging from the CT is presented here. There is a comminuted fracture of the anterior aspect of the right iliac bone with buckling of the iliac wing and several adjacent small fracture fragments; there is a mildly displaced, minimally comminuted fracture through the anterior aspect of the left iliac wing; there is a mildly displaced fracture through the pubis just to the left of the symphysis extending caudally through the ischiopubic ramus ( Figs. 63.4–63.6 ).